Magnetic Resonance Imaging of the Foot and Ankle
Clyde A. Helms
MR is playing an increasingly important role in the examination of the foot and ankle (1). Orthopedic surgeons and podiatrists are learning that critical diagnostic information can be obtained in no other way and are relying on MR for many therapeutic decisions.
Tendons
One of the more common reasons to perform MR of the foot and the ankle is to examine the tendons. Although multiple tendons course through the ankle, only a few are routinely affected pathologically. These are primarily the flexor tendons, located posteriorly in the ankle. The extensor tendons, located anteriorly, are rarely abnormal. Only those tendons that are more commonly seen to be abnormal will be discussed in detail.
Tendons can be directly traumatized or be injured from overuse. Either etiology can result in (1) tenosynovitis, which is seen on MR as fluid in the tendon sheath with the underlying tendon appearing normal, and (2) tendinosis, which is seen as increased signal within a tendon that does not get fluid-bright on T2WI and represents myxoid degeneration. The tendon may or may not demonstrate focal or fusiform swelling; (3) a partial tear, which has fluid signal within the tendon on T2WI or is attenuated in its diameter, and (4) tendon rupture, which is best identified on axial images by noting the absence of a tendon on one or more images. Complete tendon disruption can be difficult to see on sagittal or coronal images because of the tendency for tendons to run oblique to the plane of imaging. An exception to this is the Achilles tendon, which is usually best seen on a sagittal image (2).
It is important to distinguish between a partial tear and a complete disruption because surgical repair is often warranted for the latter and not for the former. Making the distinction clinically is often difficult.
Achilles Tendon
The Achilles tendon does not have a sheath associated with it; therefore, tenosynovitis does not occur. Tendinosis and partial tears are commonly seen in the Achilles tendon. Because complete disruption is such an easy clinical diagnosis, MR is usually not necessary. Complete disruption is commonly seen in athletes and in males who are approximately 40 years of age. It is also commonly associated with other systemic disorders that cause tendon weakening, such as rheumatoid arthritis, collagen vascular diseases, crystal deposition diseases, and hyperparathyroidism.
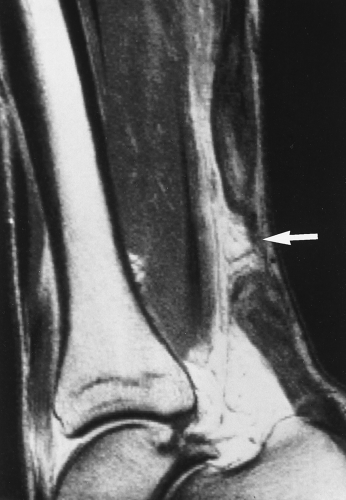
Achilles tendon disruption can be treated surgically or by placing the patient in a cast with equinus positioning (marked plantar flexion) for several months. Which treatment is superior is a controversial issue, with both methods of treatment seemingly working well. MR is being used by many surgeons to help decide if surgery should be performed. If a large gap is present (Fig. 49.1), some surgeons feel surgery should be performed for reapposition of the torn ends of the tendon; on the contrary, if the ends of the tendon are not retracted, nonsurgical treatment is preferred. No published papers have shown that this is, in fact, valid.
Posterior Tibial Tendon
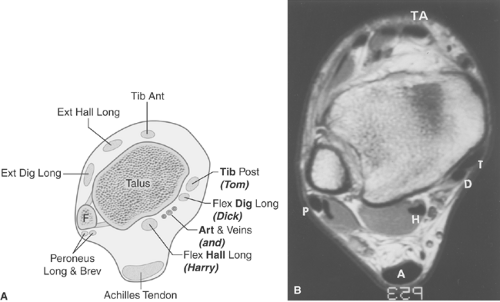
The flexor tendons are easily remembered and identified by using the mnemonic “Tom, Dick, and Harry,” with Tom representing the posterior tibial tendon, Dick the flexor digitorum longus tendon, and Harry the flexor hallucis longus (FHL) tendon. The posterior tibial tendon (PTT) is the most medial and the largest, except for the Achilles, of the flexor tendons (Fig. 49.2). The PTT inserts onto the navicular, second and third cuneiforms, and the bases of the second to fourth metatarsals. As it sweeps under the foot, it provides some support for the longitudinal arch; hence, problems in the arch or plantar fascia can sometimes lead to stress on the PTT with resulting tendinitis or even rupture. Posterior tibial tendinosis and rupture are commonly encountered in patients with rheumatoid arthritis.
Differentiation of partial tears from tendon rupture can be difficult, and MR has become very valuable for making this distinction (3). Most surgeons will operate on a disrupted PTT; however, nonoperative therapy is usually preferred for tendinosis and partial tears.
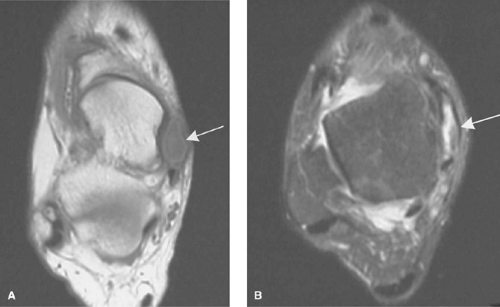
Posterior tibial tendinosis is seen on axial T1WI as swelling and/or signal within the normally low-signal tendon on one or more images (Fig. 49.3). T2WIs show the signal in the tendon getting brighter but not fluid-bright. Tendon disruption is
diagnosed by noting the absence of the tendon on one or more axial images (Fig. 49.4). This typically occurs just at or above the level of the tibiotalar joint.
diagnosed by noting the absence of the tendon on one or more axial images (Fig. 49.4). This typically occurs just at or above the level of the tibiotalar joint.
Rupture of the PTT results clinically in a flat foot due to the loss of arch support given by this tendon. The spring ligament runs just deep to the PTT and then goes underneath the neck of the talus, which it supports in a sling-like fashion. When the PTT tears, the stress is then placed on the spring ligament to support the talus and the arch. The spring ligament has a high incidence of disruption when the PTT tears. The spring ligament is identified on axial and coronal images just deep to the PTT. When it is stressed, it typically gets scarred and thickened (Fig. 49.5). A tear can be diagnosed by noting a gap in the ligament.
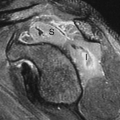
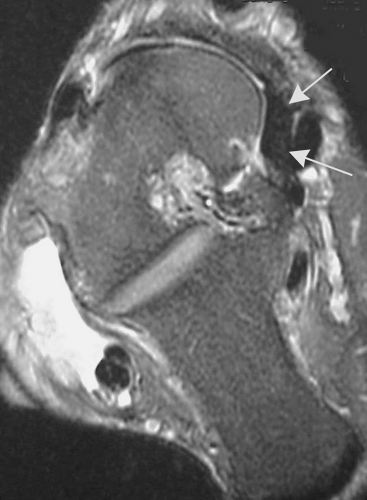 Figure 49.5. Abnormal Spring Ligament. An axial T2WI through the ankle shows a markedly thickened spring ligament (arrows) just deep to the posterior tibial tendon. |
After the PTT and the spring ligament tear, the next structures to fail are the subtalar joint ligaments in the sinus tarsi. In a report of 20 patients with PTT tears, it was found that 92% of the cases had abnormal spring ligaments (thickened or torn), and 75% had an abnormal sinus tarsi (4). It is clear these structures are linked, and injury or stress to one can affect the others.
Flexor Hallucis Longus Tendon
The FHL tendon is easily identified near the tibiotalar joint because it is usually the only tendon at that distal level that has muscle still attached. In the foot, the FHL can be seen beneath the sustentaculum talus, which it uses as a pulley to plantar flex the foot.
The FHL is known as the Achilles tendon of the foot in ballet dancers because of the extreme flexion positions they employ. Ballet dancers often will have tenosynovitis of the FHL, seen on MR as fluid in the sheath surrounding the tendon. Care must be taken to have clinical correlation because fluid can be seen in the FHL tendon sheath from a joint effusion, because the FHL tendon sheath communicates with the tibiotalar joint in as many as 20% of normal patients. Rupture of the FHL is rare.
Peroneus Tendons
The peroneus longus and the peroneus brevis tendons can be seen posterior to the distal fibula, to which they are bound by a thin fibrous structure, the superior retinaculum. The fibula serves as a pulley for the tendons to work as the principal
evertor of the foot. The tendons course close together adjacent to the lateral aspect of the calcaneus until a few centimeters below the lateral malleolus where they separate, with the peroneus brevis tendon inserting onto the base of the fifth metatarsal and the peroneus longus tendon crossing under the foot to the base of the first metatarsal. Avulsion of the base of the fifth metatarsal from a pull by the peroneus brevis tendon is known as a “dancer’s fracture” or a Jones fracture.
evertor of the foot. The tendons course close together adjacent to the lateral aspect of the calcaneus until a few centimeters below the lateral malleolus where they separate, with the peroneus brevis tendon inserting onto the base of the fifth metatarsal and the peroneus longus tendon crossing under the foot to the base of the first metatarsal. Avulsion of the base of the fifth metatarsal from a pull by the peroneus brevis tendon is known as a “dancer’s fracture” or a Jones fracture.
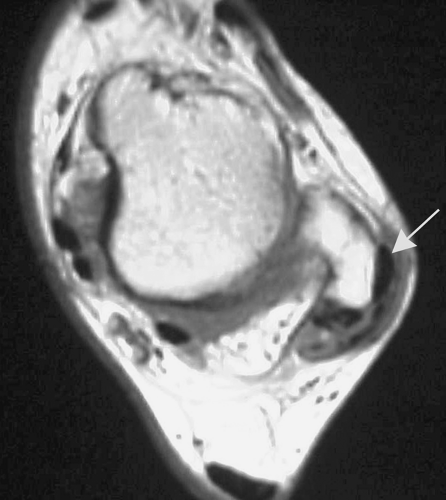 Figure 49.6. Dislocated Peroneus Longus Tendon. An axial T1WI in this rock climber who injured his ankle in a fall shows a low-signal rounded structure (arrow) lateral to the lateral malleolus. This is a dislocated peroneus longus tendon.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|