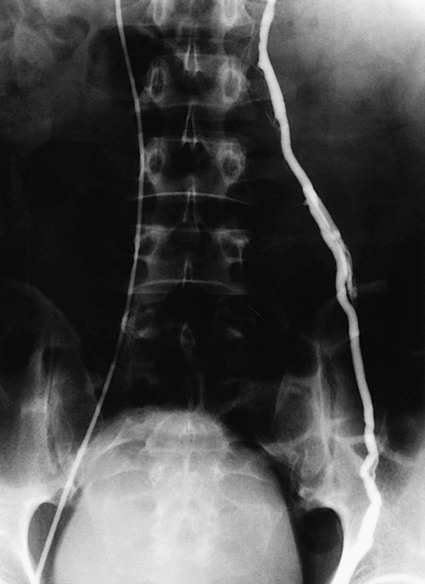
Bryan Grieme, Andrew Akman, Ali Albayati, Emily J. Timmreck, Emily M. Tanski and Anthony C. Venbrux Varicocele is most commonly diagnosed in the adult male population at a rate between 15% and 17%. The incidence occurs in less than 1% in boys younger than age 10 and then plateaus at 15% in late adolescence. Approximately 90% of varicoceles occur on the left side. The remaining 10% occur bilaterally. Gat et al. found an unusually high incidence of bilateral varicocele (80.7%; 210 of 255) in infertile men with varicocele, but only 21 of 210 (10%) right-sided varicoceles were palpable.1 The incidence of unilateral right-sided varicocele is 0.4%.2 The finding of an isolated right-sided varicocele warrants further evaluation. It can be associated with situs inversus, as well as with retroperitoneal and abdominal tumors such as lymphoma and metastases.3,4 Varicocele diagnosis is primarily made by clinical presentation and physical exam. The simple grading system of Dubin and Amelar5 is most commonly used: grade 0, not palpable; grade 1, palpable only with the patient standing and performing a Valsalva maneuver; grade 2, palpable without a Valsalva maneuver; and grade 3, visible. High-resolution real-time ultrasound and color-flow Doppler ultrasound may be used to either confirm the diagnosis or detect subclinical (nonpalpable) varicoceles. The significance of subclinical varicocele with regard to infertility is currently controversial.6–9 Doppler ultrasound may further distinguish between types of varicoceles and their blood flow characteristics.10 Because only palpable varicoceles have been documented to be associated with infertility, the Report on Varicocele and Infertility (published jointly by the Male Infertility Best Practice Committee of the American Urological Association and the Practice Committee of the American Society for Reproductive Medicine, September 2004) recommends that routine evaluation of infertile men with varicoceles include a medical and reproductive history, physical examination, and a minimum of two semen analyses, but imaging studies are only indicated if the physical exam is inconclusive.11 Spermatic venography is another imaging technique. It is generally reserved for venous mapping in preparation for transcatheter embolotherapy or surgical ligation12 (Fig. 79-1). Varicocele is seen in about 40% of men seeking evaluation for infertility. There is some controversy regarding the causal relationship of varicocele and infertility (e.g., 85% of men with varicoceles are fertile, and reports of improvement in pregnancy rate are inconsistent2,13–17). Significant evidence in the literature supports the hypothesis that varicoceles have a negative effect on the testis and fertility and that varicocele repair can reverse or prevent these effects.1,18–24 In a prospective trial, Laven et al. randomized 67 young adults with varicoceles to treatment (percutaneous embolotherapy) and nontreatment groups; 21 healthy male volunteers without varicoceles served as controls. One year after treatment, left testis volumes were measured and found to be comparable to those of the control group and significantly different (larger) (P < .001) from the untreated group. Semen quality (sperm concentration) increased significantly (P < .01) in the treated group and was unchanged in the untreated and control groups.25 The three primary indications for treatment of a varicocele are (1) subfertility or infertility in adult men, (2) varicocele and testicular atrophy in adolescent or pediatric-aged patients, and (3) pain. Recurrence of varicocele after surgical ligation is also an indication. The most common indication for treatment of a varicocele in an adult male is infertility/subfertility. Criteria for treatment in this group should include: (1) abnormal semen parameters, (2) absence of any other identifiable or correctable causes of male infertility, and (3) a female partner with normal fertility or treated infertility. Adult men with a palpable varicocele and abnormal semen analysis but who are not currently attempting to conceive should also be offered varicocele repair. Adolescents and young men with a varicocele but a normal-sized ipsilateral testicle or normal semen analysis, or both, should be offered annual follow-up monitoring.11 The following equipment is required to perform transcatheter embolization: • High-resolution digital fluoroscopy • Standard catheters and guidewires • Ultrasound for vascular access • Hockey stick–shaped catheters • Guide catheters with Simmons- and Hopkins-type (i.e., modified Cobra) curves • Microcatheters and guidewires • A selection of standard and hydrophilic wires, such as Bentson, Rosen, Terumo, Roadrunner • Embolization coils and, when appropriate, microcoils Venous blood drains from each testicle into multiple venous sinuses called the pampiniform plexus or the spermatic venous plexus. This plexus coalesces at approximately the level of the femoral head to form the internal spermatic vein (ISV), the primary draining vein. Classically, the left ISV drains into the left renal vein, and the right ISV into the inferior vena cava (IVC) anterolaterally, just caudal to the right renal vein. This classic anatomic pattern is seen on the right in 78% of patients and on the left in 79%. Variations from the classic pattern seen on the right are termination of the ISV in the renal vein in 8% and multiple veins terminating in the IVC and the renal vein in 16%. On the left, multiple veins terminating in the renal vein are seen in 20%. Rarely, one of multiple branches may terminate in the infrarenal IVC.26 Three other veins arise from within the pampiniform plexus: the external pudendal, vasal, and cremasteric veins. The external pudendal vein forms at the level of the superior pubic ramus and drains into the great saphenous vein. The vasal or ductus deferens vein forms just above the testicle, joins the inferior or superior vesicle vein, and ultimately drains into the internal iliac vein. The cremasteric (external spermatic) vein forms at the level of the superior pubic ramus and drains via the inferior epigastric vein into the external iliac vein. Based on the results of an intraoperative surgical venography study performed by Wishahi,27 venous drainage of the testes is mainly via the ISV, followed by the external pudendal, vasal, and cremasteric veins in decreasing order of significance.
Management of Male Varicocele
Incidence
Diagnosis
Indications
Equipment
Technique
Anatomy and Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine