CHAPTER 19 Magnetic Resonance Imaging Safety
In 2008, MRI safety came under scrutiny by The Joint Commission when a sentinel event alert was issued in the United States because of widespread adverse events. The alert was based on 398 adverse events reported to the U.S. Food and Drug Administration’s (FDA) Manufacturer and User Facility Device Experience Database (MAUDE) over a 10-year period, 9 of which were deaths.1 Burns from significant heating of wires and leads were the most common problem reported at more than 70% of the MRI-related incidents. Adverse events and accidents in the MRI environment happen because of failures in adherence to proper MRI safety procedures, inappropriate use of equipment, outdated safety information, lack of training for individuals working in the MRI environment, and lack of appropriate supervision of the MRI suite.1,2 The safety problems in MRI cannot be taken lightly because the safety issues surrounding MRI are complicated and often unpredictable. The Joint Commission’s recommendations for reducing accidents and injuries in MRI follow the “ACR Guidance Document for Safe MR Practices,”3 and can be found at http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_38.htm or http://www.acr.org/SecondaryMainMenuCategories/quality_safety/MRSafety/safe_mr07.aspx.
This chapter provides an overview of MRI safety as it pertains to patients with cardiovascular disease, with suggestions of supplemental information and references. MRI safety is an enormous topic that is constantly changing, and a host of Web-based resources are available. Questions of MRI safety need to be evaluated with the most up-to-date information possible, which is why providers need to research the specific devices and scanning circumstances carefully. Box 19-1 lists useful websites for the reader’s reference. MRI safety guidelines are updated on a regular basis. Failure to follow current safety guidelines puts patients at increased risk for injury and, in some instances, results in unnecessary avoidance of clinically necessary MRI examinations.
BOX 19-1
Recommended Websites
GENERAL CONCERNS
Hazards
Individuals who are not educated and trained for safety in the MRI environment cause an added level of danger because they are unfamiliar with the dangers and safety precautions needed to ensure safe operation of equipment in the MRI scanner area. Many accidents are a result of noncompliance with safety guidelines, or of adherence to outdated guidelines. The ECRI Institute, a nonprofit health services research organization, recommends that MRI clinics appoint a safety officer to oversee the establishment, implementation, and maintenance of MRI safety policies and procedures, something The Joint Commission and American College of Radiology (ACR) also recommend as a prudent preventive measure.1,3,4
Magnetic Resonance Imaging Clinic
The physical facilities of an MRI facility play a direct role in safety. Site planning for an MRI system should be done to limit access of non-MRI personnel to the actual MRI scanner room. Only properly screened patients and personnel should be allowed into the MRI scan room, and they should be allowed in the scan room only with the direct supervision of qualified MRI professionals. The ACR has recommended a clinic design safety template that includes control of site access restriction.3 An MRI facility should be considered to be made up of four zones as outlined by the “ACR Guidance Document for Safe MR Practices” (Fig. 19-1).3 Zone I is the area outside the actual MRI facility, and it is open to the general public. This is the area where the general public, patients, health care workers, and MRI center employees enter the MRI facility.
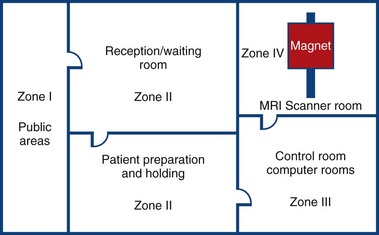
 FIGURE 19-1 The four zones (I, II, III, and IV) of an MRI suite.
FIGURE 19-1 The four zones (I, II, III, and IV) of an MRI suite.
(From Kanal E, Barkovich AJ, Bell C, et al; ACR Blue Ribbon Panel on MR Safety. ACR guidance document for safe MR practices: 2007. AJR Am J Roentgenol 2007; 188:1447-1474.)
Physics of Electricity and Magnetism
Maxwell’s equations are the building blocks of our understanding of electricity and magnetism. The four equations known as Gauss’ law for electricity, Gauss’ law for magnetism, Faraday’s law, and Ampere-Maxwell law help in understanding many of the important elements of MRI safety.5 The mathematical predictions for safety cannot be calculated easily. Ensuring the safety of a device in a patient undergoing an MRI examination requires knowledge of the device, the specific MRI system, the type of RF coils used, the sequences employed for imaging, the way the patient loads the scanner and transmit RF coil, and whether or not monitoring or gating equipment is also being used. It is nearly impossible to predict all of the possible ways for heat deposition or current induction that may occur with a given implant in a patient—hence the safety dilemma.
Static Magnetic Field Strength
Currently, most clinical scanners for cardiac use are operating at a static magnetic field of 1.5 T or 3 T. Table 19-1 outlines the FDA significant risk recommendations. Magnetic fields have the potential for translational and rotational (or torque) effects. Basically, magnetic field interactions increase as the static magnetic field strength increases. If a device is considered to pose a potential safety concern, it is prudent to consider carefully the potential options for such scanning at the lowest field strength appropriate for the imaging needs (e.g., coil selection, imaging pulse sequence selection). Imaging time is also important because the increase in scan time may prolong the requirements for monitoring a child or a sedated claustrophobic patient. Discussion with the patient on what to expect and the need for the patient to communicate any unusual sensations immediately is imperative. Devices and scanners vary considerably, so many factors must be considered. Substances that are attracted to the magnetic field are often referred to as having ferromagnetic properties. Devices that are ferromagnetic have the potential to interact with the magnetic field in a translational or rotational manner (or both), possibly causing great harm to the patient or equipment or both. The plethora of MRI accident pictures that are available via the Internet provide some idea of the danger of the static magnetic field of the MRI scanner. Many pictures of objects flying into scanners can be found at sites such as Simply Physics (http://www.simplyphysics.com/flying_objects.html).
TABLE 19-1 Static Main Magnetic Field Limit Recommendations by the U.S. Food and Drug Administration*
| Population | Main Static Magnetic Field Greater than (tesla) |
|---|---|
| Adults, children, and infants >1 month old | 8 |
| Neonates (<1 month old) | 4 |
* The FDA considers an MRI scanner to be of significant risk when it is operating above the levels listed.
From United States Food and Drug Administration, Center for Devices and Radiological Health. Guidance for Industry. Criteria for significant risk investigations of magnetic resonance diagnostic devices. Available at: http://www.fda.gov/cdrh/ode/guidance/793.pdf. Accessed June 5, 2008.
Gradient Magnetic Fields
MRI scanners use time-varying magnetic fields called gradients to encode for field of view, slice thickness, and other imaging parameters, and in certain aspects of pulse sequence image contrast. Stronger and faster gradients and more powerful RF transmission coils are being used in MRI scanners.6 The current FDA limit for gradient magnetic field rates of change (dB/dt) varies depending on operating conditions. Significant risk for dB/dt is classified as when painful nerve stimulation or severe discomfort is produced.7 Gradient fields are magnetic fields that are much weaker than the main magnetic field, but they are switched on and off very quickly and, according to Maxwell’s equations, can induce time-varying electrical currents.8 Gradients can induce currents in conductive materials9 and potentiate peripheral nerve stimulation, but are typically not painful on current FDA-approved MRI systems.10 This is a safety concern because these gradient currents have the potential also to induce currents in certain cardiac devices, which could induce arrhythmias.9 Tandri and coworkers8 reported that gradient currents may be strong enough under certain conditions to distort pacing pulses, which is significant enough to interfere with myocardial capture or loss of capture when patients with pacemakers are scanned in MRI. This finding reinforces the need for prudent screening and risk/benefit considerations with patients with any kind of implanted cardiac device.
Radiofrequency Fields
The transmit RF coils of the MRI scanner emit RF energy that is specifically tuned to the tissue of interest at a given static magnetic field strength. RF energy is absorbed by the tissue and released, producing signals that receiver coils can detect. RF energy may cause heating of biologic tissues, however, when the tissues are exposed to excessive RF energy levels. To ensure patient safety, levels of RF energy used for MRI procedures indicated in the units of specific absorption rate (SAR), are recommended by the FDA. Generally, MRI scanners calculate or estimate SAR based on the patient’s weight and report values in W/kg. In 2003, the FDA relaxed the SAR limits as follows: 4 W/kg—whole body for 15 minutes, 3 W/kg—head for 10 minutes, 8 W/kg—peak 1 g of tissue (head or torso) for 15 minutes, 12 W/kg—peak 1 g of tissue (extremities) for 15 minutes.7
SAR increases with increasing static magnetic field strength, flip angle, duty cycle of the equipment, and patient size.11 The SAR experienced at 3 T is approximately four times the absorption rate as 1.5 T,12 making some of the cardiac imaging at 3 T potentially challenging. The SAR can be reduced, however, by modifying parameters such as flip angle, repetition time, slice thickness, imaging matrix, and echo train length, depending on the pulse sequence and the desired image contrast. Parallel imaging schemes have been a successful strategy for SAR reduction at 3 T.
Cryogens
Cryogens are used to create superconducting MRI scanners. Liquid helium is the most common cryogen used in MRI scanners today, but liquid nitrogen is also used in some systems. Generally, only service engineers come in contact with the cryogens; however, if the cryogen system malfunctions, a quench can occur. A quench is the rapid release of the cryogen liquid (in the form of gas) from the MRI scanner that brings the magnetic field strength of the MRI scanner down very quickly. A quench can be problematic if the MRI scan room is built with the door opening inward, and there is not a pressure release mechanism.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


