, Gina M. Fundaro1 and Sabala R. Mandava1
(1)
Department of Radiology, Henry Ford Hospital, Detroit, MI, USA
Case 1 Mammographic Artifacts
Patient History
Screening mammograms in multiple different patients.
Radiology Findings
Fig. 1.1 (a) CC and (b) MLO images show a broken ventricular peritoneal shunt catheter in the lower inner right breast at posterior depth.
Fig. 1.2 AP supine view of the chest reveals a broken right ventricular peritoneal shunt catheter and intact left ventricular peritoneal shunt catheter.
Fig. 1.3 Left MLO view demonstrates chin artifact obscuring the superior posterior tissues.
Fig. 1.4 Deodorant artifact. Left MLO view demonstrates (a) scattered radiopaque particles in the skinfold and axillary region. (b) Scattered radiopaque particles in the skinfold and axillary region are no longer seen on repeat left MLO view following cleansing of the patient’s axilla.
Fig. 1.5 Hair artifact. CC view demonstrates curvilinear densities with intervening lucencies at posterior depth laterally.
Fig. 1.6 Motion artifact. Right MLO view demonstrates patient’s motion causing blurring of the upper breast tissues.
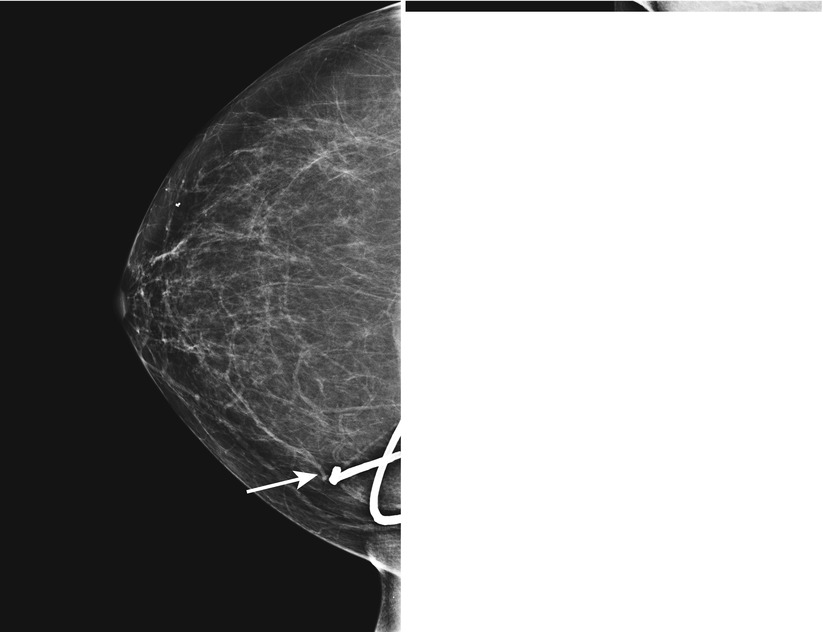
Fig. 1.1

Fig. 1.2
Fig. 1.3
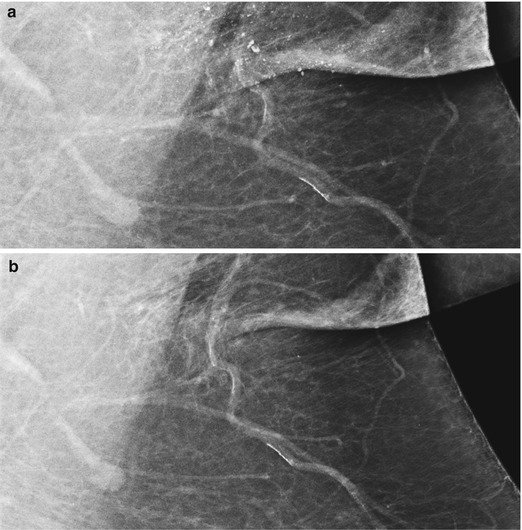
Fig. 1.4
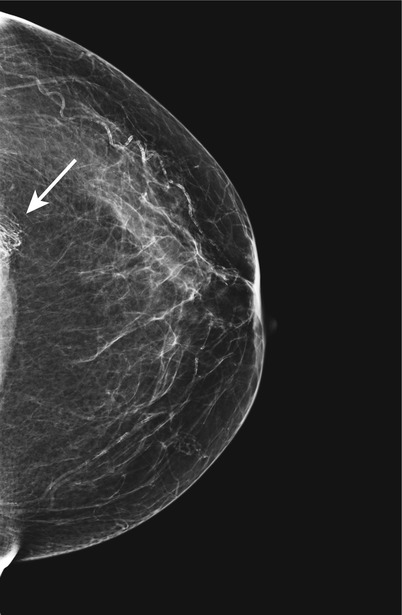
Fig. 1.5
Fig. 1.6
Diagnosis
Mammographic artifacts
Discussion
Artifacts are any objects or abnormalities that are not native to the breast.
May interfere with image interpretation.
Certain artifacts are typically seen in particular locations:
Deodorant: axilla
Catheters or pacemakers: close to chest wall
Hair: typically inner breast seen on CC view
Recognition, awareness, and history are important.
Correct presumed problems and repeat imaging can be done.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-7, p. 10–1.
Hogge JP, Palmer CH, Muller CC, et al. Quality assurance in mammography: artifact analysis. Radiographics. 1999;19:503–22.
Case 2 Secretory Calcifications
Patient History
A 60-year-old female for bilateral screening mammogram.
Radiology Findings
Fig. 1.1 Bilateral (a, b) CC and (c, d) MLO views demonstrate dense, thick, continuous rodlike calcifications in a ductal pattern.
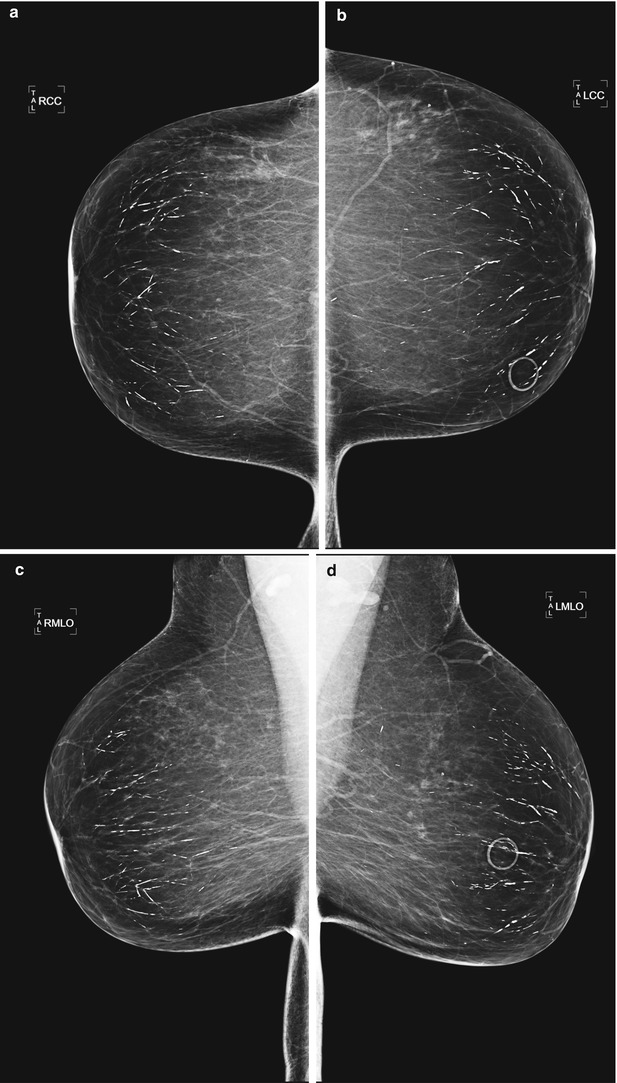
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign finding.
Diagnosis
Secretory calcifications
Discussion
Secretory calcifications arise from secretions and debris within the ducts, which calcify and cause inflammation.
Other names include plasma cell mastitis (typically in premenopausal women) and mammary duct ectasia (typically in post menopausal women).
The calcifications are large and rodlike. Typically radiate from the nipple in a ductal pattern.
Size of the calcifications is greater than or equal to 1 mm.
Rarely seen in patients before the age of 60.
Usually bilateral.
Asymptomatic.
No intervention necessary.
References
American College of Radiology (ACR) BI-RADS® Atlas. ACR BI-RADS® atlas-mammography. 5th ed. Reston: American College of Radiology; 2013. p. 44–6.
Bassett LW, Jackson VP, Fu KL, Fu YS. Diagnosis of diseases of the breast. 2nd ed. Philadelphia: Elsevier; 2005. p. 444–5.
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV 1, p. 74–5.
Case 3 Invasive Ductal Carcinoma (IDC)
Patient History
A 55-year-old female for screening mammogram.
Radiology Findings
Fig. 1.1 (a) CC and (b) ML images show a mass with spiculated margins at 6 o’clock in the left breast at the anterior depth. Another irregular mass with spiculated margins is seen in the upper outer left breast at posterior depth.
Fig. 1.2 (a) Grayscale and (b) color Doppler ultrasound images show a hypoechoic mass with spiculated margins and vascular flow.
Fig. 1.3 (a) Grayscale and (b) color Doppler ultrasound images show an enlarged lymph node with a thickened hypoechoic cortex and a compromised hyperechoic hilum. There is vascular flow within the hilum.
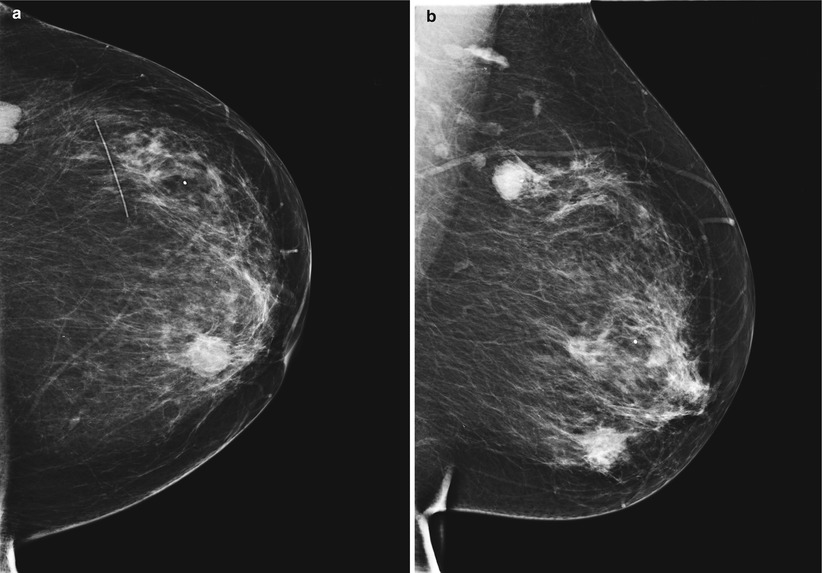
Fig. 1.1
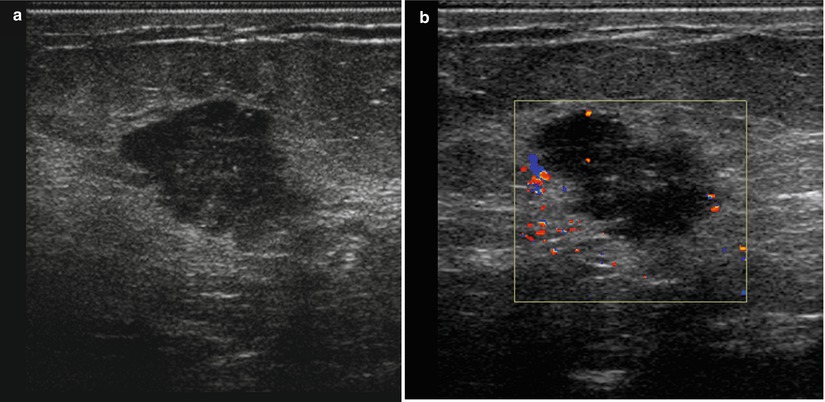
Fig. 1.2
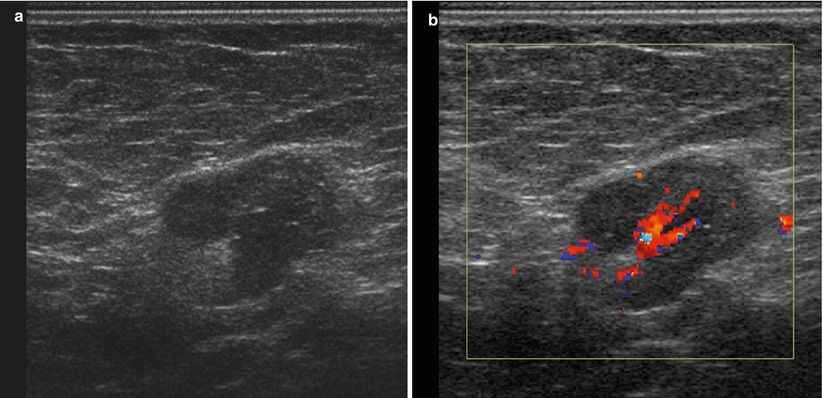
Fig. 1.3
BI-RADS Assessment
BI-RADS 5. Highly suggestive of malignancy (following diagnostic workup, prior to biopsy).
Diagnosis
Invasive ductal carcinoma (IDC) (not otherwise specified) with axillary lymph node metastasis
Discussion
Eighty percent of breast cancers are ductal in origin.
Up to 65 % of breast cancers diagnosed in the USA represent IDC, not otherwise specified.
IDC forms a desmoplastic reaction with cicatrization and fibrosis, thus commonly seen as a spiculated mass on mammogram.
Usually seen as a hypoechoic mass with spiculated or ill-defined margins on ultrasound. Posterior acoustic shadowing of the mass can be seen.
Secondary signs of IDC on imaging include skin thickening, nipple inversion, and lymphadenopathy.
References
Kopans DB. Breast imaging. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1998. p. 577–81.
Ruhbar G, Sie AC, Hansen GC. Benign versus malignant breast masses: ultrasound differentiation. Radiology. 1999;213:889–94.
Case 4 Complicated Cyst
Patient History
A 50-year-old female with a palpable mass in the left breast.
Radiology Findings
Fig. 1.1 (a, b) Grayscale and (c) color Doppler ultrasound images show an avascular oval circumscribed predominately anechoic mass with a dependent layering debris and posterior enhancement.
Fig. 1.2 (a) Grayscale, (b) color Doppler, and (c) grayscale (left image) and strain elastogram ultrasound images of a different patient show an avascular oval circumscribed mass that contains homogeneous, low-level echoes and an intermediate pattern on elastography. On the elastogram color scale, red represents soft and blue represents hard. An adjacent benign simple cyst is seen that has a soft pattern and trilaminar appearance on elastography.
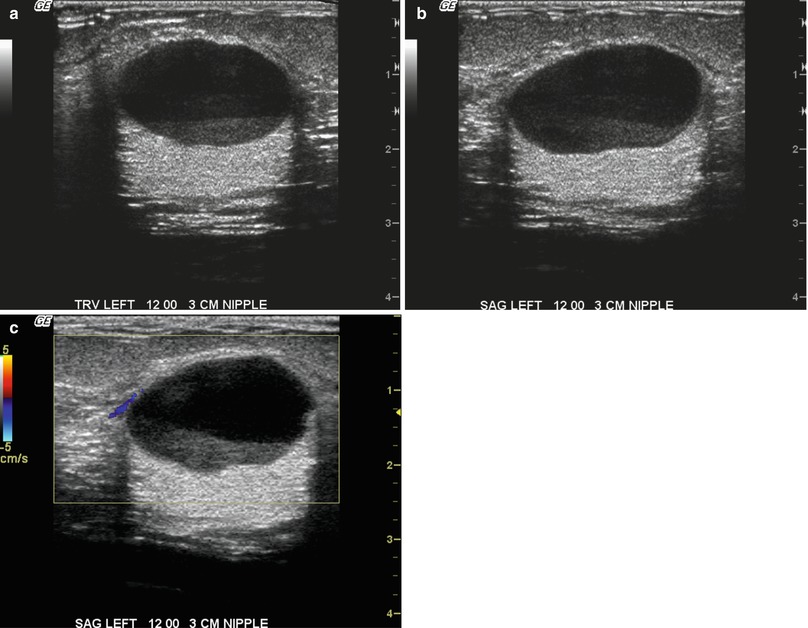
Fig. 1.1
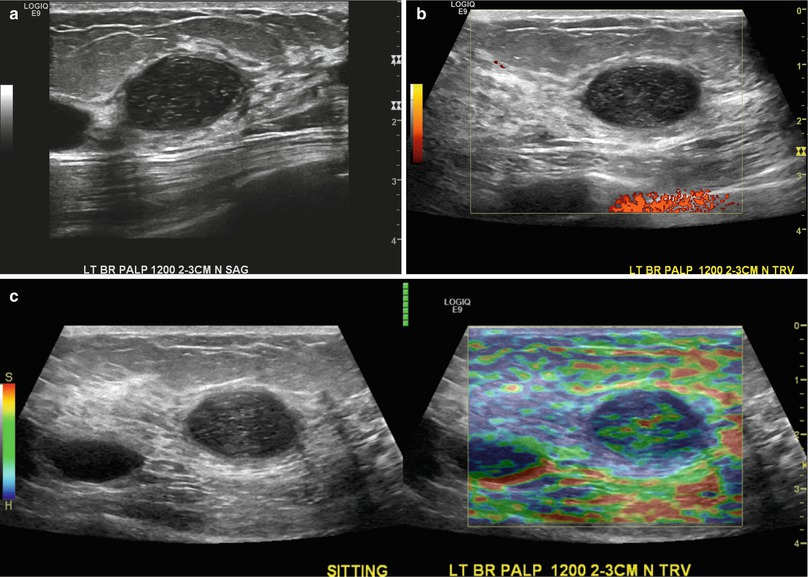
Fig. 1.2
Diagnosis
Complicated cyst
Discussion
A complicated cyst contains:
Fluid–debris level or homogeneous, low-level echoes, without a discrete solid component and with an imperceptible wall.
Imperceptible wall on ultrasound
Mobile debris or homogeneous low-level echoes
Complex features, such as thick irregular septations, intracystic mass, or thick cyst wall, are not seen in complicated cysts.
Can have simple cysts within the vicinity.
Less than two percent risk of malignancy.
No further management necessary for an asymptomatic complicated cyst.
A complicated cyst on baseline mammogram or incidental finding on ultrasound can be followed at 6 months.
Aspiration with possible biopsy can be performed if the following are present:
Symptomatic
New finding
Enlarging complicated cyst
References
American College of Radiology (ACR) BI-RADS® Atlas. ACR BI-RADS® atlas-ultrasound. 5th ed. Reston: American College of Radiology; 2013. p. 96–7, 103.
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-1, p. 34–9.
Berg WA, Campassi CI, Ioffe OB. Cystic lesion of the breast: sonographic-pathologic correlation. Radiology. 2003;227:183–91
Mandell J. Core radiology: a visual approach to diagnostic imaging. 1st ed. Cambridge: Cambridge University Press; 2013. p. 629.
Case 5 Desmoid Tumor
Patient History
An 83-year-old female with a palpable mass in the right axilla. History of right breast lumpectomy and radiation therapy for ductal carcinoma in situ (DCIS).
Radiology Findings
Fig. 1.1 MLO view shows an asymmetry in the right axilla seen only on the MLO view.
Fig. 1.2 (a) Grayscale and (b) color Doppler images show an irregular spiculated hypoechoic mass that is avascular.
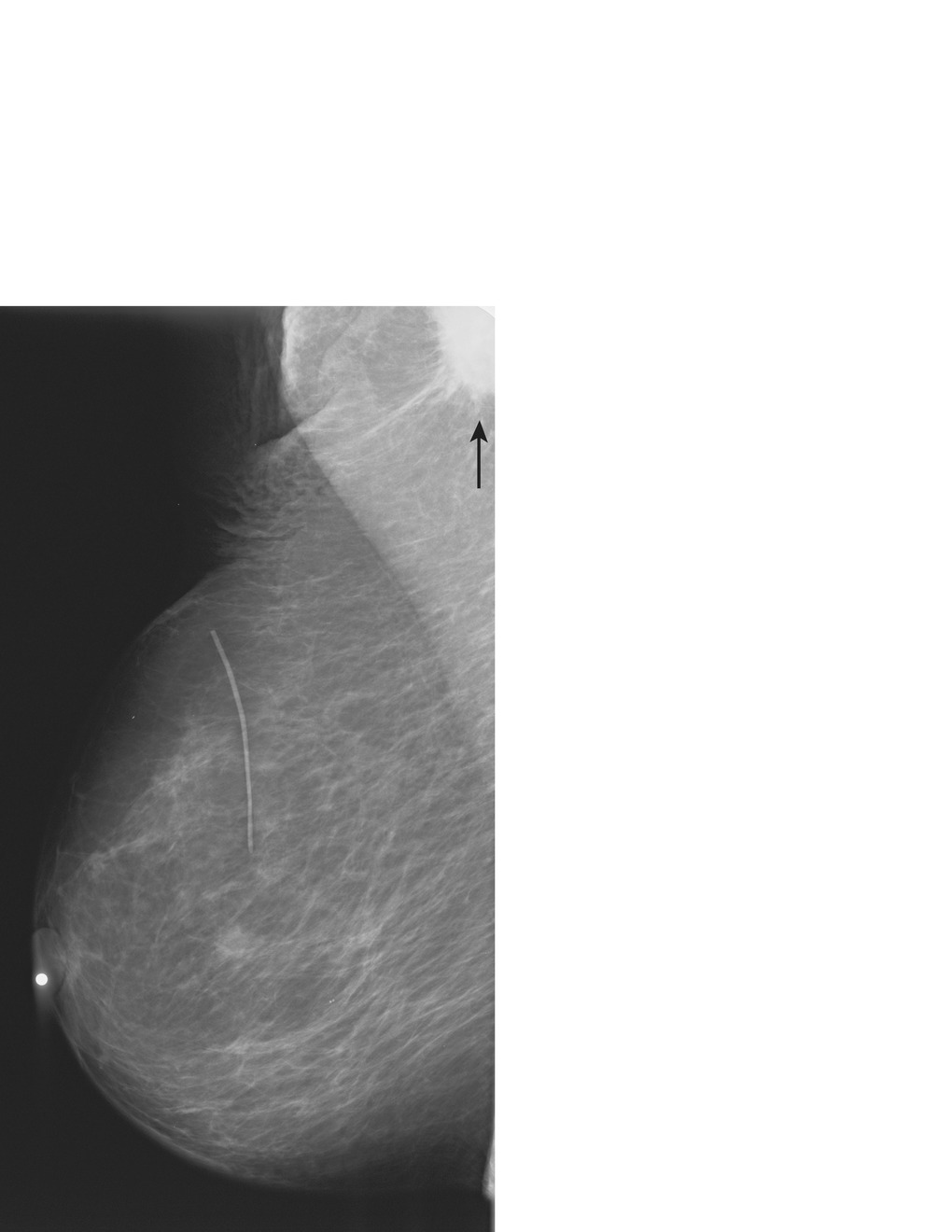
Fig. 1.1
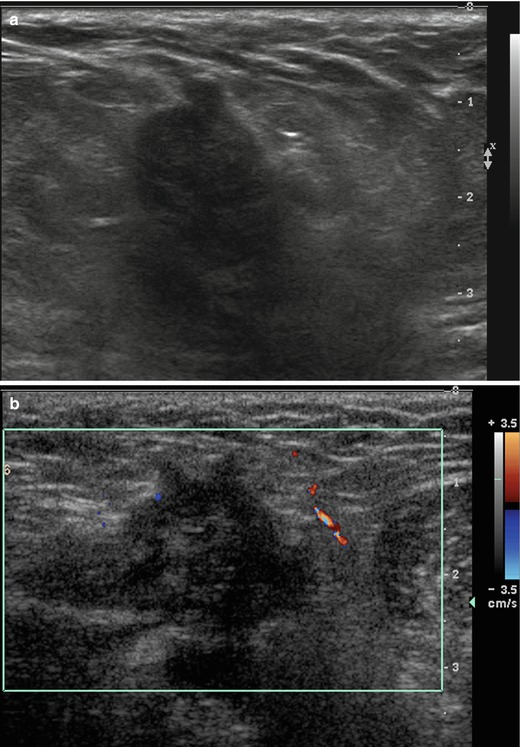
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup and biopsy).
Diagnosis
Desmoid tumor (extra-abdominal desmoid)
Discussion
Desmoid tumor is an infiltrative, locally aggressive area of fibromatosis that may recur locally.
May be related to prior trauma or surgery and has been reported in women with saline breast implants.
Can present as a solitary, hard, painless mass.
On mammography, a mass with indistinct or spiculated margins can be seen.
On ultrasound, a hypoechoic mass with posterior acoustic shadowing can be seen.
Treatment is local surgical excision.
References
Cardenosa G. Breast imaging companion. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. p. 411–2.
Ikeda DM. Breast imaging the requisites. 2nd ed. Philadelphia: Elsevier, Mosby; 2011. p. 401–2.
Case 6 Gynecomastia
Patient History
An 87-year-old male with left breast pain and a palpable mass.
Radiology Findings
Fig. 1.1 Bilateral (a, b) CC and (c, d) MLO images show a focal asymmetry in the retroareolar left breast, corresponding to the triangular marker indicating a palpable mass (circle marker corresponds to a skin mole). The right breast mammogram is negative.
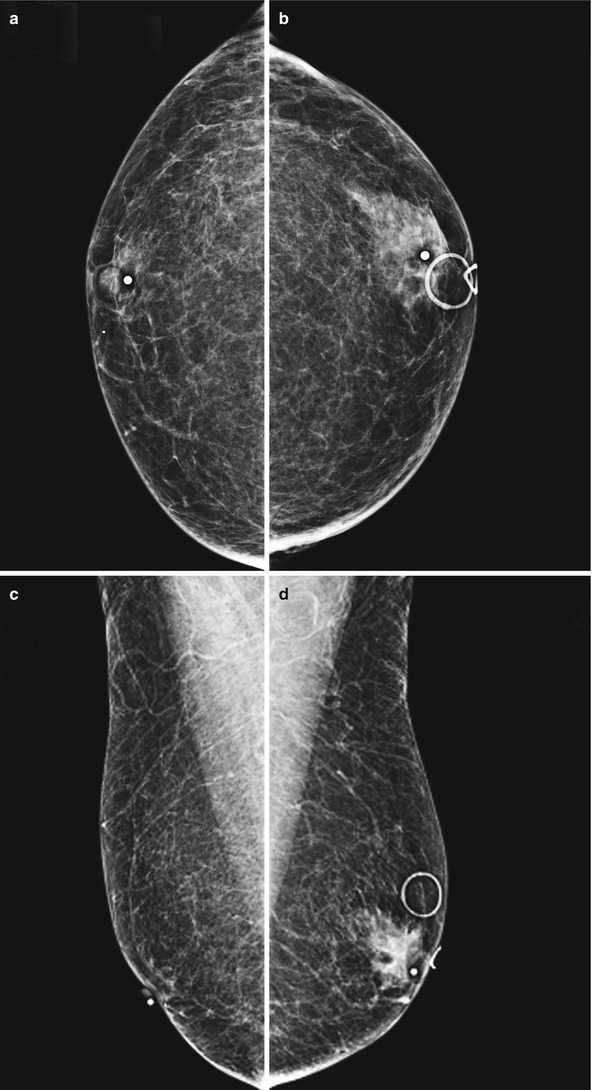
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup).
Diagnosis
Gynecomastia
Discussion
Gynecomastia is characterized by hyperplasia of ductal and stromal elements of the male breast.
Clinically, it may present as pain, breast enlargement, diffuse thickening, or palpable thickening behind the nipple.
Three patterns of gynecomastia have been described: nodular, dendritic, and diffuse.
Common mammographic appearance is a triangular- or flame-shaped density present behind the nipple or diffuse-increased density.
Gynecomastia may be unilateral or bilateral.
Some causes of gynecomastia include:
Idiopathic
Drugs: marijuana, thiazides, reserpines, cardiac glycosides, and cimetidine
Testicular tumors: embryonal cell carcinoma, seminoma, and choriocarcinoma
Klinefelter’s disease
Chronic hepatic disease
Exogenous estrogen administration
References
Applebaum AH, Evans GF, Levy KR, Amirkhan RH, Schumpert TD. Mammographic appearance of male breast disease. Radiographics. 1999;19:559–68.
Kopans DB. Breast imaging. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1998. p. 497, 501–2.
Mandell J. Core radiology: a visual approach to diagnostic imaging. 1st ed. Cambridge: Cambridge University Press; 2013. p. 651.
Case 7 Atypical Lobular Hyperplasia (ALH)
Patient History
A 49-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 (a) Spot-magnification CC and (b) spot-magnification LM views demonstrate grouped amorphous and heterogeneous calcifications at 12 o’clock at anterior depth.
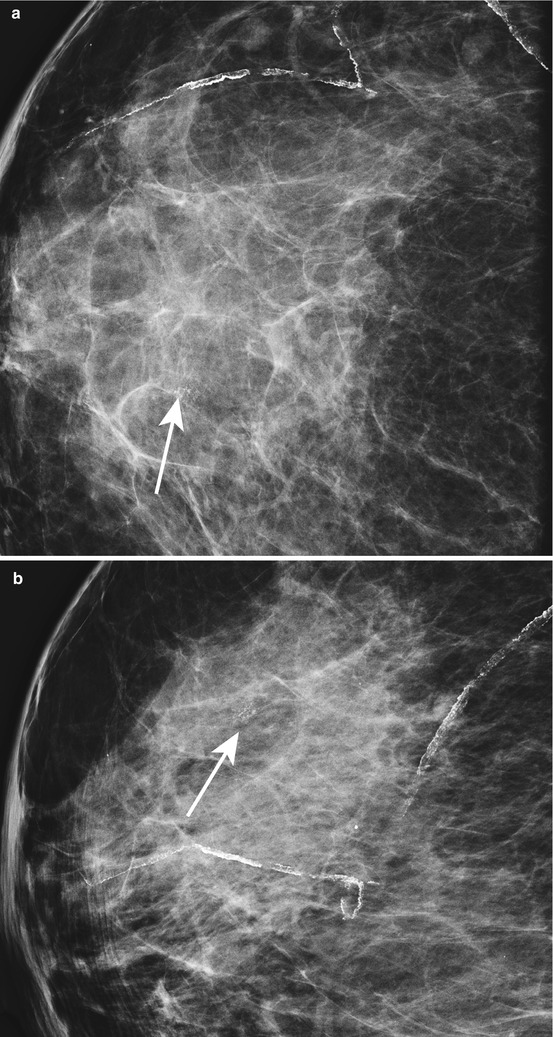
Fig. 1.1
Assessment
High-risk lesion.
Diagnosis
Atypical lobular hyperplasia (ALH)
Discussion
ALH presents commonly as amorphous calcifications.
Usually incidentally found at biopsy.
ALH is a high-risk lesion associated with increased risk of malignancy in either breast.
Treatment continues to be controversial following diagnosis on core needle biopsy.
Excision is generally recommended following diagnosis of ALH on core needle biopsy.
With excision, upgrade rates to malignancy range from 0 to 23 %.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsy; 2006. Section IV-2, p. 74–5.
Foster M, Helvie M, Gregory N, Rebner M, Nees A, Paramagul C. Lobular carcinoma in situ or atypical lobular hyperplasia at core needle biopsy: is excisional biopsy necessary? Radiology. 2004;231:813–9.
Case 8 Sternalis Muscle
Patient History
A 40-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 (a, b) Bilateral CC views demonstrate flame-shaped densities medially.
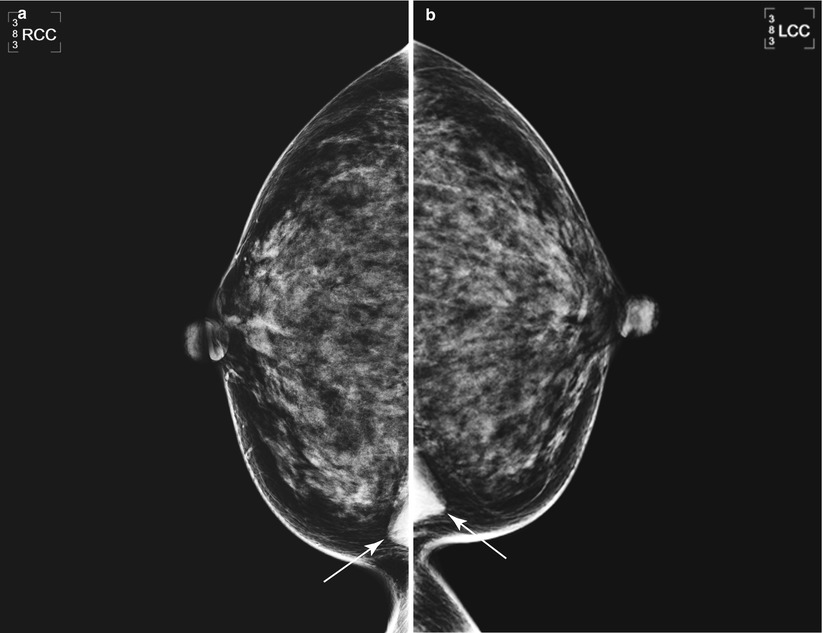
Fig. 1.1
BI-RADS Assessment
BI-RADS 1. Negative.
Diagnosis
Sternalis muscle
Discussion
Sternalis muscle is an anatomic variant of chest wall musculature.
Location is medial and parasternal.
It runs parallel to the sternum and perpendicular to the pectoralis muscle.
Sternalis muscle is seen only on CC views.
Sternalis muscle is triangular or rounded in shape.
Found in <10 % of individuals.
Twice as often unilateral as bilateral.
Main differential diagnosis is a medially located mass.
Location, shape, and lack of corresponding density on lateral views suggest the diagnosis.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-3, p. 40–1.
Bradley FM, Hoover HC Jr, Hulka CA, et al. The sternalis muscle: an unusual normal finding seen on mammography. AJR. 1996;166:33–6.
Kopans DB. Breast imaging. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1998. p. 9–10.
Mandell J. Core radiology: a visual approach to diagnostic imaging. 1st ed. Cambridge: Cambridge University Press; 2013. p. 638.
Case 9 Transverse Rectus Abdominis Myocutaneous (TRAM) Flap
Patient History
A 62-year-old female with a history of left mastectomy and reconstruction.
Radiology Findings
Fig. 1.1 MLO view demonstrates the typical appearance of a transverse rectus abdominis myocutaneous (TRAM) flap.
Fig. 1.2 CC view of a different patient demonstrates a large area of heterogeneous calcifications having a mass-like appearance.
Fig. 1.3 Axial nonfat suppressed T1-weighted image demonstrates that the central area of the left breast is isointense to the surrounding fat representing fat necrosis. This corresponds to the mammographic calcifications seen in Fig. 1.2.
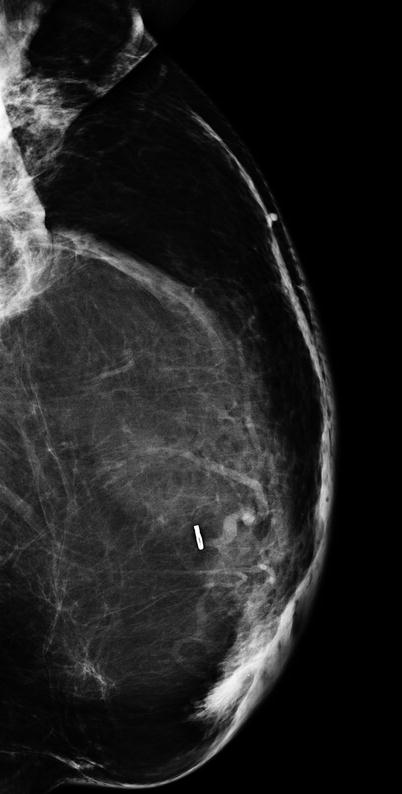
Fig. 1.1
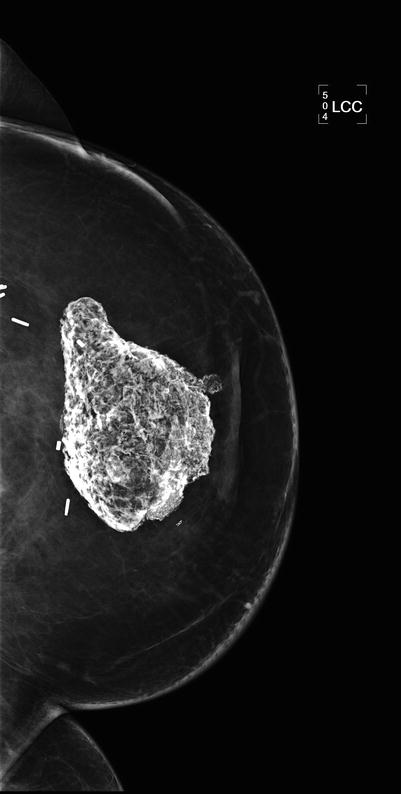
Fig. 1.2
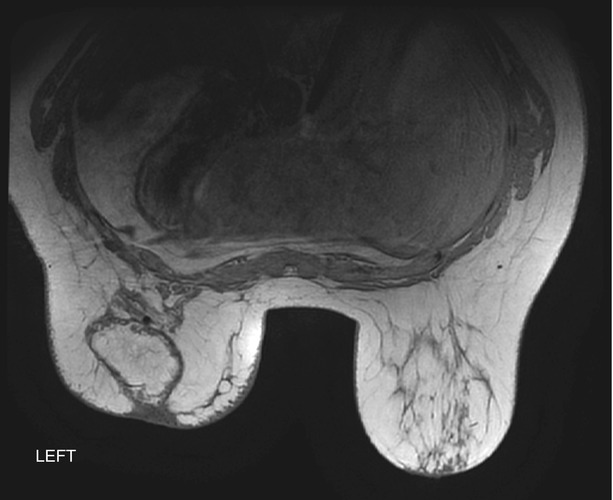
Fig. 1.3
BI-RADS Assessment
BI-RADS 2. Benign finding.
Diagnosis
TRAM flap
Discussion
A TRAM flap is a means of reconstruction following mastectomy or after implant removal.
There is a spectrum of myocutaneous flaps including the following:
TRAM flap
Latissimus dorsi myocutaneous (LDM) flap
Deep inferior epigastric perforator (DIEP) flap
Contraindications include the following:
Poor general health
Extensive abdominal scarring
Vascular disease
Locally advanced primary breast malignancy
Complications include the following:
Partial/complete loss of flap
Abdominal muscle weakness
Fat necrosis
Disease recurrence
Postreconstruction radiotherapy complications
Local recurrence rates are similar in patients with mastectomy and TRAM reconstruction vs. mastectomy alone.
TRAM screening is controversial.
Fat necrosis in a TRAM may present as a calcified mass.
Fat necrosis is commonly seen in the upper outer breast owing to decreased vascularity.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section V-3, p. 22–5.
Helvie MA, Bailey JE, Roubidoux MA, et al. Mammographic screening of TRAM flap breast reconstructions for detection of nonpalpable recurrent cancer. Radiology. 2002;222:211–6.
Case 10 Galactocele
Patient History
A 35-year-old female with a palpable mass in the left breast who recently stopped breast feeding.
Radiology Findings
Fig. 1.1 Spot magnification (a) CC and (b) MLO demonstrate an oval, low-density mass with circumscribed margins in the upper outer left breast at middle depth.
Fig. 1.2 ML view shows a fat–fluid level within the mass in the upper left breast at middle depth.
Fig. 1.3 Grayscale (a) transverse, (b) sagittal, and (c) color Doppler ultrasound images show an oval mass with a fluid–debris level.
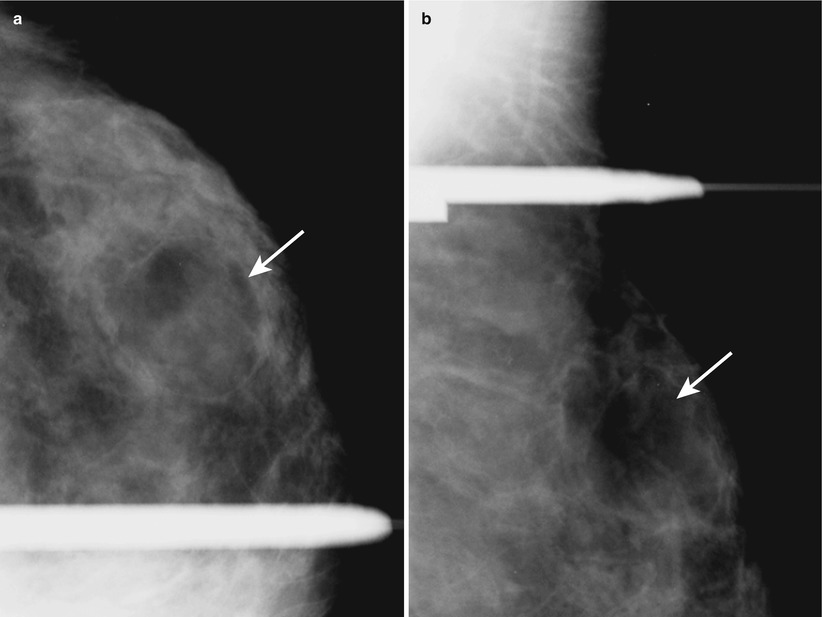
Fig. 1.1

Fig. 1.2
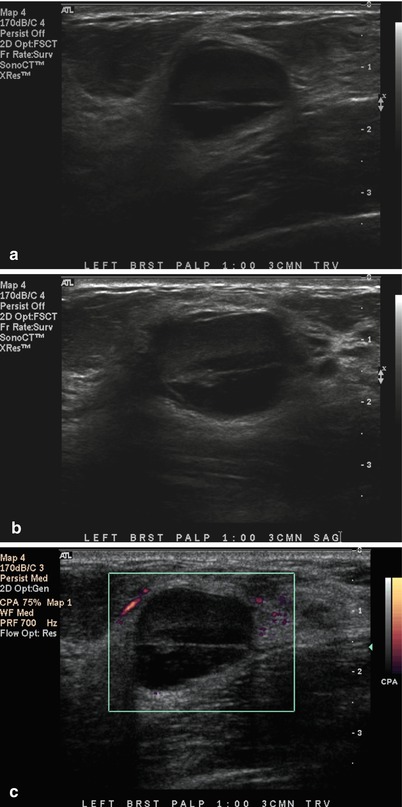
Fig. 1.3
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup).
Diagnosis
Galactocele
Discussion
A galactocele is a focal collection of breast milk.
On mammography, a galactocele presents as a low-density or equal-density mass with a fat–fluid level appreciated on the lateral mammogram.
On ultrasound, a fluid–debris level in the mass (fat rising to the top of the galactocele and milk/fluid layering dependently below) can be seen.
Typically seen in a lactating or postlactational woman.
Usually resolves spontaneously within a few weeks to months.
Aspiration can be performed for symptomatic relief.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-5, p. 6–9.
Ikeda DM. Breast imaging the requisites. 2nd ed. Philadelphia: Elsevier, Mosby; 2011. p. 379–80.
Mandell J. Core radiology: a visual approach to diagnostic imaging. 1st ed. Cambridge: Cambridge University Press; 2013. p. 623–4.
Case 11 Milk of Calcium
Patient History
A 45-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 (a) Spot-magnification CC and (b) MLO images show a cluster of round calcifications at 3 o’clock in the left breast at middle depth.
Fig. 1.2 Spot-magnification ML image of the left breast demonstrates the cluster of microcalcifications to have a curvilinear appearance.
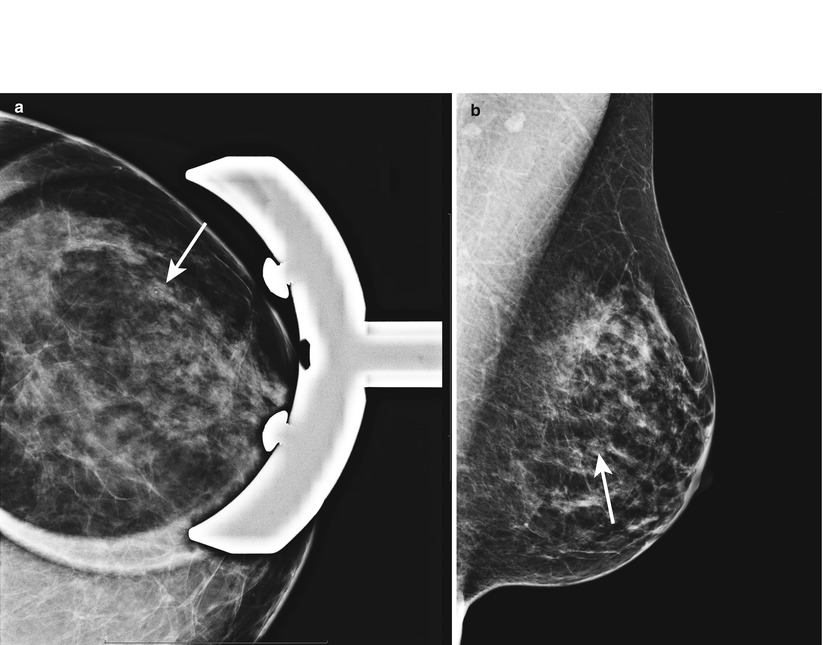
Fig. 1.1
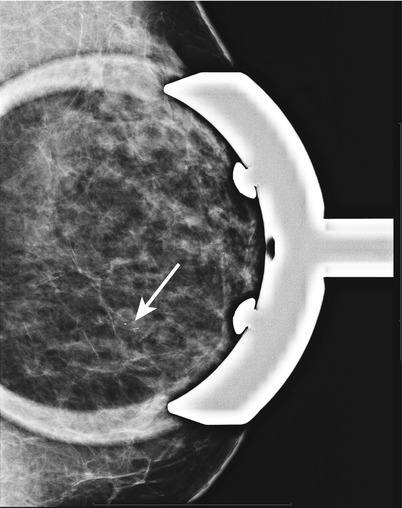
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign findings (following diagnostic workup).
Diagnosis
Milk of calcium
Discussion
Milk of calcium is sedimented calcium-oxalate calcifications within tiny benign cysts and dilated lobules.
Key diagnostic clue is the different shapes of calcifications between CC and lateral views.
Rounded or amorphous (“smudgy”) calcifications are seen on the CC view.
“Teacup,” linear, or crescent calcifications are seen on the lateral view.
Biopsy not warranted.
References
American College of Radiology (ACR) BI-RADS® Atlas. ACR BI-RADS® atlas-mammography. 5th ed. Reston: American College of Radiology; 2013. p. 55–7.
Berg WB, Birdwell RB, Gombos EC, et al. Diagnostic imaging: breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-1, p. 68–70.
Ikeda DM. Breast imaging the requisites. 2nd ed. Philadelphia: Elsevier, Mosby; 2011. p. 79–81.
Mandell J. Core radiology: a visual approach to diagnostic imaging. 1st ed. Cambridge: Cambridge University Press; 2013. p. 608.
Case 12 Lymphoma
Patient History
A 68-year-old female with an enlarging breast mass.
Radiology Findings
Fig. 1.1 (a) CC and (b) MLO images show an irregular mass with spiculated margins at 12 o’clock in the right breast at middle depth.
Fig. 1.2 Grayscale (a) transverse and (b) sagittal ultrasound images show an irregular hypoechoic mass surrounded by a hyperechoic rim.
Fig. 1.3 Color Doppler ultrasound image shows vascular flow within the mass.
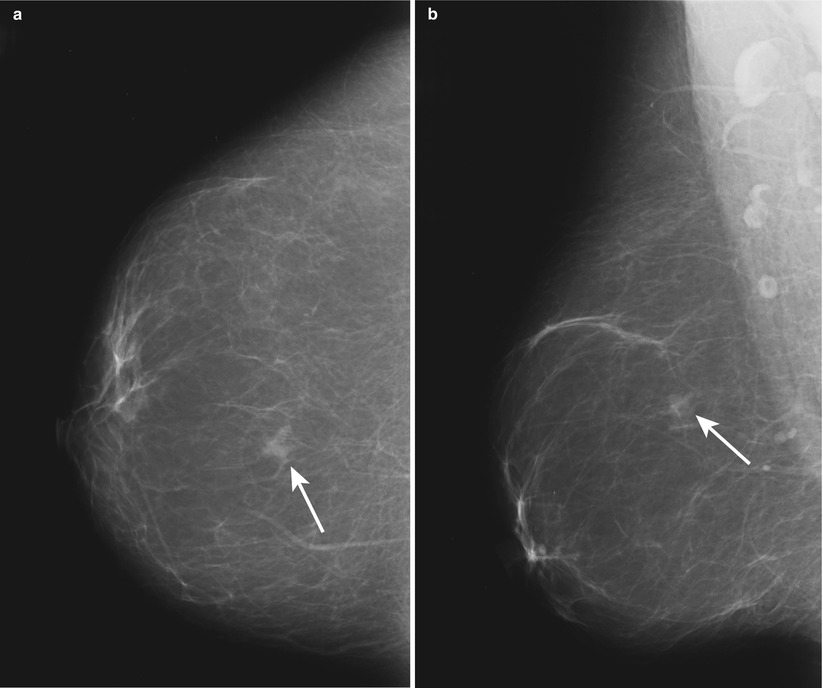
Fig. 1.1
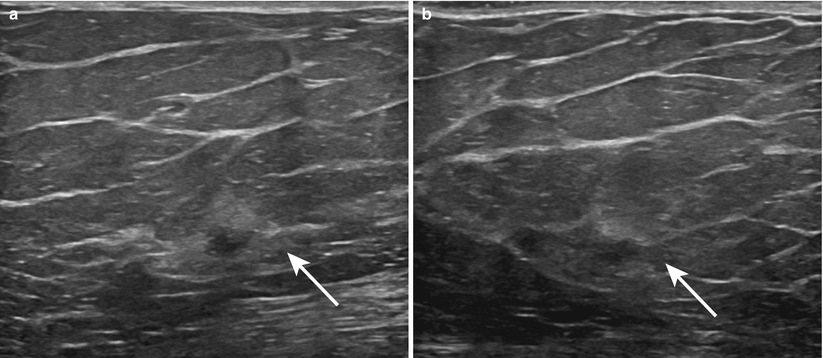
Fig. 1.2
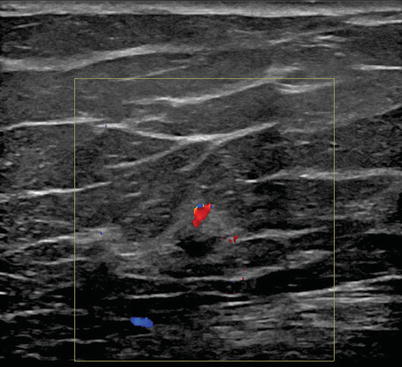
Fig. 1.3
BI-RADS Assessment
BI-RADS 5. Highly suggestive of malignancy (following diagnostic workup, prior to biopsy).
Diagnosis
Lymphoma
Discussion
Lymphoma accounts for approximately 0.1–0.2 % of all breast carcinomas.
Diagnosis of primary breast lymphoma is reserved for patients with no evidence of systemic lymphoma.
More commonly lymphoma occurs in the breast due to metastasis of extramammary lymphoma.
Mammographically, lymphoma can be seen as a solitary noncalcified mass, often well marginated and less often irregular.
A hypoechoic mass with indistinct margins and vascular flow is commonly seen on ultrasound.
On MRI, lymphoma is often seen as intense heterogeneous enhancement with a washout kinetic curve (type III).
References
Feder JM, Shaw de Paredes E, Hogge JP, Wilken JJ. Unusual breast lesions: radiologic-pathologic correlation. Radiographics. 1999;19:S11–26.
Yang WT, Lane DL, Le-Petross HT, Abruzzo LV, Macapinlac HA. Breast lymphoma: imaging findings of 32 tumors in 27 patients. Radiology. 2007;245:692–702.
Case 13 Fibroadenoma
Patient History
A 29-year-old female with a palpable mass at 12 o’clock in the left breast.
Radiology Findings
Fig. 1.1 (a) Grayscale and (b) color Doppler images show an oval circumscribed hypoechoic avascular mass at 12 o’clock, corresponding to the patient’s palpable mass.
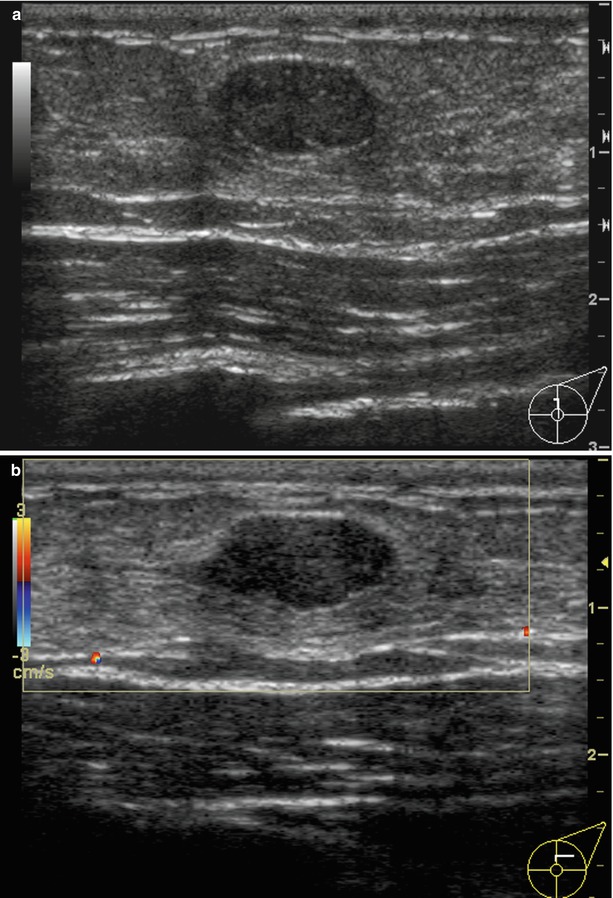
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup and biopsy).
Diagnosis
Fibroadenoma
Discussion
Fibroadenoma is a benign fibroepithelial tumor with mixed stromal and epithelial elements.
Juvenile-type fibroadenoma:
Is a “cellular” fibroadenoma
Has no leaflike growth pattern on pathology (which is a differentiating factor from phyllodes tumor)
Has a uniform stromal hypercellularity
Is usually seen between 10 and 20 years of age and rare in >45 years of age
Adult-type fibroadenoma:
Most common type
On pathology, has bland, fibroblastic stroma.
Is hypocellular to variably hypercellular.
Most fibroadenomas in teenagers are adult type.
Most commonly presents as a palpable, painless, mobile, firm mass.
Biopsy is indicated if it is new, enlarging, and palpable or has suspicious features. Otherwise, clinical and sonographic follow-up may be adequate.
Cryoablation therapy can be considered as an alternative treatment.
References
Berg WA, Birdwell RB, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-2, p. 32–7.
Cyrlak D, Pahl M, Carpenter SE. Breast imaging case of the day. Radiographics. 1999;19:549–51.
Mandell J. Core radiology: a visual approach to diagnostic imaging. 1st ed. Cambridge: Cambridge University Press; 2013. p. 625.
Case 14 Paget’s Disease
Patient History
A 58-year-old female with nipple erythema and retraction.
Radiology Findings
Fig. 1.1 (a) CC, (b) ML, (c) spot-magnification CC, and (d) spot-magnification MLO images show indistinct calcifications in a linear distribution, extending from the nipple to middle depth in the right breast. The nipple is inverted.
Fig. 1.2 (a) Axial subtracted T1-weighted and (b) sagittal contrast-enhanced delayed T1-weighted images show non-mass-like enhancement extending from the nipple to the posterior depth of the right breast. There is abnormal enhancement of the nipple–areolar complex.
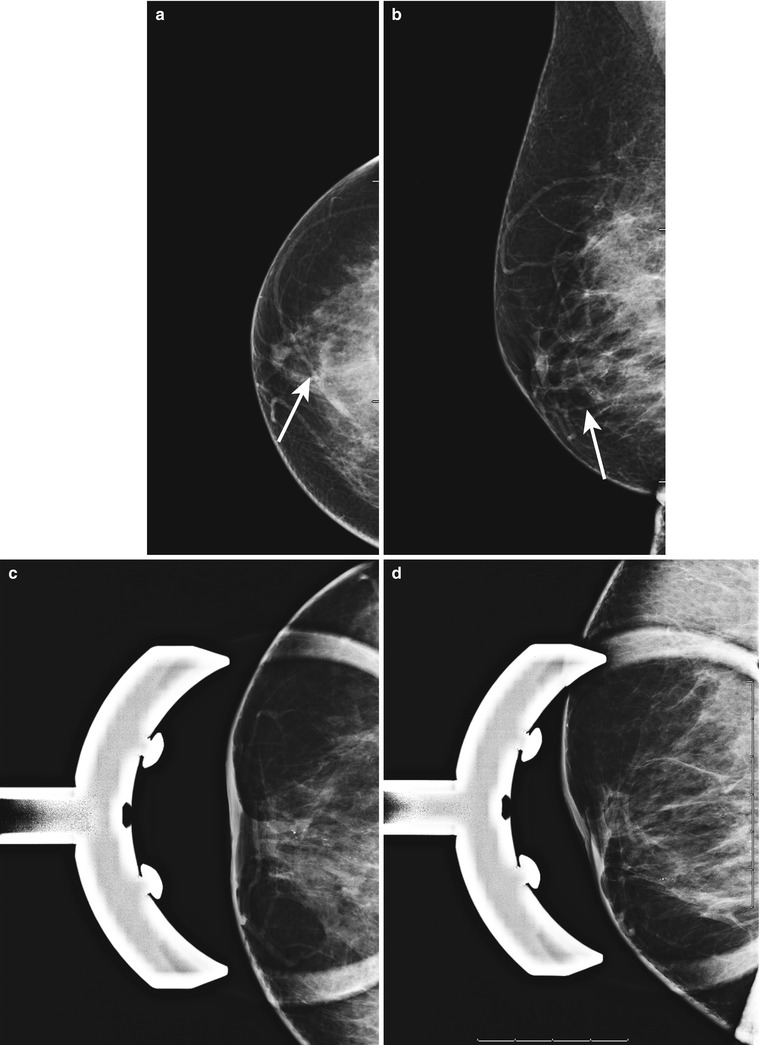
Fig. 1.1
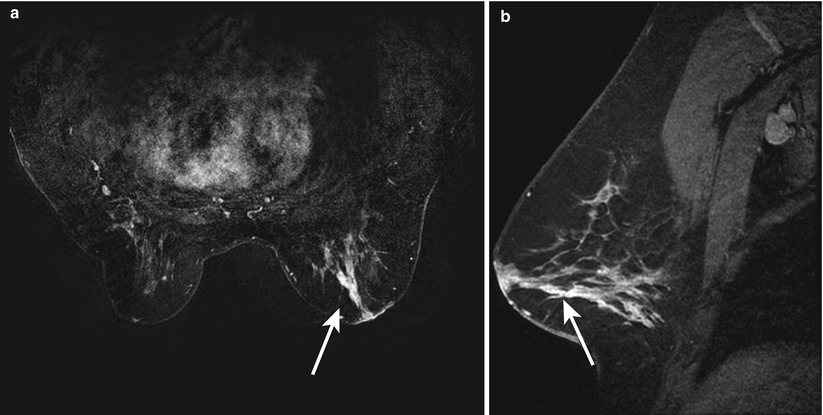
Fig. 1.2
BI-RADS Assessment
BI-RADS 5. Highly suggestive of malignancy (following diagnostic workup, prior to biopsy).
Diagnosis
Paget’s disease
Discussion
Paget’s disease is an extension of carcinoma to the epidermal layers of the nipple.
Often associated with an underlying DCIS and less commonly with IDC.
Clinically, Paget’s disease presents as scaling, erosions, erythema, or eczematous reaction of the nipple.
Mammogram can often be negative; however, calcifications or a mass associated with an underlying DCIS or IDC can be seen.
Skin thickening and heterogeneity of the breast parenchyma can be seen on ultrasound; the same nonspecific changes can be seen with mastitis.
MRI can be of value when the mammogram is normal, often showing abnormal nipple enhancement, thickening of the nipple–areolar complex, or an enhancing underlying carcinoma.
Diagnosis can be made by a punch biopsy of the nipple–areolar complex, which will demonstrate cancer cells.
Paget’s disease can be rarely associated with invasive lobular carcinoma.
References
Harvey JA, March DE. Making the diagnosis: a practical guide to breast imaging. Philadelphia: Elsevier; 2013. p. 375.
Kopans DB. Breast imaging. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1998. p. 583–4.
Nicholson BT, Harvey JA, Cohen MA. Nipple-areolar complex: normal anatomy and benign and malignant processes. Radiographics. 2009;29:509–23.
Case 15 Mastitis
Patient History
A 51-year-old male with swelling and erythema of the left breast following a human bite to the left breast.
Radiology Findings
Fig. 1.1 (a) CC and (b) MLO images show an asymmetry in the central anterior left breast.
Fig. 1.2 (a, b) Grayscale and (c) color Doppler ultrasound images show skin thickening and edematous tissue.
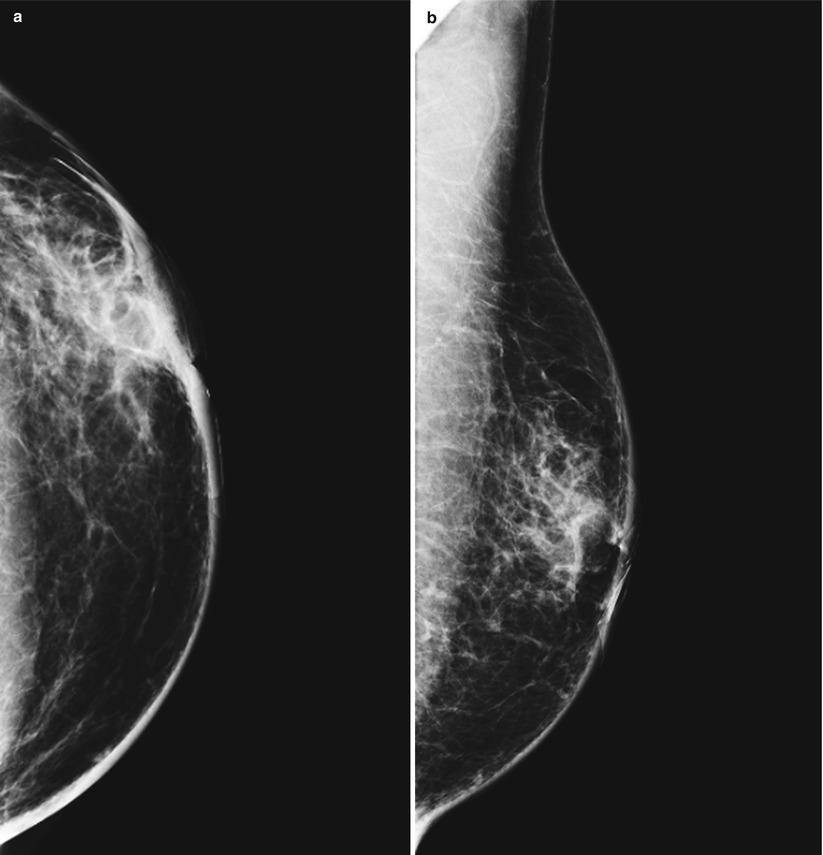
Fig. 1.1
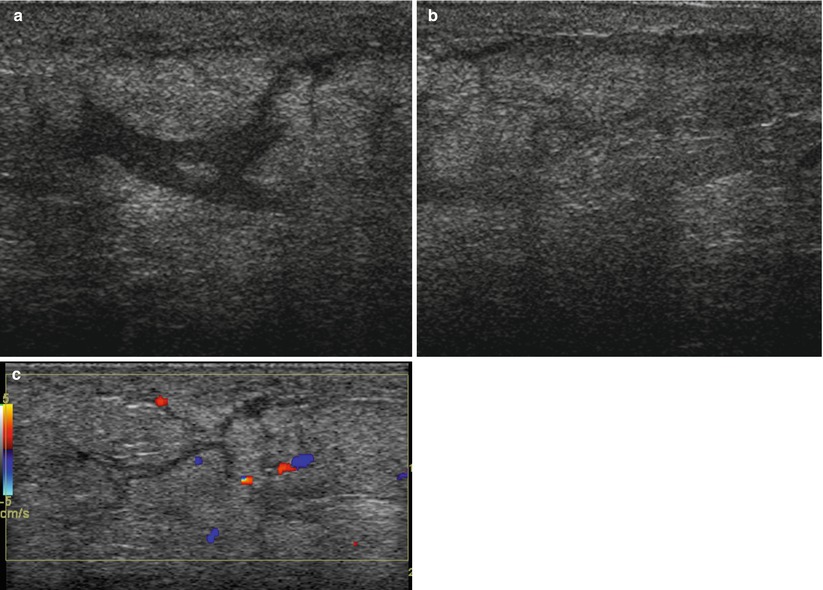
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign findings (following diagnostic workup).
Diagnosis
Mastitis
Discussion
Mastitis can present with pain, skin edema, erythema, and a palpable mass.
Mammographically, it can be seen as skin thickening and trabecular thickening, with or without an area of asymmetry in the breast.
Reactive lymphadenopathy can be present.
Skin thickening, edema, and increased echogenicity of the breast can be seen on ultrasound.
Most common pathogens are Staphylococcus aureus and Streptococcus.
Puerperal mastitis is most common.
A skin-punch biopsy is needed to differentiate inflammatory breast cancer from mastitis refractory to treatment.
References
Bassett LW, Feig SA, Hendrick RE, Jackson VP, Sickles EA. Breast disease (third series) test and syllabus. Reston: American College of Radiology; 2000. p. 82.
Berg W, Birdwell R, Gombos EC, et al. Diagnostic imaging: breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-6, p. 10–2.
Case 16 Neurofibromatosis Type I (NF I)
Patient History
A 52-year-old female with multiple skin lesions for screening mammogram.
Radiology Findings
Fig. 1.1 (a, b) CC and (c, d) MLO views show multiple circumscribed skin masses bilaterally.
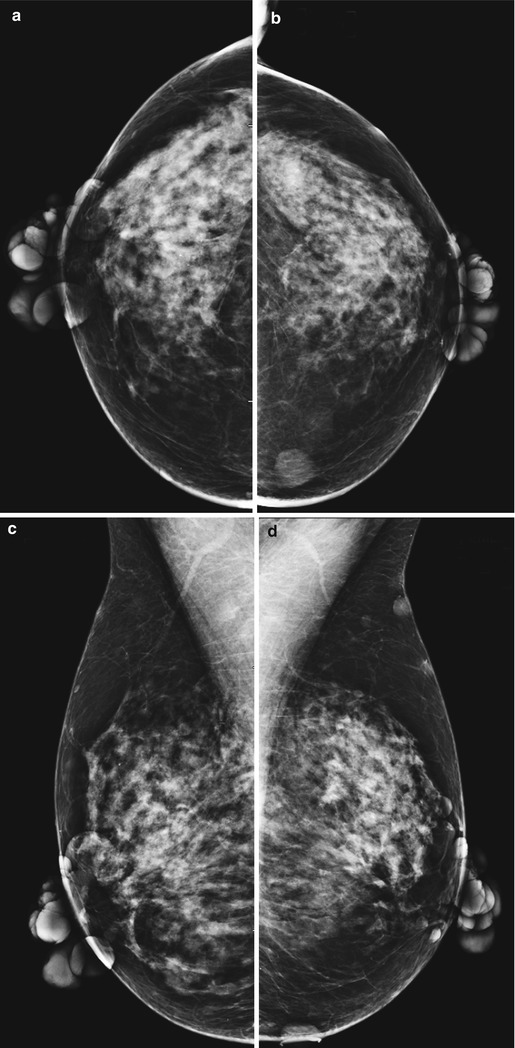
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign findings.
Diagnosis
Neurofibromatosis Type I (NF I)
Discussion
NF I, also termed as von Recklinghausen’s disease, presents initially in children and young adults.
Classic features of NF I include neurofibromas and cafe au lait spots.
NF I also has vascular, skeletal, and pulmonary manifestations.
Associated neoplasms with NF I include meningiomas, optic gliomas, neurofibrosarcomas, and pheochromocytomas.
Likely associated with an increased risk for breast cancer.
Neurofibromas can project over the breast and have the appearance of masses within the breast on mammogram.
References
Brant WE, Helms CA, editors. Fundamentals of diagnostic radiology. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1999. p. 430.
Harvey JA, March DE. Making the diagnosis: a practical guide to breast imaging. Philadelphia: Elsevier; 2013. p. 352.
Case 17 Multiple, Bilateral Circumscribed Masses
Patient History
A 42-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 (a, b) Bilateral CC views demonstrate multiple, bilateral, noncalcified circumscribed masses.
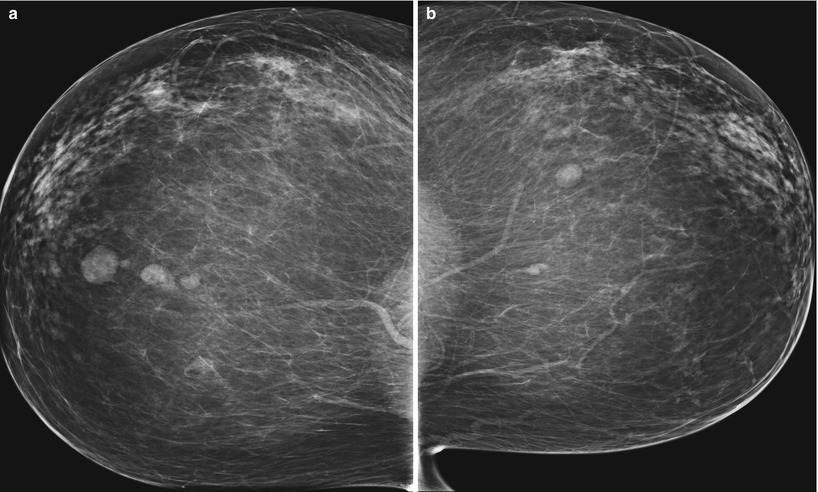
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign findings.
Diagnosis
Multiple, bilateral circumscribed masses
Discussion
Multiple, bilateral masses are defined as at least three masses in total with at least one in each breast.
Multiple masses are seen in 1.7 % of screening mammograms.
Margins must be 75 % circumscribed and the remainder can be obscured.
No mass can have spiculated margins.
Excludes palpable masses and those with suspicious calcifications.
Interval cancer rate associated with multiple, bilateral masses is 0.14 %.
Ultrasound is indicated if any mass is palpable, rapidly growing, or has an otherwise suspicious appearance.
Differential diagnosis includes:
Cysts
Fibroadenomas
Papillomas
Oil cysts
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-5, p. 22–5.
Leung JW, Sickles EA. Multiple bilateral masses detected on screening mammography: assessment of need for recall imaging. AJR. 2000;175:23–9.
Case 18 Vascular Calcifications
Patient History
A 74-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 Bilateral (a, b) CC and (c, d) MLO views demonstrate linear, serpiginous, parallel calcifications.
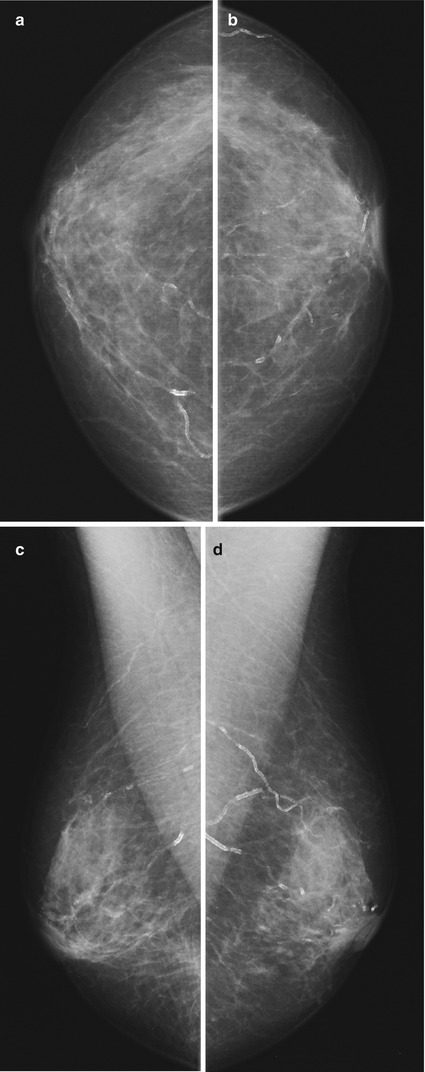
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign finding.
Diagnosis
Vascular calcifications
Discussion
Vascular calcifications are calcifications within the media of the arterial wall.
Classic “tram track” pattern.
Seen in 8–9 % of all screening mammograms.
Increased frequency with advancing age.
Vascular calcifications are more common in women with diabetes and renal dialysis.
Some studies have shown that breast arterial calcifications are an independent risk factor for cardiovascular mortality.
Atypical vascular calcifications may mimic malignancy.
No specific breast-related treatment.
If not a classic appearance, differential diagnosis includes:
DCIS
Secretory calcifications
Mondor’s disease
Fat necrosis
References
American College of Radiology (ACR) BI-RADS® Atlas. ACR BI-RADS® atlas-mammography. 5th ed. Reston: American College of Radiology; 2013. p. 40–1.
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-1, p. 76–8.
Kemmeren J, Beijerinck D, van Noord PA, et al. Breast arterial calcifications: association with diabetes mellitus and cardiovascular mortality. Work in progress. Radiology. 1996;201:75–8.
Moshyedi AC, Puthawala AH, Kurland RJ, O’Leary DH. Breast arterial calcifications: association with coronary artery disease. Work in progress. Radiology. 1995;194:181–3.
Case 19 Stromal Fibrosis
Patient History
A 60-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 (a) CC and (b) MLO views demonstrate an oval mass with partly circumscribed and partly ill-defined margins in the lower inner left breast at posterior depth.
Fig. 1.2 Grayscale ultrasound image demonstrates a hypoechoic oval mass with ill-defined margins and posterior acoustic shadowing.
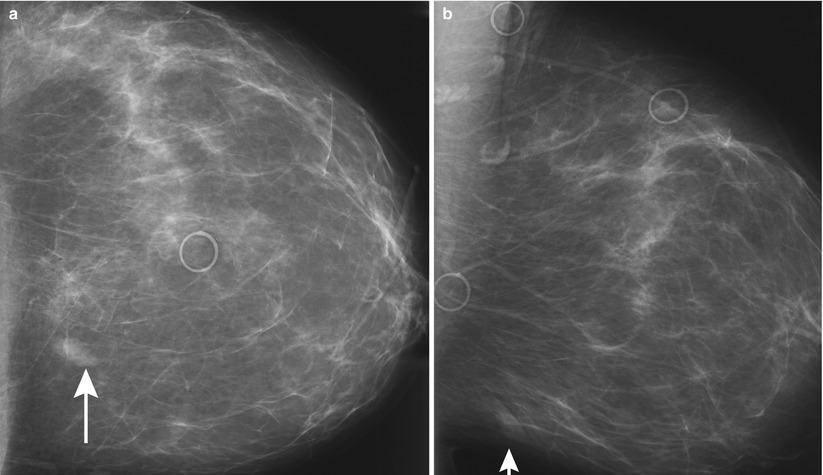
Fig. 1.1
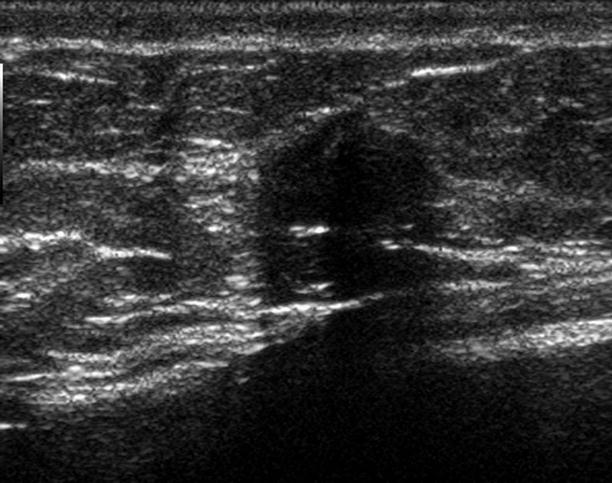
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup and biopsy).
Diagnosis
Stromal fibrosis
Discussion
Stromal fibrosis may present incidentally on imaging or as a palpable mass.
Formed by proliferation of collagenized stroma between terminal ductal lobular units.
On mammography, stromal fibrosis can present as a benign-appearing mass or lesion that has features suggestive of malignancy.
On ultrasound, stromal fibrosis appears hypoechoic or of mixed echogenicity and is nonvascular.
No malignant potential and no intervention are necessary.
It is important to assess radiology/pathology concordance after a diagnosis of stromal fibrosis on core needle biopsy.
If concordant, 6-month follow-up may be performed to assess stability.
Discordance between imaging features and diagnosis of stromal fibrosis should result in rebiopsy or excision.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-2, p. 46–9.
Sklair-Levy M, Samuels TH, Catzavelos C, Hamilton P, Shumak R. Stromal fibrosis of the breast. AJR. 2001;177(3):573–7.
Case 20 Reduction Mammoplasty
Patient History
A 51-year-old female with a history of prior bilateral breast surgery for a screening mammogram.
Radiology Findings
Fig. 1.1 Bilateral (a, b) CC and (c, d) MLO views demonstrate prominent fibroglandular tissue with a swirled pattern of architectural distortion in the lower breast. An oval lucent mass in the lower inner breast represents fat necrosis.
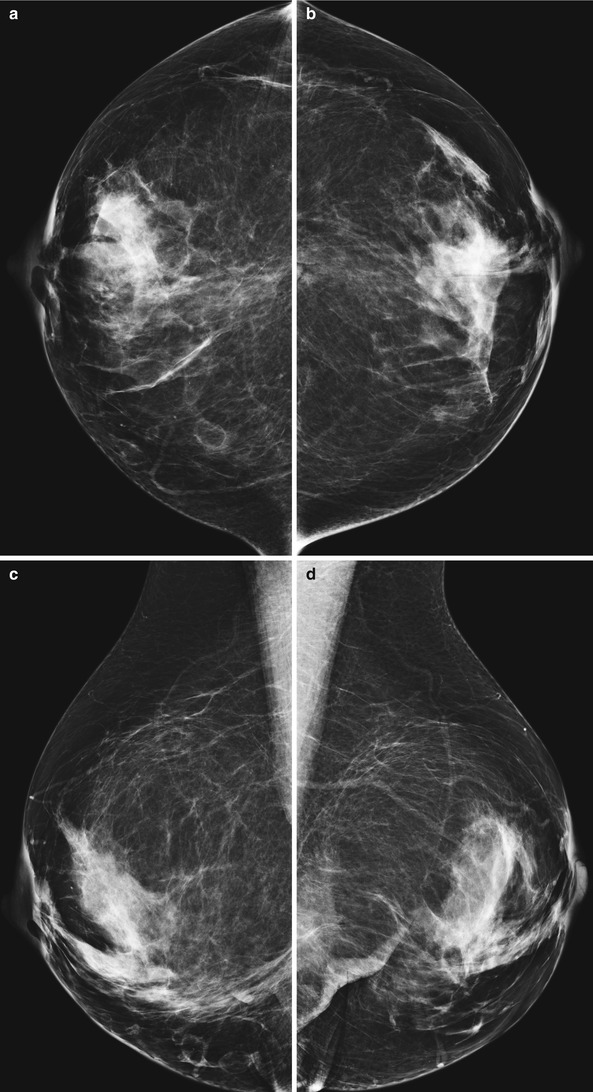
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign finding.
Diagnosis
Reduction mammoplasty
Discussion
Reduction mammoplasty is a plastic surgery procedure to decrease the breast size in macromastia, in the setting of contralateral mastectomy or breast conservation surgery, trauma, or congenital asymmetry. A keyhole incision is usually made.
Characteristic mammographic findings include:
Elevation of nipple with more skin inferior than superior.
Redistribution of fibroglandular tissue from upper outer quadrant to lower inner quadrant.
“Swirled pattern” of fibroglandular tissue in the lower inner quadrant.
Dermal calcifications are common in the scar tissue.
The breasts appear higher and flatter in contour than normal breasts.
Associated findings include:
Fat necrosis
Postsurgical skin thickening
Sutural calcifications
Retroareolar fibrotic band
Baseline mammogram is generally performed prior to the surgery to evaluate for any suspicious masses or calcifications.
Mammogram is recommended 3–6 months postoperatively, which becomes the new baseline.
References
Bassett LW, Jackson VP, Fu KL, Fu YS. Diagnosis of diseases of the breast. 2nd ed. Philadelphia: Elsevier; 2005. p. 617–21.
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-4, p. 32–4.
Harvey JA, March DE. Making the diagnosis: a practical guide to breast imaging. Philadelphia: Elsevier; 2013. p. 470–2.
Case 21 Invasive Lobular Carcinoma (ILC)
Patient History
A 66-year-old female for a screening mammogram.
Radiology Findings
Fig. 1.1 (a) CC, (b) MLO, and (c) LM images show an area of architectural distortion in the upper inner left breast at posterior depth.
Fig. 1.2 (a) Grayscale and (b) color Doppler ultrasound images show a lobular hypoechoic mass with spiculated margins. There is vascular flow within the mass.
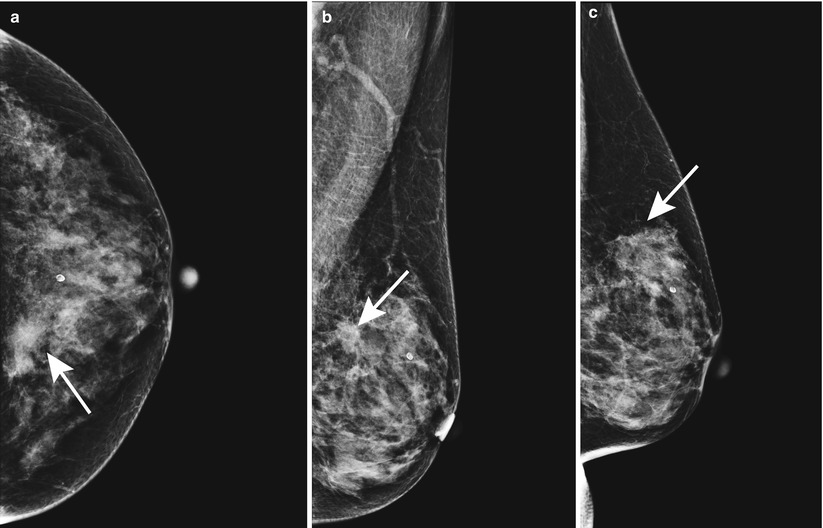
Fig. 1.1
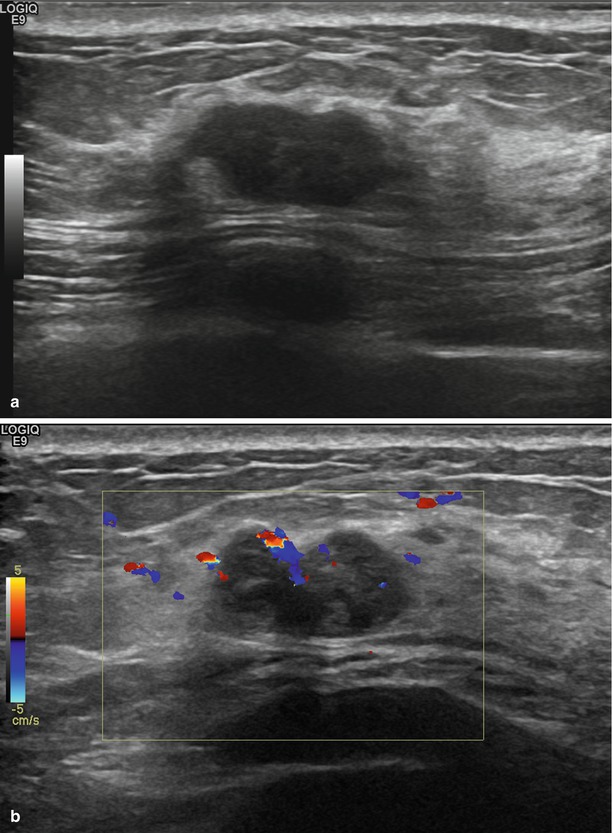
Fig. 1.2
BI-RADS Assessment
BI-RADS 4. Suspicious abnormality (following diagnostic workup, prior to biopsy).
Diagnosis
Invasive lobular carcinoma (ILC)
Discussion
ILC arises from the lobular epithelium.
It is the second most common breast cancer and accounts for 10–15 % of all invasive breast malignancies.
Malignant cells grow in single file, and therefore, ILC does not evoke a desmoplastic reaction.
On mammogram, ILC may be difficult to detect due to its growth pattern, decreased likelihood to develop calcifications, and atypical presentation such as a single-view finding of architectural distortion.
ILC is seen as an ill-defined or spiculated mass on mammogram in 45–65 % of the cases.
Usually detected at a later stage mammographically and clinically, thus increasing the likelihood of a large primary tumor and positive axillary lymph nodes at the time of diagnosis.
When ILC is large, the breast may appear smaller on mammogram owing to decreased compressibility of the breast from the sheets of tumor cells, commonly referred to as the “shrinking breast.”
ILC can metastasize to peritoneal surfaces, bladder, stomach, uterus, and ovaries, thus causing presenting symptoms of ascites, pelvic masses, or hydronephrosis.
A high rate of false-negative findings with PET has been reported with ILC.
References
Avril N, Rose CA, Schelling M, et al. Breast imaging with PET and fluorine-18 fluorodeoxyglucose: uses and limitations. J Clin Oncol. 2000;18:3495–502.
Breas RF, Ioffe M, Rapelyea JA, et al. ILC: detecting with mammography, sonography, MRI and breast specific gamma imaging. AJR. 2009;192:379–83.
Harvey JA. Unusual breast cancers: useful clues to expanding the differential diagnosis. Radiology. 2007;242:638–94.
Harvey JA, March DE. Making the diagnosis: a practical guide to breast imaging. Philadelphia: Elsevier; 2013. p. 295.
Lopez JK, Bassett LW. ILC of the breast: spectrum of mammographic, ultrasound and MRI imaging findings. Radiographics. 2009;29:165–76.
Sickles EA. The subtle and atypical mammographic features of invasive lobular carcinoma. Radiology. 1991;178:25–6.
Case 22 Lactating Adenoma
Patient History
A 30-year-old pregnant female with a palpable mass in the right breast.
Radiology Findings
Fig. 1.1 Grayscale (a) transverse and (b) sagittal ultrasound images show a gently lobulated circumscribed hypoechoic mass.
Fig. 1.2 Color Doppler ultrasound image shows no vascular flow within the mass.
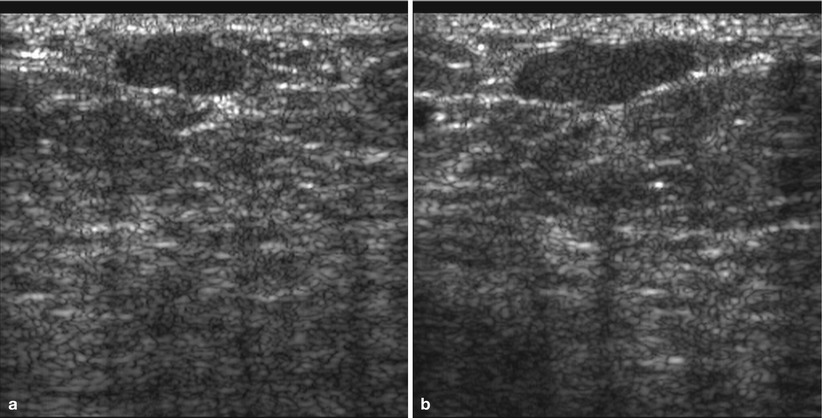
Fig. 1.1
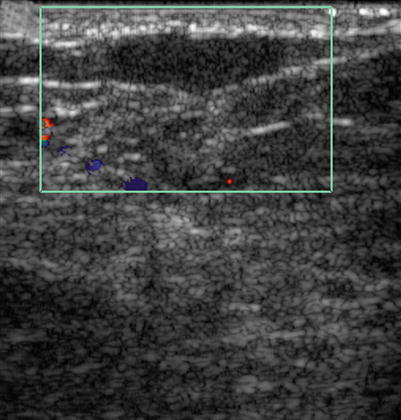
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup and biopsy).
Diagnosis
Lactating adenoma
Discussion
Lactating adenoma is a benign breast mass thought to occur in response to the physiologic changes seen in pregnancy and lactation.
There is often spontaneous regression of a lactating adenoma following pregnancy and lactation.
Lactating adenoma is a fibroepithelial lesion that is similar in imaging and histologic appearance to a fibroadenoma.
On mammogram, a circumscribed mass with a benign appearance is seen.
On ultrasound, a circumscribed hypoechoic mass is commonly seen.
Less frequently, a lactating adenoma with spiculated margins and posterior acoustic shadowing is seen by ultrasound, suggesting malignancy.
Radiolucent or hyperechoic areas can be seen on mammogram and ultrasound, respectively, representing the fat content of milk secondary to lactational hyperplasia.
References
Chung EM, Cube R, Hall GJ, Gonzalez C, Stocker JT, Glassman LM. Breast masses in children and adolescents: radiologic-pathologic correlation. Radiographics. 2009;29:907–31.
Harvey JA, March DE. Making the diagnosis: a practical guide to breast imaging. Philadelphia: Elsevier; 2013. p. 303.
Sabate JM, Clotet M, Torrubia S. Radiologic evaluation of breast disorders related to lactation and pregnancy. Radiographics. 2007;27:S101–124.
Case 23 Silicone Granuloma
Patient History
A 50-year-old female with a history of removal of ruptured silicone implants.
Radiology Findings
Fig. 1.1 (a) CC and (b) MLO views demonstrate a dense irregular mass in the lower inner right breast at posterior depth.
Fig. 1.2 Grayscale ultrasound image demonstrates a “snowstorm” appearance.
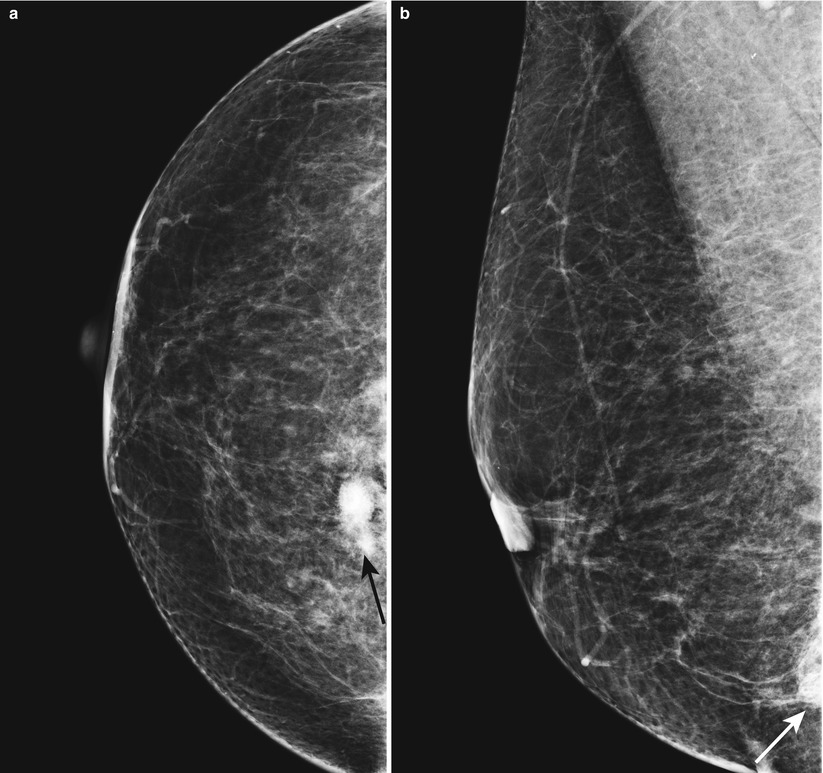
Fig. 1.1
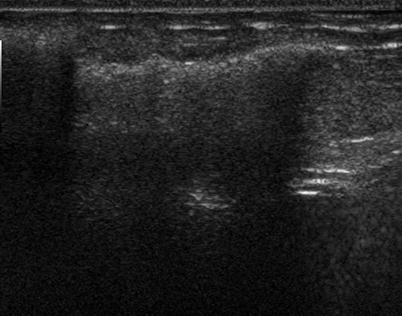
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup).
Diagnosis
Silicone granuloma
Discussion
Silicone granuloma is a mass caused by foreign body reaction to free silicone in tissues.
Most common locations are at the edge of implants and axilla.
They are usually easy to recognize due to their high density. Their margins may be circumscribed or indistinct.
Patients may be asymptomatic or present with a palpable mass.
Silicone in an axillary node is an indication of extracapsular implant rupture.
Presence of silicone granulomas indicates extracapsular rupture of a current or prior implant.
If asymptomatic, no treatment is necessary. If symptomatic, supportive therapy and/or excision is recommended.
Silicone in the axilla can involve the brachial plexus causing neuropathy.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section: IV-4, p. 36–7.
Caskey C, Berg WA, Hamper UM, Sheth S, Chang BW, Anderson ND. Imaging spectrum of extracapsular silicone: correlation of ultrasound, MR. imaging, mammographic and histopathologic findings. Radiographics. 1999;19:F39–51.
Harvey JA, March DE. Making the diagnosis: a practical guide to breast imaging. Philadelphia: Elsevier; 2013. p. 511–2.
Case 24 Lipoma
Patient History
A 58-year-old male with a palpable left breast mass for 1 month.
Radiology Findings
Fig. 1.1 (a) CC, (b) MLO, and (c) ML images show a radiolucent oval circumscribed mass, corresponding to a triangular marker indicating a palpable mass.
Fig. 1.2 Grayscale ultrasound image shows a nearly isoechoic oval circumscribed mass.
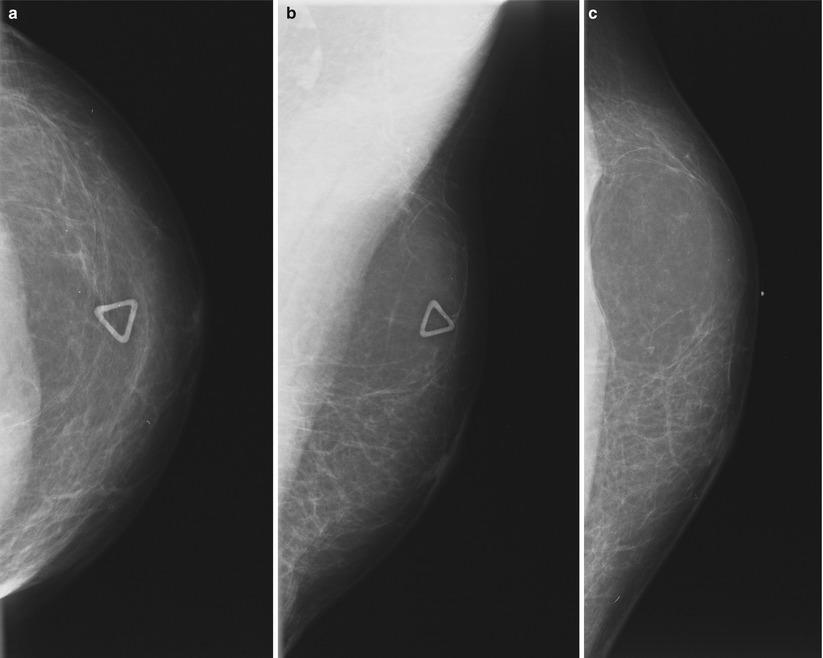
Fig. 1.1
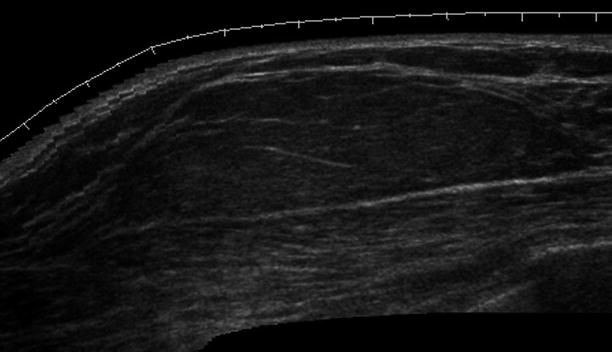
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign finding.
