Noninvasive, nonionizing, multiparametric magnetic resonance (MR) imaging of the pelvis using a field strength of 3 T now provides a comprehensive assessment of perineal involvement in pediatric Crohn disease. MR imaging accurately evaluates inflammatory disease activity, and allows determination of the number and course of fistula tracts as well as their relationships to vital perianal structures, including the external anal sphincter, helping to guide surgical management and improve outcomes. This article provides an up-to-date review of perineal MR imaging findings of Crohn disease in the pediatric population, including fistulous disease, abscesses, and skin manifestations. Imaging technique is also discussed.
Key points
- •
High-resolution, especially at 3-T, magnetic resonance (MR) imaging with a small field of view allows comprehensive evaluation of the perineum in pediatric Crohn disease, including assessment of the perianal, labial, and scrotal regions.
- •
Crohn disease–related perianal fistulas (including complex fistulous disease) and associated abscesses, as well as cutaneous inflammation, are exquisitely depicted by MR imaging.
- •
Other imaging modalities (such as fluoroscopic fistulography, endoscopic and transperineal ultrasonography, and computed tomography) and physical examination can provide useful information about perineal Crohn disease; however, they frequently do not depict the true extent of perineal and pelvic inflammation as well as does MR imaging.
- •
MR imaging findings predict outcomes in perineal Crohn disease better than other imaging modalities and physical examination.
- •
MR imaging improves surgical outcomes in perianal fistulous disease by alerting surgeons to exact anatomic relationships and true extent of disease.
Introduction
Crohn disease (CD) is one type of chronic inflammatory bowel disease (IBD) affecting both children and adults that can involve any portion of the gastrointestinal tract from the mouth to the anus. This condition can also affect a variety of extraintestinal structures and body systems, including the perineum and skin. The initial diagnosis of IBD is made approximately 20% to 30% of the time during childhood, with a pediatric prevalence of 5 to 16 cases per 100,000 children. Perianal and perineal cutaneous inflammatory involvement in the setting of IBD occurs almost exclusively with CD (rather than ulcerative colitis) and has been reported to occur in 13% to 49% of pediatric CD patients. In a small number of children with CD (up to about 4%), perineal and cutaneous inflammation may become evident before detection of bowel involvement. Cutaneous inflammatory involvement by pediatric CD very commonly affects the perineal region (perianal, labial, and scrotal regions), presenting as fistulas and fissures, associated abscesses, uncomplicated skin inflammation, and skin tags.
Recent advances in magnetic resonance (MR) imaging have transformed the clinical and operative management of pediatric CD patients. MR enterography allows for dedicated nonionizing, high-quality imaging of the bowel and can detect inflamed intestinal segments characterize inflammatory disease activity, and diagnose a variety of disease-related complications, such as strictures and internal fistulas. High-resolution, small field-of-view MR imaging of the perineum, particularly at a field strength of 3-T, provides for nonionizing, multiparametric evaluation of the perianal, labial, and scrotal regions in a noninvasive manner, and allows for definitive assessment of perineal and pelvic inflammation in pediatric CD. This article provides a contemporary review of perineal MR imaging appearances of CD in the pediatric population, including fistulous disease, abscesses, and skin manifestations. The perineal MR imaging technique is also discussed.
Introduction
Crohn disease (CD) is one type of chronic inflammatory bowel disease (IBD) affecting both children and adults that can involve any portion of the gastrointestinal tract from the mouth to the anus. This condition can also affect a variety of extraintestinal structures and body systems, including the perineum and skin. The initial diagnosis of IBD is made approximately 20% to 30% of the time during childhood, with a pediatric prevalence of 5 to 16 cases per 100,000 children. Perianal and perineal cutaneous inflammatory involvement in the setting of IBD occurs almost exclusively with CD (rather than ulcerative colitis) and has been reported to occur in 13% to 49% of pediatric CD patients. In a small number of children with CD (up to about 4%), perineal and cutaneous inflammation may become evident before detection of bowel involvement. Cutaneous inflammatory involvement by pediatric CD very commonly affects the perineal region (perianal, labial, and scrotal regions), presenting as fistulas and fissures, associated abscesses, uncomplicated skin inflammation, and skin tags.
Recent advances in magnetic resonance (MR) imaging have transformed the clinical and operative management of pediatric CD patients. MR enterography allows for dedicated nonionizing, high-quality imaging of the bowel and can detect inflamed intestinal segments characterize inflammatory disease activity, and diagnose a variety of disease-related complications, such as strictures and internal fistulas. High-resolution, small field-of-view MR imaging of the perineum, particularly at a field strength of 3-T, provides for nonionizing, multiparametric evaluation of the perianal, labial, and scrotal regions in a noninvasive manner, and allows for definitive assessment of perineal and pelvic inflammation in pediatric CD. This article provides a contemporary review of perineal MR imaging appearances of CD in the pediatric population, including fistulous disease, abscesses, and skin manifestations. The perineal MR imaging technique is also discussed.
Perianal anatomy
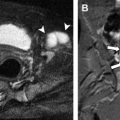
Understanding the anatomy of the perineum and perianal region is necessary to properly interpret imaging of these areas and to appropriately direct clinical and surgical care ( Figs. 1 and 2 ). The internal anal sphincter (IAS) is a smooth muscle layer that encircles the anal canal and provides a majority of resting anal tone, although it is not necessary for maintenance of bowel continence. The external anal sphincter (EAS) is composed of striated muscle and is located peripheral to the IAS. It provides voluntary muscle contraction and a small amount of resting anal tone; disruption of the EAS can result in bowel incontinence. The EAS attaches to the perineal body anteriorly and the anococcygeal ligament posteriorly, and is continuous with the puborectalis muscle and the levator ani musculature superiorly. The IAS and EAS are separated by a layer of loose connective tissue commonly referred to as the intersphincteric space (or plane), which represents a potential space for fistula passage and infection. Lateral to the EAS is the contiguous spaces of the ischioanal fossa and ischiorectal fossa, which contain mostly fat as well as inferior rectal vessels and nerves.
Description of the location of perianal abnormality in the axial (transverse) plane commonly makes use of the “anal clock” (see Fig. 2 ). When using anal-clock nomenclature, the patient is supine (in the lithotomy position) and the physician is presumed to be standing at the patient’s feet looking at the perineum. The anterior (toward the perineal body) and posterior (toward the intergluteal cleft) positions are represented by 12 o’clock and 6 o’clock on the clock face, respectively. The left (patient left) lateral position is represented by 3 o’clock, and the right (patient right) lateral position is represented by 9 o’clock.
Classification and management of perianal fistulous Crohn disease
The EAS joins the puborectalis muscle at the level of the dentate (or pectinate) line, a point about 2 cm deep to the anal verge where squamous epithelium transitions to columnar epithelium. At this location, longitudinal columns of mucosa (columns of Morgagni) are present with intervening anal sinuses (or crypts), which collect drainage from the anal glands. Obstruction and infection of the glands at this location has been hypothesized to be the cause of most idiopathic abscesses and fistulas in the “crypto-glandular hypothesis” described by Parks in 1961. However, in the setting of CD, the development of perineal inflammation and infection is more complex as other routes of inflammation and infection are possible, including extraintestinal granulomatous inflammation arising primarily in the perineal skin/soft tissues, or contiguous extension of inflammation from affected bowel directly to the perineum.
Based on extensive clinical experience in adults with fistula-in-ano, Parks and colleagues developed a novel classification system for describing perianal fistulas that is still used by surgeons today. This classification system more recently has been applied to both fistulas and abscesses arising in CD patients ( Fig. 3 ). Although variations exist, this classification scheme has 4 major groupings based on anatomic location of the fistula:
- •
Type 1: Intersphincteric. Fistula crosses the IAS and extends only within the intersphincteric plane
- •
Type 2: Transsphincteric. Fistula traverses both the IAS and EAS, and extends into the ischioanal fossa
- •
Type 3: Suprasphincteric. Fistula extends superiorly within the intersphincteric space and over the top of the puborectalis muscles, then traverses the levator ani musculature and extends downward to the ischioanal fossa
- •
Type 4: Extrasphincteric. Fistula extends from the deep pelvis (high perirectal region) through the levator ani and into the ischioanal fossa without involving the EAS complex
Knowledge of the type of fistula and the anatomic structures involved has been shown to be crucial for proper surgical planning and good postoperative outcomes in adults. A type 1 (intersphincteric) fistula is the simplest form, and can be treated surgically by dividing the IAS (fistulotomy or fistulectomy) with very low associated risk of subsequent loss of bowel continence. More complex fistula types (types 2, 3, and 4) usually necessitate an operation involving the EAS complex for complete excision, which increases the chances of bowel incontinence. To avoid a loss in bowel control, alternative surgical therapies, such as seton stitch placement that promotes healing by keeping the fistula tract patent for drainage of infectious material, may be used; such alternative techniques are often preferred in CD patients because of the presence of complex fistulous disease (eg, multiple or branching fistula tracts) and an increased risk of local recurrence after operations involving the EAS. Rarely, diversion of the fecal stream with ostomy formation may be required to promote healing of perianal CD.
Referring physicians can often visualize fistula tracts that extend to the skin surface. By performing a digital rectal examination and probing the tract, commonly under sedation or general anesthesia, the course of a fistula tract can sometimes be established. Clinical parameters also have been developed to characterize perianal fistulas, such as the perianal disease activity index (PDAI), which evaluates a fistula for discharge, pain, restriction of activity, type of recurrent disease, and extent of disease. Physical examination and clinical evaluation, however, often do not detect blind-ending tracts, secondary tracts, abscesses, and extension into the deep pelvis, and therefore may underestimate the true extent of perianal inflammatory activity. Detection of such occult perineal CD manifestations directly affects patient management. Proper clinical (both medical and surgical) decision making requires precise knowledge of the true extent of disease. Such knowledge, which is now provided by high-resolution, small field-of-view perineal MR imaging, can establish the feasibility and efficacy (at follow-up) of medical management (eg, treatment with immunomodulator and/or biological therapies, which can be associated with serious side effects) as well as determine which patients will benefit from surgery.
Imaging of perineal Crohn disease
Multiple imaging modalities have been used to evaluate for the presence and extent of perianal CD. Fluoroscopic fistulography was used in the past, but was often difficult to interpret, as the anal sphincter complex cannot be directly visualized and some fistula tracts or abscesses may not fill with injected contrast material. Endoscopic and transperineal ultrasonography have been used and can provide useful results, although the full extent of inflammation, particularly involving the EAS and deeper structures, may not be visualized owing to the lack of sound-wave penetration. The limited soft-tissue contrast resolution of computed tomography (CT) makes distinguishing perineal musculature, fibrous tissue, and fistula tracts potentially difficult, although organized fluid collections larger than about 1 cm in size generally can be readily seen. The availability of other imaging modalities that do not require ionizing radiation also makes CT imaging less desirable in this patient population, as repeat imaging is often required during the course of treatment. Recently, MR imaging has emerged as an ideal modality for assessing perineal CD. High-resolution, small field-of-view MR imaging of the perineum at a field strength of 3-T provides images with excellent spatial resolution and contrast resolution, enabling comprehensive evaluation of the entire perineum (perianal, labial, and scrotal regions) and lower pelvis.
Perineal MR Imaging Technique
The authors presently perform perineal MR imaging exclusively at a field strength of 3-T if there is no contraindication (eg, certain implanted devices that have been demonstrated to be safe at a field strength of 1.5-T only). 3-T MR imaging systems offer increased signal-to-noise ratio (SNR) when compared with 1.5-T systems, allowing for shorter image acquisition times and/or improved spatial resolution. A multielement torso surface coil is placed over the patient’s pelvis and upper thighs anteriorly. Parallel imaging can be used to reduce scan times, although care must be taken not to noticeably diminish the SNR. In the authors’ experience, the known disadvantages of 3-T MR imaging rarely adversely affect the diagnostic quality of perineal examinations. However, on occasion, air adjacent to the perineum may cause localized susceptibility artifacts or inhomogeneous fat suppression. Endorectal coils are generally avoided in pediatric perineal MR imaging because of safety concerns, their invasive nature, and the small field of view afforded.
The authors’ perineal MR imaging protocol comprehensively assesses the perineum and lower pelvis from the skin surface through the mid-to-upper rectum in the transverse plane. Coronal and sagittal images generally extend from the iliac crests through the perineal skin. Perineal MR imaging is most often performed without associated MR enterography pulse sequences, and therefore requires no specific patient preparation (other than peripheral intravenous catheter placement) if the examination is to be performed without sedation. In patients undergoing MR enterography with known or suspected perineal CD, limited high-resolution, small field-of-view imaging (eg, axial and sagittal T2-weighted fast spin-echo with fat saturation, and postcontrast T1-weighted 3-dimensional spoiled gradient recalled echo [3D-SPGR] with fat saturation in 3 planes) may be acquired. Our routine clinical perineal MR imaging protocol is shown in Table 1 .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree