(1)
Radiology – Neuroradiology Section, S. Paolo Hospital, Bari, Italy
Magnetic resonance imaging (MRI) has made a major contribution in the last decade to an early diagnosis of spondyloarthritis, other than a better understanding of the course of the disease [1–3]. Moreover, MRI may be used as an objective outcome measure for clinical trials [1, 4, 5].
Regarding other radiological techniques, conventional radiography can only detect chronic bony changes (i.e., osteosclerosis, erosions, syndesmophytes) in the late stages of spondyloarthritis. Such bony structural changes can be better detected by computed tomography (CT), but this imaging technique is rarely used because of a much higher radiation exposure. Finally, scintigraphy has been used in the past to detect foci of active inflammation but no longer plays a role in the diagnosis and follow-up of spondyloarthritis because of limited sensitivity and specificity and radiation exposure [1, 6].
In this perspective, MRI emerges as the gold standard imaging technique to detect spinal inflammation in clinical practice, in both early and late disease stages.
It is mandatory to use a proper MRI study protocol, given that “standard” examinations do not always allow a correct diagnosis.
All the patients in this series were examined with a 1.5 T MR system (Siemens Symphony-TIM) by using the following basic study protocol:
Cervical/Dorsal/Lumbosacral Spine
TSE T1-weighted images on the sagittal plane.
TSE T2-weighted images with fat saturation on the sagittal plane.
TSE T2-weighted images with fat saturation on the axial plane (eventually to be conducted on the pathologic area, for a better spatial characterization of the edematous lesion).
TSE/SE T1-weighted images with fat saturation on the sagittal and axial planes following the administration of contrast medium (eventually to be conducted to identify the active inflammatory stage of the disease). In this series, we administered Dotarem, Guerbet (0.5 mmol/ml, 0.2 ml/kg, dose), as intravenous paramagnetic contrast medium.
Sacroiliac Joints
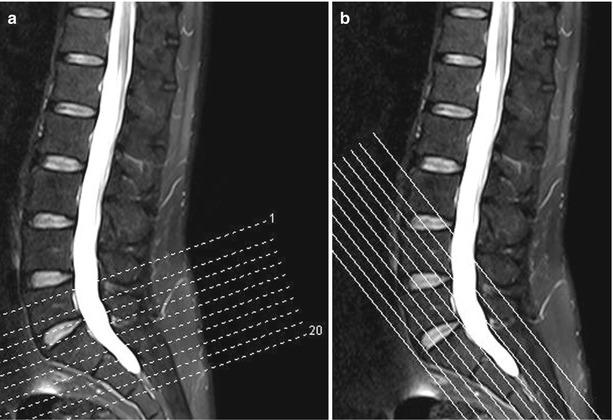
The sacroiliac joints are imaged in axial orientation and semicoronal section orientation along the long axis of the sacral bone (Fig. 3.1a, b):
TSE T2-weighted images with fat saturation on the axial and semicoronal plane
TSE T1-weighted images on the axial plane
GE T2*-weighted images on the semicoronal and axial plane (eventually to be obtained to highlight joint erosions)
TSE/SE T1-weighted images with fat saturation on the semicoronal and axial planes following the administration of contrast medium (eventually to be conducted to identify the active inflammatory stage of the disease)
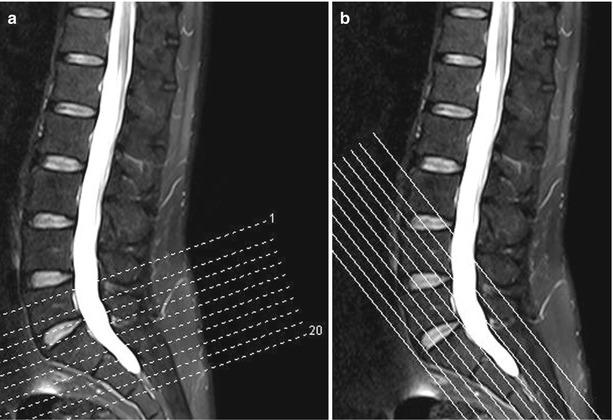
Fig. 3.1
MRI of the sacroiliac joints. Correct positioning of the slices in axial orientation (a) and semicoronal orientation along the long axis of the sacral bone (b)
An efficient spinal imaging protocol must comprise fat-suppressed T2-weighted sequences, in particular with fat saturation technique or STIR sequences, in order to clearly visualize hyperintensity corresponding to edematous lesions, otherwise not easily identifiable with “standard” imaging sequences without fat suppression (Figs. 3.2 and 3.3).

Get Clinical Tree app for offline access

Fig. 3.2
Sagittal TSE T2-weighted image with fat saturation (a) and “standard” sagittal TSE T2-weighted image without fat saturation (b). Hyperintense lesions in fat-suppressed T2-weighted image in the anterior corners of the vertebral bodies L2 and L4, indicating edematous lesions (a




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree