MALIGNANT TUMORS OF THE EXTERNAL AND MIDDLE EAR AND MASTOID
KEY POINTS
- Imaging is critical to medical decision making in temporal bone malignancies.
- A variety of diseases of the temporal bone and adjacent sites can mimic cancers of the temporal bone.
The most common malignancies involving the temporal bone are those that arise from the skin of the pinna and periauricular region that secondarily invade the temporal bone (Chapter 24). Primary cancers of the external auditory canal (EAC) are uncommon, and those of the middle ear are rare. These include such diverse lesions such as papillary adenocarcinoma of the middle ear and endolymphatic sac and transitional cell and carcinoid tumors of the middle ear. Some carcinomas may be associated with chronic infection. Differentiation of these by imaging from the more common squamous cell carcinoma is not possible except for the rare endolymphatic cancer that is diagnosed by its morphology (Chapter 12), anatomic location, and von Hippel-Lindau syndrome association. Temporal bone tumors may be confused with chronic inflammatory disease and as a result may be diagnosed late.
A paraganglioma is the most common tumor seen in the temporal bone. This tumor is only occasionally malignant and is discussed in detail in Chapters 33 and 123.
Rhabdomyosarcoma may arise in the middle ear in children (Chapter 35). Ewing sarcoma (Chapter 30), osteosarcoma (Chapter 38), and other mesenchymal-origin lesions uncommonly originate from the temporal bone.
The histiocytoses frequently involve the temporal bone, mainly in the pediatric age group (Chapter 19). Other hematopoietic and lymphoid tumors rarely present primarily in the temporal bone (Chapters 27 and 28).
Metastases (Chapter 43) to the temporal bone are very unusual, although their incidence may be underestimated because the symptoms such as hearing loss and those of chronic mastoiditis are overshadowed by more disabling symptoms of the primary tumor. Metastases are usually the result of hematogenous spread and may involve both ears. The most commonly reported primary tumors are breast, lung, renal, and prostate carcinoma.1
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
A detailed and complete knowledge of normal temporal bone anatomy is required for evaluation of cancer in this region. Computed tomography (CT) and magnetic resonance imaging (MRI) of the parotid and periparotid region, nasopharynx, surrounding deep spaces, facial nerve, and regional lymphatics also must be understood when evaluating malignancies of the temporal bone. The most common key elements in this evaluation include the following:
- Soft tissues: Parotid gland and capsule attachments to the EAC, parapharyngeal space, upper masticator space, and temporomandibular joint (Chapter 175)
- Temporal bone: EAC, roof of the middle ear and mastoid, carotid canal and jugular fossa, and petrous apex (Chapter 104)
- Nerves/Facial nerve: Brain stem to the parotid, the auriculotemporal nerve to V3, and the trigeminal ganglion (Chapter 104)
- Vascular structures: Internal carotid artery, jugular vein and bulb, and major dural venous sinuses of the posterior fossa
- Regional lymphatics: Parotid nodes and cervical lymph node levels 1 through 5, external jugular nodes, retropharyngeal nodes, mastoid, and occipital nodes (Chapters 149 and 175)
The gross anatomy most pertinent to evaluation of malignancy is summarized here.
The pinna and cartilaginous portion of the EAC are skin covered with numerous associated hair follicles and sebaceous and ceruminous glands. In the bony EAC, the skin firmly adheres to the periosteum. The entire external ear canal is about 2 to 4 cm long, the lateral third being fibrocartilage and the remainder being bone up to the bony tympanic ring where the tympanic membrane attaches and separates the EAC and middle ear (Figs. 104.21–104.23). Both the bony and cartilage parts of the EAC may be incomplete, with gaps that are filled with fibrous tissue. The temporomandibular joint lies anteroinferior to the EAC. Part of the tissue of the joint capsule may on occasion herniate into a small anteroinferior EAC bony dehiscence. The capsule of the parotid gland attaches to the cartilage of the EAC, providing a bidirectional conduit for spread of pathology arising from either structure (Fig. 104.20).
The mastoid lies posterior to the EAC and contains the descending facial canal and its nerve as it exits the skull into the stylomastoid fat pad.
The capillary lymphatics of the EAC drain to the parotid, preauricular, mastoid, suboccipital, and posterior neck chains that have ultimate connections to levels 2 and 5 (Chapters 24, 149, and 157).
The middle ear cavity is connected to the mastoid and eustachian tube. The tympanic cavity and mastoid antrum and air cells are lined by ciliated and nonciliated columnar epithelium. This epithelium extends into the eustachian tube to the nasopharynx.
The tympanic cavity and mastoid likely do not have significant capillary lymphatics, nor does the inner ear labyrinth. Capillary lymphatics are described for the mucosa. The cartilaginous portion of the eustachian tube has capillary lymphatics that drain to predominantly parotid, retropharyngeal, and level 2 nodes.
The petrous apex is home to the carotid canal. The jugular fossa is at the boundary of the petrous and mastoid portions of the temporal bone. The transverse and sigmoid sinuses drain to the jugular bulb, and one side is often dominant in this posterior fossa venous drainage pattern.
IMAGING APPROACH
Techniques and Relevant Aspects
Imaging is indispensable for the differential diagnosis and in planning therapy for malignancies of the temporal bone. Both CT and magnetic resonance (MR) are often necessary. CT is usually the primary study because the assessment of bony detail is critical to surgical decision making. MR is used in advanced lesions to evaluate perineural spread and dural and brain involvement as well as to separate obstructive from tumor-associated mastoid and middle ear changes. Anatomic imaging usually suffices for evaluation of adjacent major vascular structures, including the dural sinuses, the jugular vein, and the carotid. Carotid balloon occlusion testing may be done if carotid sacrifice is anticipated.
CT and MRI must be carefully supervised when evaluating malignancies of the temporal bone. Even 2- or 3-mm differences in tumor extent can markedly alter the morbidity of surgical management. The techniques and supportive rationale required for such high-quality scans may be reviewed if necessary. These are summarized in Appendixes A and B.
CT scans must be done with a slice thickness of 0.50 to 0.75 and a combination of a focused (7- to 9-cm) temporal bone field of view and wider fields of view encompassing surrounding soft tissues and the adjacent brain. These must be processed with bone and soft tissue algorithms. MR studies should be focused on the precise area of interest and done with the highest possible spatial resolution. Focused studies with small field of view coils produce the best results. Coronal and axial MRI sections are fundamental. Sagittals may be used selectively. Intravenous contrast is typically used in both studies.
Pros and Cons
Most lesions of the EAC are epithelial in origin and often are biopsied before imaging. However, any subcutaneous or submucosal lesion should be studied with CT and supplemented with MR whenever necessary prior to biopsy. Lesions that are not obviously cholesteatoma and that present medial to the tympanic ring and tympanic membrane should always be imaged first with CT before biopsy. MRI is usually done second and is focused on a particular concern that might alter medical decision making. Imaging prior to biopsy can limit hemorrhagic complications of biopsy that can occur with a paraganglioma. It can also avoid rare complications such as sampling of an aberrant carotid or encephalocele. In this way, imaging may obviate middle ear exploration in some patients.
SPECIFIC DISEASE/CONDITION
Carcinoma of the External and Middle Ear and Mastoid
Benign neoplasms such as squamous cell papilloma and adenomas are uncommon in the EAC and rare in the middle ear. Rare malignancies such as papillary adenocarcinoma and transitional cell and carcinoid tumors of the middle ear cannot be differentiated from each other by imaging. Endolymphatic sac papillary carcinoma is discussed in conjunction with petrous bone malignancies.
Carcinomas of the EAC are almost exclusively squamous cell and basal cell skin carcinomas and are the most common primary EAC lesion (Fig. 24.21 and Chapter 24). More commonly, squamous cell carcinoma and basal cell carcinoma arise from the pinna and skin over the temporal bone to involve that structure (Figs. 122.1–122.3). Melanomas and Merkel cell carcinoma can also arise from the skin in these areas to invade the temporal bone. Ceruminous gland adenocarcinoma is a rare tumor arising from modified sweat glands of the EAC. Tumors arising from the tympanic cavity, mastoid, or eustachian tube are all rare. The specific tumor types reported include squamous cell carcinoma and benign and malignant salivary gland tumors. These tend to arise from the medial two thirds of the eustachian tube and the middle ear.
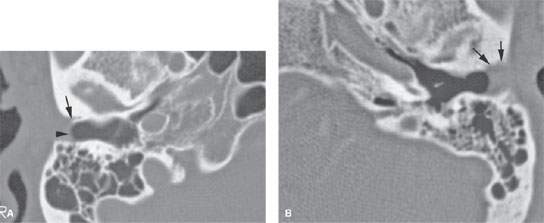
FIGURE 122.1. A patient with carcinoma of the pinna. A: Baseline normal side showing the junction of the cartilage (arrowhead) and bony (arrow) portion of the external auditory canal (EAC). On the opposite side, there is extension of the tumor along the cartilage portion of the EAC to invade the lateral aspect of the bony canals (arrow).
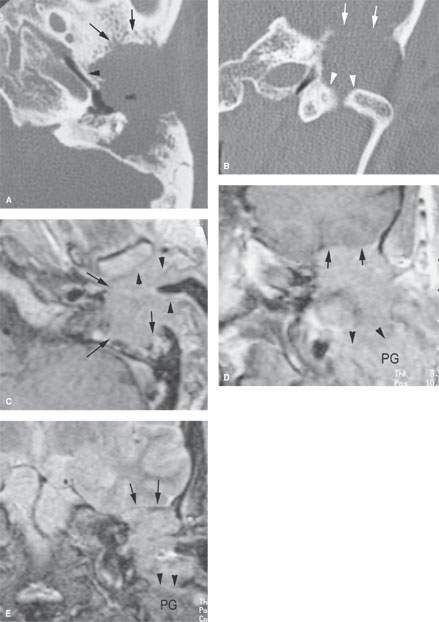
FIGURE 122.2. A patient with cancer of the external ear. A, B: Computed tomography images showing an extensive infiltrating mass destroying the mastoid and invading the root of the zygoma (arrows). The tumor involves the wall of the bony eustachian tube (arrowhead). In (B), the mass erodes the bone of the glenoid fossa (arrows), exposing the floor of the middle cranial fossa as well as displacing the condylar head of the mandible and eroding the bone of the medial aspect of the glenoid fossa (arrowheads). C–E: Magnetic resonance (MR) study on the same patient. In (C), the contrast-enhanced T1-weighted (T1W) image correlates with that in (A). The mass extends from the cartilage portion of the external auditory canal (arrowheads) to invade the soft tissues around the temporomandibular joint capsule and likely the capsule itself. The tumor then extends medially to destroy the mastoid (arrows). In (D), contrast-enhanced T1W coronal MR shows a relatively sharp interface with dura and no abnormal dural enhancement. This is likely intracranial extradural invasion. Inferiorly, the mass invades the parotid gland (PG) (arrowheads). In (E), the T2-weighted coronal MR image shows the displaced thickened dura without brain invasion (arrows) and the interface between the inferior tumor margin where it involves the parotid gland (PG) (arrowheads).
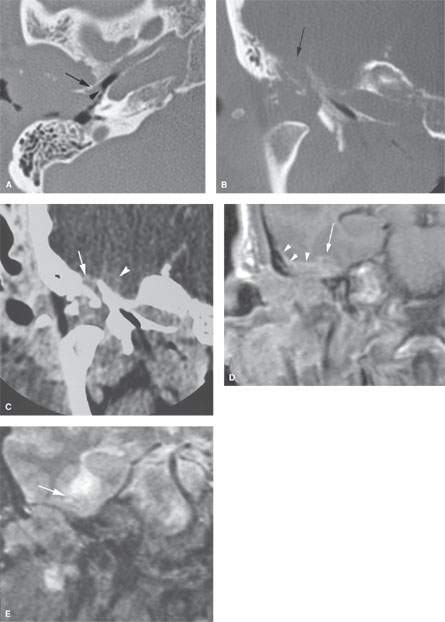
FIGURE 122.3. A patient with advanced squamous cell carcinoma of the ear with intracranial invasion. A: There is destruction of the external auditory canal and tumor extending along the bone of the hypotympanum (arrow) with tumor growing toward the bony eustachian tube (arrowhead). B: There is destruction of bone between the glenoid fossa and floor of the middle cranial fossa (arrow). C: Contrast-enhanced computed tomography viewed at brain windows showing intracranial spread with an apparently sharp dural interface at one point (arrow) and possible brain invasion (arrowhead) at another. The relationship of tumor to brain and dura is uncertain. D: T1-weighted coronal image with contrast showing reactive dural changes (arrowheads) along most of the intracranial invasion interface; however, there is also evidence of leptomeningeal enhancement (arrow). E: T2-weighted coronal image showing evidence of brain edema. Surgery confirmed early brain invasion.
Prevalence and Epidemiology
Most cancers of this region are induced by sun exposure since they are skin cancers. Immune-compromised patients have an increased incidence of these skin cancers, and these malignancies may be more aggressive in that population. Other carcinomas may arise due to long-standing infections. Others are sporadic. This is essentially a disease of adults that has no particular prevalence based on patient gender.
Clinical Presentation
EAC tumors usually present as a painless skin lesion in the canal. Further growth causes minor bleeding, pain, itching, and drainage. These symptoms and signs mimic benign inflammatory disease. There may be a conductive hearing loss when the EAC is occluded or the tympanic membrane or middle ear becomes involved.
A good deal of growth may occur beneath the skin surface. A preauricular mass or fullness may be present or herald deep spread to surrounding structures. Trismus may result from invasion of the temporomandibular joint. The external ear is often involved.
Middle ear cancer may be seen in patients with long-standing middle ear inflammation (Fig. 122.4). Pain, discharge, and facial nerve palsy are possible presenting complaints. Carcinoma rarely arises in the eustachian tube. When it does, patients will usually have pain and otitis with conductive hearing loss. Advanced lesions may have associated deficits of cranial nerves VII through XII and possibly Horner syndrome. The naso-pharynx will appear normal. Imaging with CT and MRI are essential to avoid a delay in diagnosis. Physical examination typically will reveal findings that mimic benign disease unless there are cranial nerve deficits.
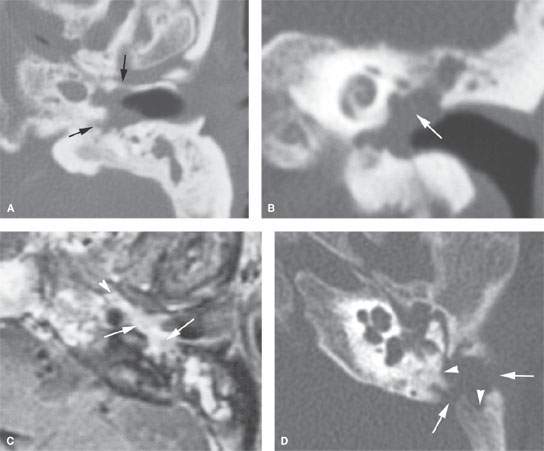
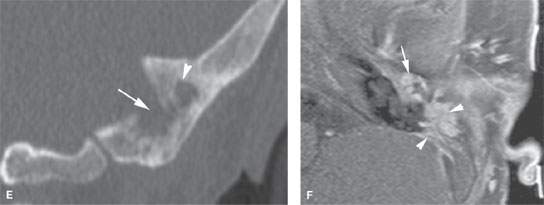
FIGURE 122.4. Two patients with destructive processes within the middle ear. A–C: Patient 1. There is a soft tissue mass in the middle ear and external canal in this patient with a history of chronic otomastoiditis. Possible bony erosive changes and reactive changes are present (arrows). In (B), the coronal image shows complete absence of the ossicles and the presence of the soft tissue mass (arrows). In (C), the contrast-enhanced T1-weighted (T1W) image shows an enhancing middle ear mass (arrows) extending into the eustachian tube. (NOTE: The findings are indistinguishable from an inflammatory destructive middle ear process. In this patient, carcinoma of the middle ear and long-standing infection as a possible etiology was confirmed at surgery. D–F: Patient 2 with conductive hearing loss and ear pain. In (D)and (E), computed tomography shows a destructive mass centered in the mastoid both eroding bone within the mastoid antrum (arrowheads) and destroying the cortical bone over the sigmoid plate and external cortex of the mastoid (arrows). Coronal images show a combination of erosive (arrow) and reactive (arrowhead) changes. In (F), the contrast-enhanced T1W fat-suppressed image shows abnormal enhancing tissue surrounding the ossicles (arrow) and within the mastoid antrum associated with the bony changes seen in (C) and (D). These findings were due to Langerhans cell histiocytosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