Diagnosis
Lipoma
Discussion
A lipoma is a benign fatty mass that presents as a radiolucent mass surrounded by a thin pseudocapsule on mammogram.
Clinically, lipomas are soft and mobile.
May distort the breast architecture on mammogram by displacing the adjacent normal breast tissue.
On ultrasound, a lipoma is seen as a hypoechoic, isoechoic, or hyperechoic oval or round circumscribed mass parallel to the skin, with an echotexture similar to the subcutaneous fat.
The diagnosis usually can be made on mammogram without the need for ultrasound.
References
Applebaum AH, Evans GF, Levy KR, Amirkhan RH, Schumpert TD. Mammographic appearance of male breast disease. Radiographics. 1999;19:559–68.
Kopans DB. Breast imaging. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 1998. p. 551–4.
Case 25 Adenoid Cystic Carcinoma
Patient History
A 47-year-old female with a history of focal left breast pain.
Radiology Findings
Fig. 1.1 (a) CC, (b) MLO, and spot-compression (c) CC and (d) ML views show an oval mass with partially obscured margins in the subareolar region of the left breast.
Fig. 1.2 (a) Grayscale and (b) color Doppler images show an oval circumscribed avascular mass in the subareolar region of the left breast.
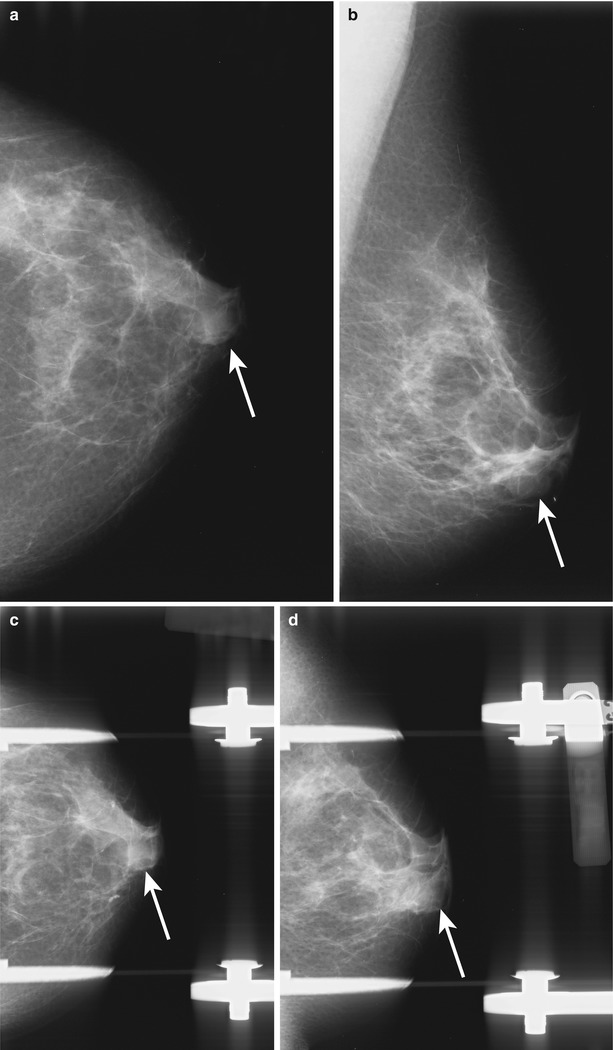
Fig. 1.1
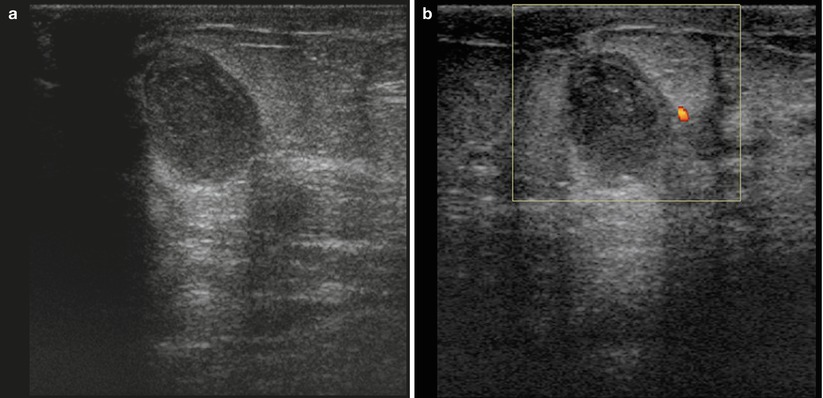
Fig. 1.2
BI-RADS Assessment
BI-RADS 4. Suspicious abnormality (following diagnostic workup, prior to biopsy).
Diagnosis
Adenoid cystic carcinoma
Discussion
Adenoid cystic carcinoma is a rare malignant breast tumor.
Typically, a slow-growing lobular mass is seen clinically.
Median size is 2 cm with a range between 0.2 and 12 cm.
Commonly seen in the subareolar or central region but can occur anywhere in the breast.
Excellent prognosis. Recurrence is possible if mass is not completely excised.
Imaging characteristics vary and range from a circumscribed mass to ill-defined mass or focal asymmetries.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-2, p. 102–3.
Ikeda DM. Breast imaging the requisites. 2nd ed. Philadelphia: Elsevier, Mosby; 2011. p. 131.
Santamarie G, Velasco M, Zanon G, et al. Adnoid cystic carcinoma of the breast: mammographic appearance and pathologic correlation. AJR. 1998;171:1679–83.
Case 26 Diabetic Mastopathy
Patient History
A 31-year-old female with a palpable mass in the retroareolar right breast. The patient is on dialysis.
Radiology Findings
Fig. 1.1 Bilateral (a, b) CC and (c, d) MLO, and right spot-compression (e) CC and (f) MLO views show no discrete mass. There is a focal asymmetry in the retroareolar right breast when compared with that of the left. There is a permacatheter incidentally seen in the upper right breast.
Fig. 1.2 (a, b) Grayscale and (c) color Doppler ultrasound images show a hypoechoic avascular mass with indistinct margins in the retroareolar region of the right breast, corresponding to the patient’s palpable mass.
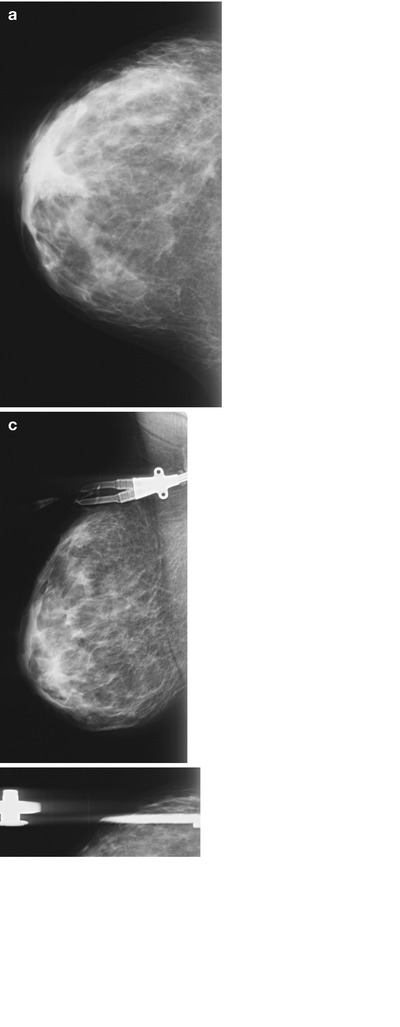
Fig. 1.1
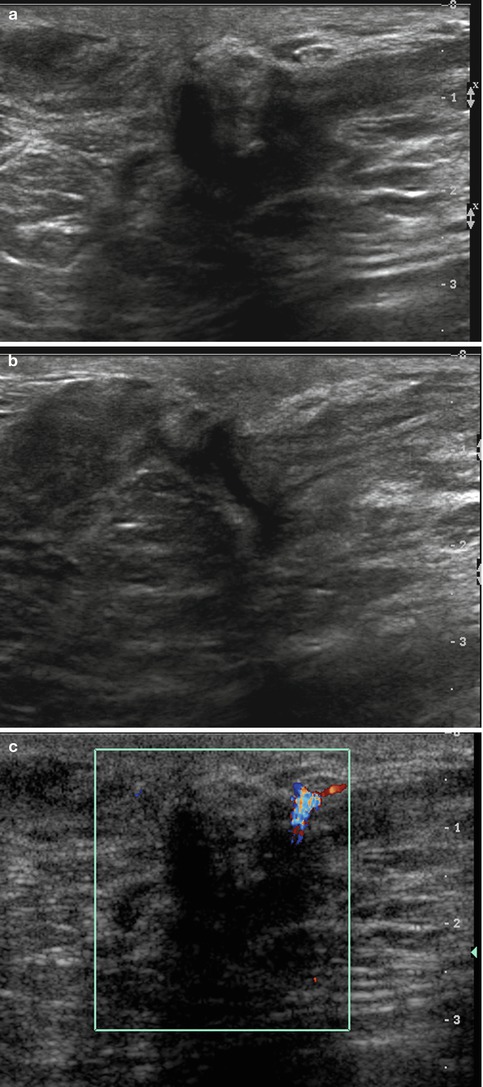
Fig. 1.2
BI-RADS Assessment
BI-RADS 2. Benign finding (following diagnostic workup and biopsy).
Diagnosis
Diabetic mastopathy
Discussion
Diabetic mastopathy is a variant of stromal fibrosis occurring in long-term insulin-dependent diabetics, in premenopausal women with long-standing insulin-dependent diabetes, or in rare patients with thyroid disease.
Diabetic mastopathy results from an autoimmune reaction to the accumulation of abnormal matrix proteins caused by hyperglycemia.
Clinical symptoms include palpable and firm, nontender masses, thickening of the breasts, or hard breasts.
On mammography, increased parenchymal density may be seen unilaterally or in both the breasts.
On ultrasound, a hypoechoic mass with indistinct margins can be seen.
A biopsy is needed to establish the diagnosis.
Excellent prognosis, self-limited.
References
Berg WA, Birdwell RL, Gombos EC, et al. Diagnostic imaging breast. 1st ed. Salt Lake City: Amirsys; 2006. Section IV-5, p. 30–1.
Ikeda DM. Breast imaging the requisites. 2nd ed. Philadelphia: Elsevier, Mosby; 2011. p. 400–1.
Sabate JM, Clotet M, Gomez A, De las Heras P, Torrubia S, Salinas T. Radiologic evaluation of uncommon inflammatory and reactive breast disorders. Radiographics. 2005;25:411–24.
Case 27 Diffuse Bilateral Breast Calcifications
Patient History
A 79-year-old female for a bilateral screening mammogram.
Radiology Findings
Fig. 1.1 (a, b) CC and (c, d) MLO views of both breasts show multiple diffuse secretory, vascular, round, and oval calcifications scattered diffusely bilaterally.
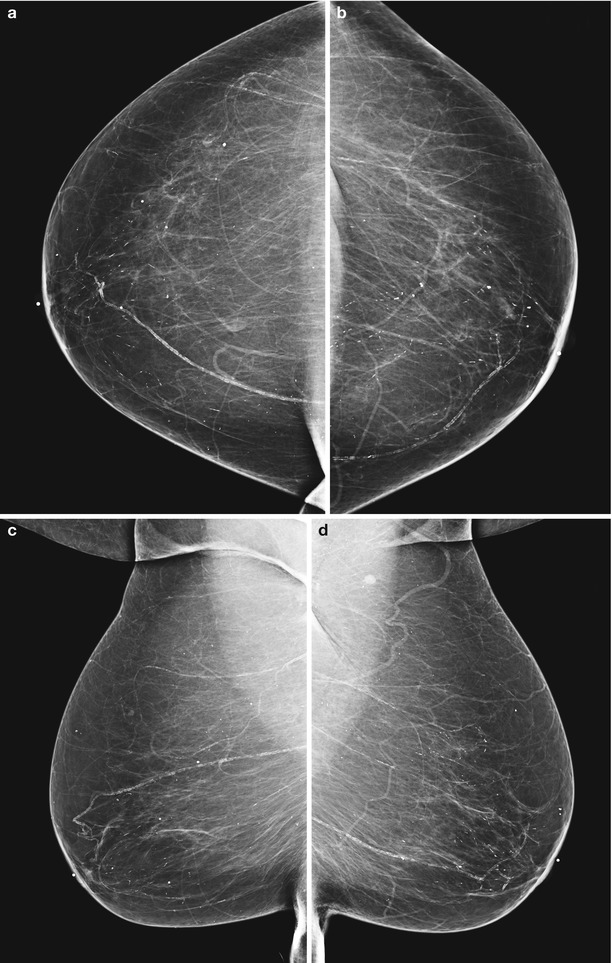
Fig. 1.1
BI-RADS Assessment
BI-RADS 2. Benign findings.
Diagnosis
Diffuse bilateral breast calcifications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree