Abstract
Beginning in the second half of the 20th century, the most common allegations in medical malpractice lawsuits filed against physicians in the United States changed from committing complications to failure to diagnose cancer and other serious injuries; that is, accusations of commission were replaced by errors of omission. Inasmuch as the determination of medical diagnoses very often involved, and continue to involve, radiologic imaging, radiologists are currently more often a defendant in malpractice lawsuits than in the past. Allegations of missed cancer of the lung and of the breast, failure to communicate serious radiologic findings to referring physicians, and failure to adhere to American College of Radiology parameters are on the rise. Risk management can lessen the likelihood of incurring a medical malpractice lawsuit, maximize chances for a successful defense if such a suit is filed, and, even more importantly, enhance good patient care. More recent issues regarding radiologic practice include “defensive medicine,” how to manage and report incidental findings that are being increasingly seen in high-tech imaging such as computed tomography and magnetic resonance exams, and whether radiologists should disclose to patients and apologize for errors they have committed.
Keywords
Malpractice, radiologic errors, communication failure, missed radiologic diagnoses, teleradiology, mammography, risk management, ACR parameters
Prologue
To gain a more meaningful understanding of the current state of affairs with regard to medical malpractice litigation in the United States, we begin by looking back at certain events that have brought us to the present.
England, 1765
British legal scholar Sir William Blackstone published Commentaries on the Laws of England, in which “neglect or unskillful management of a physician or surgeon” was referred to as “mala praxis.” It is from this term that the modern word “malpractice” is derived.
Connecticut, 1832
A state supreme court establishes the Standard of Care (SOC) for a physician: “A physician and surgeon is liable for injuries resulting from the want of ordinary diligence, care, and skill.… Ordinary means usual, common. If you were to draw a line of distinction just halfway between the eminently learned physicians and those grossly ignorant, you would hit exactly on those who are ordinary.”
Pennsylvania, 1853
A state supreme court added the following: “The law requires physicians to possess reasonable skill and diligence… not extraordinary skill such as belongs only to few men of rare genius and endowments.”
Colorado, 1896
One year after Roentgen’s discovery of the x-ray, an x-ray image showing a bone fracture was offered as legal evidence for the first time in an American court. Disagreeing with a lawyer’s arguing against admitting the x-ray, the judge stated: “We have been presented with a photograph showing a femur bone which is surrounded with tissues and therefore is hidden…. Modern science has made it possible to look beneath the tissues of the human body and has aided in telling hidden mysteries. The photograph will be admitted in evidence.”
United States: First Half of the 20th Century
In the decades prior to the end of World War I, most malpractice cases focusing on radiology involved alleged x-ray and radium burns. For the entire first half of the 20th century, most malpractice lawsuits filed against all physicians focused on errors of commission : that is, the doctor did something wrong.
United States: Second Half of the 20th Century
Beginning in the early 1950s, allegations of malpractice evolved from errors of commission to errors of omission; that is, the doctor failed to do something right: they failed to make a timely diagnosis. In the last 3 decades of the 20th century, allegations of malpractice against radiologists focused mainly on failure to diagnose; that is, the radiologist missed an abnormality on the radiographic images. By the mid-1980s, missed lung and breast cancers became the most frequent reason radiologists were sued for malpractice.
United States: The Present
Of all radiology medical malpractice lawsuits, 57% to 67% are diagnosis related. Failure to diagnose accounts for most of these. Only 2% of all patients sustaining adverse events file malpractice lawsuits.
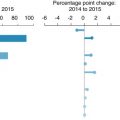
How often are radiologists sued for malpractice?
A recent review of malpractice records of more than 8400 radiologists found that 50% of radiologists would be sued by age 60. A later survey disclosed that 75% of radiologists were sued for malpractice at least once in their lifetime. A recent report focusing on all medical malpractice cases reported to the National Practitioner Data Bank between 2005 and 2014 revealed that internists accounted for 15% of all cases; obstetrician-gynecologists, 13%; general surgeons, 12%; orthopedic surgeons, 7%; and radiologists, 6%. Other studies have disclosed that the number of malpractice lawsuits filed in the United States has decreased 10% to 15% over the past several years, but payment per case has increased (Medical Protective Insurance Company unpublished report).
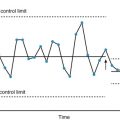
Radiologic Errors
Causes of error in radiology are multifactorial: poor technique, failure of perception, lack of knowledge, poor judgment. Numerous research studies reported over the past 60 years have disclosed an average 30% “miss rate” in the retrospective evaluation of general radiographic, computed tomography (CT), magnetic resonance, and ultrasound examinations. This means that if 100 radiologic examinations containing abnormal findings are given blindly to radiologists, an average of 30% of the abnormalities will be missed. Such studies, however, do not reflect the everyday practice of radiology, where the number of normal examinations far exceeds those that are abnormal. Various studies and performance improvement data derived from radiologists’ interpretations under ordinary working conditions of both normal and abnormal radiologic studies disclose an average error rate of 3% to 4%. Fortunately, most of these errors are not injurious to the patient or are corrected by review of radiologic studies before they become injurious.
Seventy percent of missed radiologic diagnoses are perceptual in nature; that is, the radiologist fails to “see” the abnormality. The remaining 30% are cognitive errors; that is, the radiologist “sees” an abnormality but attaches the wrong significance to what is seen, either through lack of knowledge or lack of judgment. Diagnostic errors are also caused by the phenomenon known as “satisfaction of search”; that is, an imaging study may contain several abnormalities. The radiologist notes one or perhaps two abnormalities but then tends to “stop looking” for additional abnormalities; his or her “search” has been “satisfied” prematurely. Another cause of errors is the “alliterative” error, also termed “diagnosis momentum.” Here, the radiologist looks at a previous study and previous report rendered by the same or another radiologist before interpreting the new follow-up study, and if the previous diagnosis was erroneous, the radiologist interpreting the new study has a tendency to repeat the same error.
Errors Versus Differences of Opinion
Variations in diagnosis are thought to imply the presence of error, but this is not always the case. Variation may reflect error but can be a genuine difference of opinion. Variability can occur as inconsistencies in practice by the same radiologist on different occasions or discrepancy between radiologists. Radiology researchers have found that experienced radiologists miss 30% of radiographs positive for evidence of disease and, furthermore, will disagree with themselves 20% of the time. A study by Harvard University radiologists disclosed that radiologists disagree on interpretation of chest radiographs as much as 56% of the time. Another academic study disclosed that up to 90% of all lung carcinomas were missed by radiologists when interpreting radiographs. A University of Arizona study found that in 75% of mammograms initially interpreted as normal, breast carcinomas were seen on retrospective evaluation.
The main reason for studying medical errors is to try to prevent many, if not most, of them. Physicians feel a sense of guilt as a result of making an error and may fear suffering professional and economic consequences and being isolated by their colleagues. Unfortunately, a friendly and confidential reporting culture does not exist in medicine. The current “blame culture” in healthcare inhibits error reporting. To lower the miss rate, we need to develop a safety culture so that we can bring errors to our colleagues’ attention in a sensitive and constructive fashion. Such a culture will exist only when radiologists who make errors use such feedback positively as a learning experience and know that punitive action will not be taken against them.
Unfortunately, errors of perception are an unavoidable hazard of the human condition. Although technology has made enormous progress in the last century, there is no evidence of similar improvement in the performance of the human eye and brain.
Radiology diverges from the normal path of most other medical specialties in that it depends entirely on visual perception. However, lest nonradiologic physicians believe that radiologists’ error rates are considerably higher than their own; in fact, studies that date back as far as the 1950s reveal a 20% to 30% error rate in clinical medicine. For example, medical researchers have found clinicians to be unreliable in their assessment in 32% of physician examination skills. Accuracy in the physical diagnosis of abdominal ascites was as low as 56% among good clinicians. Pediatricians were 50% accurate in clinical diagnosis of acute otitis media; otolaryngologists were 73% accurate.
Autopsies revealed a major missed diagnosis 25% of the time; despite more modern diagnostic techniques, the number of missed major diagnoses has not changed over 30 years. A meta-analysis of 53 autopsy articles published over a 40-year period disclosed a major finding median error of 23.5%, with a range of 4% to 50%. “The error rate has been strikingly unchanged,” emphasized the authors.
False-Positive Radiologic Findings
Although almost all radiologic diagnostic errors are false-negative errors, occasionally there are false-positive errors. A review of claims occurring in the United Kingdom between 1995 and 2006 disclosed that 7% were due to false-positive radiologic findings.
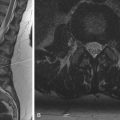
A very sad medical malpractice lawsuit from Massachusetts is an unfortunate illustration of a false-positive rather than a false-negative radiologic error. A 4-month-old infant was admitted to the hospital with symptoms of urinary tract infection and started on intravenous (IV) antibiotics. Although improving, a precautionary sonogram was done and showed a “lesion” in the upper pole of the right kidney, suspicious for Wilms tumor. A CT scan confirmed a positive right renal Wilms tumor. The patient was taken to surgery, during which the surgeon felt a subtle enlargement of the kidney and proceeded to perform a nephrectomy. Postsurgical study of the kidney revealed chronic pyelonephritis but no evidence of tumor. A malpractice lawsuit was filed and eventually settled for $500,000.
In the 70 years since radiologic errors were first acknowledged, the error rates have not decreased appreciably. This must not dissuade us from making every effort to reduce them, however. Yes, to do so is a daunting challenge, but radiologists cannot simply shrug their shoulders and walk away. Will computers help us decrease errors? A recently published study suggests that the answer is likely no. In a study comparing the results of 496,000 women whose screening mammograms were interpreted with the aid of computer-assisted detection (CAD) with 130,000 women whose mammograms were interpreted without CAD over a period from 2003 to 2009, no statistical difference in sensitivity and specificity was found. The researchers’ conclusion was that CAD does not improve diagnostic accuracy in mammography interpretations.
It is highly unlikely that radiologists will ever be able to eliminate radiologic interpretive errors, but we can reduce them by adhering to the following suggestions:
- •
Possess sufficient knowledge of the modality by which the image being interpreted was obtained.
- •
Ensure prompt transmission of imaging reports to the ordering physician and possibly to the patients themselves.
- •
Expend sufficient time interpreting and reporting.
- •
Be cautious about voice recognition and templates.
- •
Proofread dictated reports.
- •
Because poor image quality increases the likelihood of missing an abnormality, insist that patient positioning and radiographic exposure be adequate before interpretation.
- •
Have available as much patient information as possible, along with previous radiologic examinations and reports for comparison, but take care not to be overinfluenced by this information.
- •
Considering all possible diagnostic possibilities is far preferable to making hasty conclusions.
- •
When interpreting studies that are follow-ups from previous studies, ask the following: “Could the findings represent anything different from the previously suggested diagnosis?”
- •
When asked by a referring physician, “What did you find on the radiologic examination of my patient?” instead of recalling what was diagnosed, if time permits a much better answer would be, “I interpreted the study as normal (or as showing specific pathology), but let’s look at it again together” (if physician is present) or “let me look at it again” (if physician is not present). A second look by the radiologist with or without a referring physician or colleague can reveal a radiographic finding that was initially overlooked or misinterpreted.
- •
Occasionally the patient’s physical condition or other circumstances may prevent technologists from obtaining all required views or using optimal exposure techniques. In such circumstances, state in the report that the examination was incomplete because of the patient’s condition and that additional or follow-up views need to be obtained when the patient’s condition permits.
- •
Consultation with radiology colleagues and referring physicians before rendering final reports is encouraged.
- •
Make recommendations for additional or follow-up studies when indicated.
- •
Making instant or rapid diagnoses may be acceptable goals in film-interpreting conferences at medical meetings, but doing so in everyday practice may cause radiologists to limit diagnostic possibilities and may increase the likelihood of error. Taking sufficient time during radiologic interpretation for deliberation and reflection is essential for good judgment.
- •
“If you don’t think of it, you won’t diagnose it” is a basic axiom in diagnostic radiology. Radiologists must constantly reinforce and expand their reservoir of radiology knowledge by reading current scientific publications and attending continuing medical education programs.
As we look toward the future, the major issue about which we should be concerned is electronic medical records (EMRs). Mistyped words, reversed numbers, inaccurate information, or other data entry mistakes are often “cut and pasted” repeatedly in the patient record; templates are often repeated even though minor imaging changes may occur. Every time an exam or image is reviewed on a monitor, it is accurately timed and permanently recorded; EMRs are anticipated to cause an increase in the number of medical malpractice lawsuits, although data are not yet available.
Proving Malpractice
To prevail in a medical malpractice lawsuit involving a defendant-radiologist, the plaintiff must prove that (1) the radiologist had a physician-patient relationship with the patient, (2) the radiologist committed a negligent act, (3) the negligent act caused an injury to the patient (proximate cause), and (4) the patient sustained injury directly from the defendant’s alleged negligent conduct. In almost all cases, items 1, 3, and 4 are obvious and therefore rarely challenged. As for the physician-patient relationship, anytime the radiologist interprets a radiologic study on a patient, whether that interpretation is written and included in a formal medical record or was given by conversing with a referring physician who later, in his own chart, writes a notation of his conversation with the radiologist, a physician-patient relationship has been legally established. Thus, in almost all medical malpractice lawsuits, the single point to be debated and argued is whether the defendant acted in a negligent manner. How is the word negligence defined? What constitutes physician negligence? Let us go back to an 1860 medical malpractice lawsuit when physician negligence was argued for the first time before the Illinois State Supreme Court. In that case, a farmer named Richie sustained a fracture of the wrist and was treated by Dr. West, a general practitioner. Dr. West applied a plaster cast to the wrist, but for some inexplicable reason, Mr. Richie’s wrist became permanently deformed. He sued Dr. West, alleging malpractice. Dr. West retained a Springfield, Illinois, attorney by the name of Abraham Lincoln. A trial was held, and a jury rendered a verdict in favor of Mr. Richie; Dr. West appealed the matter to the Illinois Supreme Court, which issued a decision affirming the jury verdict:
When a person assumes the profession of physician and surgeon, he must be held to employ a reasonable amount of skill and care. For anything short of that degree of skill, the law will hold him responsible for any injury which may result. While he is not required to possess the highest order of qualification, to which some men attain, still he must possess and exercise that degree of skill which is ordinarily possessed of the profession, and whether the injury results from a want of skill, or the want of its application, he will, in either case, be equally liable.
At about the same time, the Georgia Supreme Court issued a similar opinion:
The physician must exercise a reasonable degree of care and skill. He does not undertake to use the highest possible degree of skill, for there may be persons who, for having enjoyed a better education and greater advantage, are possessed of greater skill in our profession; but he undertakes that he will bring a fair, reasonable and competent degree of skill.
Over the next several decades, appellate or supreme court decisions in all American states rendered opinions using similar wording. In other words, the courts have stated that an accused physician’s performance must be compared to a “standard” performance that does not need to be ideal, perfect, extraordinary, excellent, or match that of an expert witness. Rather, it is compared to a standard of performance that is ordinary and/or reasonable . Herein lies one of the basic problems that has always existed in medical malpractice litigation, namely, how the words reasonable and ordinary are defined. Defining the exact meaning of these two words might seem simple, but it is not. Webster’s dictionary defines reasonable as “not extreme, not excessive, moderate, not demanding too much, possessing good sound judgment, well-balanced, sensible.” The word ordinary is defined as “common, lacking in excellence, not distinguished in any way from others, not above but rather below average, somewhat inferior level of quality.” Thus, clear-cut definitions of these two words unfortunately have never been spelled out by the courts. If radiologists, who are trained to precisely pinpoint radiologic abnormalities and render interpretations in specific terms, feel perplexed at the vagueness of the words reasonable and ordinary , they are not alone. More concrete definition of these words remains elusive. Some light was shed on the term reasonable person in a decision of a Canadian malpractice case:
The reasonable person is not an extraordinary or unusual creature; he is not superhuman; he is not required to display the highest skill of which anyone is capable; he is not a genius who can perform uncommon feats, nor is he possessed of unusual powers of foresight. He is a person of normal intelligence who makes prudence a guide for his conduct. He acts in accord with general and approved practice.
Notwithstanding the words of the court, every juror and every jury in every medical malpractice lawsuit will have their own opinion regarding whether a defendant-radiologist acted reasonably under the circumstances described during a malpractice trial.
Defending the Missed Diagnosis
The question to be answered by a jury in a medical malpractice lawsuit involving a missed radiologic diagnosis is theoretically not “Has the radiologist missed an x-ray finding, or made an erroneous interpretation?” Rather, it should be “Has the radiologist missed an x-ray finding, or made an erroneous interpretation, which could have been missed, or made by an ordinary radiologist, practicing in a reasonable (average) manner?” There are several major issues that exacerbate a jury’s difficulty in determining whether a radiologist’s conduct was negligent or not. One is hindsight bias , defined as “the tendency for people with knowledge of the actual outcome of any event, to believe falsely that they would have predicted the outcome.” Researchers have repeatedly pointed out that the retrospective reader has new information regarding the clinical course and later x-ray findings showing advanced disease that were not available at the time of the original interpretation. This improves the ability to perceive subtle abnormalities that were not seen on the previous study. Perception is better if you know where to look. The courts do attempt to minimize the effect of hindsight bias. One typical instruction to a jury states:
I charge you that in a medical malpractice action, physicians cannot be found negligent for assessing a patient’s condition which only later or in hindsight proved to be incorrect, as long as the initial assessment was made in accordance with the then-reasonable standards of medical care. The concept of negligence does not encompass hindsight.
An Illinois Appellate Court decision included the words, “In hindsight, almost everything is foreseeable, but that is not the test we should employ.”
One other inherent problem in medical malpractice litigation that especially involves radiology is outcome bias, which is defined as “[t]he tendency for people to attribute blame more readily when the outcome of an event is serious than when the outcome is comparatively minor.” In other words, hypothetically, if a radiologist is accused of negligence for missing a rib fracture that can be plainly seen in retrospect, most jurors and others would conclude that there was no negligence, because the injury was so minimal. On the other hand, if a radiologist is accused of negligence for missing an extremely subtle fracture of the cervical spine that probably would be missed by well over 95% of radiologists, but the patient is now quadriplegic, most jurors and physicians would agree that the radiologist was negligent, because the injury, that is, the outcome, was so serious and debilitating.
It is very difficult, but certainly not impossible, to convince a jury that a radiologist who is well paid and is supposed to be well trained to find all abnormalities on a radiologic study should be excused for failing to perceive a radiologic abnormality that in retrospect can be readily perceived by medical and nonmedical observers alike. However, solid defense-supporting data are available that may at times be presented to a jury that can assist in achieving vindication for the defendant-radiologist. These data include statistics regarding the frequency of errors committed by radiologists and other physicians during the course of an ordinary everyday practice, the factors that limit conspicuity of radiographic densities, limitations of normal human visual perception, and evidence that the process by which the radiologist originally rendered the interpretation was free of deficiency.
Occasionally juries can be successfully educated by defense attorneys and expert witnesses as to psychovisual phenomena and other human limitations affecting the visual process, and radiologists are exonerated for failing to observe and report radiologic abnormalities. A good working relationship between the defendant-radiologist and the defense attorney increases the chances of achieving a satisfactory jury verdict.
Failure of Radiologic Communication
Although missed diagnoses account for the highest average indemnification paid in malpractice lawsuits filed against radiologists, the second highest average indemnification is paid for claims alleging failure of communication. Indeed, data show that failed communication is a factor in up to 80% of radiologic malpractice lawsuits. A survey of American College of Radiology (ACR) members disclosed that more than 25% acknowledged being involved in at least one malpractice claim involving failure to communicate; payment to plaintiffs in such cases averaged nearly $2 million. A more recent ACR survey asked the question, “Has anyone in your group been sued for failure to communicate radiologic findings?” Twenty-three percent answered “yes,” 49% answered “no,” and 28% did not respond (ACR Survey on Communication, unpublished). Also, malpractice insurance carriers have found that in 60% of malpractice lawsuits involving radiologists, the referring physician had never been directly contacted with urgent or significant unexpected findings.
The nation’s courts have consistently ruled that communication of an abnormal radiologic finding is as important as the finding itself. Time and time again, courts have found radiologists liable for failing to directly communicate significant abnormalities to referring physicians. As one state appeals court ruled, “When a patient is in peril of his life, it does him little good if the radiologist has discovered his condition, unless that radiologist informs the patient, or those responsible for his care, of that fact.”
The Practice Parameter for Communication of Diagnostic Imaging Findings calls for radiologists to differentiate between routine and nonroutine communications. Reports of routine imaging findings can be communicated through usual administrative channels. Nonroutine reports that include findings that require immediate physician intervention, differ from a preceding or preliminary interpretation, or contain a significant or unexpected finding should be “expedited in a manner that reasonably ensures timely receipt of the findings.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree