T2 w HASTE
T2 w fat-suppressed HASTE
T2 w BLADE-TSE
True FISP
T1 w VIBE
Repetition time (ms)
1,000
1,000
3,880
3.5
6
Echo time (ms)
85
85
130
1,46
2.7/3
Section thickness (mm)
5–6
6
5–6
4
3/3.5
Slice/s
30/20 s
30/23 s
10/20 s
30/20 s
30/19 s
Slice gap (%)
10 %–0
10 %
10 %
15 %
3D
Matrix
256 × 182
256 × 182
356 × 256
256 × 182
256 × 159
FOV (mm2): variable
350
350
350 × 350
350
350
Flip angle (°)
150–180
150–180
150
60
10
Slice orientation
Axial-corona
Axial
Axial-coronal
Axial-coronal
Axial-coronal
Gadolinium chelate iv
–
–
–
–
60 s delay
Negative superparamagnetic contrast agent
Yes
Yes
Yes
No
Yes
Biphasic contrast agent
Multiple artefacts
No
No
Yes
Yes
Retrograde air inflation may be useful to distend the colon, the air having a negative contrast effect, although it may be risky in case of severe colonic inflammation and less tolerated by patients.
Alternatively, biphasic contrast agents such as polyethylene glycol, may be used, producing a negative effect on T1-w and a positive effect on T2-w images.
Biphasic contrast agents are frequently used in IBD, being easily available and inexpensive [6–10] (Fig. 5.2). They are more effective on T1-weighted imaging and balanced imaging (True-FISP, FIESTA) rather than with T2-weighted imaging, due to inhomogeneous signal related to frequent flow-void artefacts.
5.2.2 Sequences
MRI assessment of IBD should always include T1-weighted sequences after gadolinium injection for the excellent display of bowel wall inflammation. These sequences, available in 2D or 3D breath hold acquisition, with and without fatsuppression, are labelled in different ways in different MR systems (FSPGR, VIBE, Thrive, etc.) and characterized by a short acquisition time (<1 s for slice). A 60 s delay after gadolinium injection is adequate to obtain a good assessment of the wall and mesenteric vascularity. Suppression of the fat signal is mandatory for the evaluation of wall enhancement after gadolinium injection, although it may obscure evidence of mesenteric lymph nodes [7–9].
T2-weighted sequences are very sensitive in detecting inflammatory tissues, but only under adequate image conditions and with optimal and intestinal contrast, particularly in association with negative superparamagnetic contrast agents. Half-Fourier single-shot turbo spin-echo (HASTE) T2-weighted sequences are commonly used in the evaluation of the bowel, in breath hold or breath hold free acquisition, being characterized by a very short acquisition time (<1 slice/s). Having high intrinsic contrast and adequate spatial resolution (Figs. 5.1a, c, f, g, h, i, j, 5.3a, b), they are effective in detecting bowel wall and mesenteric inflammation, both with and without fat suppression [9]. Balanced sequences (true-FISP Fiesta), T1 and T2-weighted images are valuable in association with a biphasic in contrast agents (Fig. 5.2a, b).
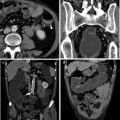
Fig. 5.1
9-year-old boy, with severe bloody diarrhoea and weight loss, affected by UC as confirmed at endoscopy and histology. Three consecutive MRI studies were performed within a period of 14 months from the initial diagnosis, showing caudocranial progression of the colonic disease in spite of the pharmacological therapy. No oral contrast was administered due to low patient compliance. Starting with a prevalent severe involvement of the rectum and sigmoid colon, observed in the first examination, the disease progressed to a severe involvement of the left colon in the second examination and the transverse colon, in the third one. The patient was finally treated with total proctocolectomy and ileo-anal pouch. For a direct comparison, the axial images of the three different examinations are shown consequentially, as well as the coronal views. The first examination includes (a, b and c), the second, performed 10 months after the first one, includes (d, e and f) and the third examination, performed 3 months after the previous (g, h, i and j). Axial T2-weighted half-Fourier single-shot turbo spin-echo (a), axial T1- weighted gadolinium-enhanced images (b) and coronal T2-weighted half-Fourier single-shot turbo spin-echo (c) of the first examination show diffuse wall thickening of the sigmoid colon and extensive Gd-enhancement, suggesting severe inflammation. Notice that the external wall profile is very regular even in very active disease, due to the prevalent inflammation of the inner wall layers (a white arrow). Axial images of the second examination (d and e) show only minimal reduction of wall thickness in the sigmoid colon, severe wall inflammation being still evident. Notice the minimal amount of perivisceral free fluid (white arrow head), suggesting acute disease. On the coronal image (f) a continuous inflammatory involvement from the proximal sigmoid colon up to the splenic flexure (f white arrow) is observed, with loss of the colonic haustra and tubular aspect of the bowel (f black arrow), due to severe wall oedema. In the third and last examination (g, h, i and j) there is a further reduction of wall thickness and a recovery of the austral folds (i white arrow head) in the left colon, due to reduced wall inflammation, as also confirmed at endoscopy. Unfortunately, the disease progressed and worsened in the transverse colon (j). Due to persistence of severe symptoms the patient underwent total colectomy.
Fig. 5.2
Active ulcerative “pancolitis with back-wash ileitis” in a 10-year-old male with clinical and endoscopic signs of active UC. This patient assumed a biphasic oral contrast agent. a The coronal True FISP image shows a mild diffuse thickening of the terminal ileum (white arrow), as well as of the right colon. b T1 VIBE post-contrast fat-saturated coronal MRI image of the same patient shows diffuse wall enhancement of terminal ileum, ileocecal valve and right colon, findings consistent with active colitis and backwash ileitis (white arrow head)
5.3 Assessment of Intestinal Disease and Perivisceral Manifestations
5.3.1 Intestinal Wall Characterization
The typical inflammatory process of UC, being confined to the mucosal and submucosal layers only, determines mild wall thickness with sparing of outer layers (muscularis propria and serosa). Colonic wall thickening is, in fact, usually lower in UC than in CD, with a mean value of 7 mm versus 13 mm, respectively, as reported in previous CT studies [4, 11–13]. At MRI, it can be detected both on T1- and T2-weighted images (Fig. 5.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree