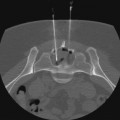
Angiomyolipoma (AML) is the most common benign mesenchymal neoplasm of the kidney. It is characterized by proliferation of varying amounts of dysmorphic thick-walled blood vessels, smooth muscle, and mature adipose tissue.1 AMLs account for 0.3% to 3% of renal masses and 1% of surgically resected tumors,2–5 although these numbers probably underestimate the prevalence of this tumor. Malignant transformation does not occur except in rare cases.6 Around 50% to 70% of AMLs are sporadic, more commonly unilateral and single, right-sided (two thirds of lesions), and occur almost exclusively in adult females (fourth to sixth decade, with a 4 : 1 female/male ratio).7–10 Some 30% to 50% of AMLs are bilateral, multiple, develop early in life (third to fourth decade), have no sex predilection, and are usually associated with tuberous sclerosis complex (TSC).10,11 TSC (Bourneville disease) is a syndrome with autosomal dominant inheritance and includes variable expressions of mental retardation, seizures, facial angiofibroma, subungual fibroma, retinal hamartomas, renal cysts, and AMLs. Approximately 20% of patients with AMLs have TSC, and up to 80% of patients with TSC have AMLs.12 In addition, AMLs associated with TSC are far more likely to be larger than the sporadic form, which increases the risk of hemorrhage.7 The classic treatment of AMLs that are symptomatic, show progressive growth on follow-up imaging studies, or are larger than 4 cm has been nephron-sparing partial nephrectomy.13 However, since the first embolization of a bleeding AML with gelfoam in 1977,14 selective renal artery embolization, which spares normal renal parenchyma, has become increasingly popular and is gradually replacing partial or total nephrectomy. In adults, a renal mass containing fat is diagnostic of AML,15 and cross-sectional imaging with computed tomography (CT) or magnetic resonance imaging (MRI) are the best diagnostic imaging modalities to detect subtle fat within a tumor.16–18 Since approximately 5% of AMLs have no detectable fat on imaging, AMLs without demonstrable fat require tissue diagnosis to exclude renal cell carcinoma.17 AMLs may occasionally extend into the inferior vena cava, but that does not imply malignant transformation.19 CT angiography (CTA) may show numerous, often aneurysmal, vessels within and around the tumor. If a solid-appearing lesion is detected in a patient with TSC, fluorodeoxyglucose positron emission tomography (FDG-PET) can be helpful because AMLs are generally not FDG-avid.20,21 Angiography is generally performed for intervention rather than diagnosis. The angiographic findings of AML are consistent with a highly vascular tumor, sacculated pseudoaneurysms, lack of normal vessel tapering, tortuous vessels, absence of arteriovenous shunting, “sunburst” appearance of capillary nephrogram, and “onion-peel appearance” of peripheral vessels in the venous phase.22–24 The most serious complication of renal AML is tumor rupture and acute hemorrhage, which can be massive (Wunderlich syndrome) and life threatening.8,25 Patients with AML and TSC are also at increased risk for tumor invasion of the adjacent normal renal parenchyma, causing chronic kidney disease and even end-stage-renal failure.26 Treatment of AML depends on the presence of symptoms, size and number of tumors, and presence or absence of TSC. AMLs smaller than 4 cm in maximum diameter that are discovered incidentally in asymptomatic patients do not require treatment.8,27 There is controversy as to when to perform follow-up imaging, but this is usually done by annual CT or ultrasound. Symptomatic presentations of AML include abdominal or flank pain, a palpable mass, hematuria, fever, anemia, and hypertension, with the most common symptoms being acute flank pain and hematuria.28,29 There is a direct correlation between AML size and symptoms. About 80% of AMLs smaller than 4 cm in maximum diameter are usually asymptomatic, whereas nearly 80% of tumors larger than 4 cm cause symptoms.25 Of the latter, 80% to 90% are symptomatic, and 50% to 60% bleed spontaneously.8,30 In addition to size, the likelihood of AML hemorrhage depends on the presence of intratumoral aneurysms larger than 5 mm.22 The relation between pregnancy and AML rupture is not clearly defined, but a review of the reported cases in the literature suggests that pregnancy could increase the risk of renal AML rupture.31 AMLs that are larger than 4 cm in asymptomatic patients may be observed using short follow-up intervals. However, in view of the significantly increased risk for a potentially catastrophic hemorrhage, either spontaneously or after minimal trauma, partial nephrectomy or renal arterial embolization is warranted in these patients.30 A variety of embolic materials have been used, including particles (<500 µm), but these do not penetrate to the capillary level. Absolute ethanol is advocated by some interventionalists to be the embolic agent of choice for selective embolization of AML because it causes complete occlusion of the peripheral renal arteries. Ethanol is mixed with ethiodized oil (Ethiodol [iodized poppyseed oil]; Savage Laboratories, Melville, N.Y.) to make it radiopaque. It is very important to inject the mixture slowly to prevent reflux and nontarget embolization into the rest of the renal arterial circulation. Selective renal artery embolization can also be performed on AMLs larger than 10 cm, since resection of these tumors would require that a greater percentage of the kidney be removed.32 The following equipment is required to perform transcatheter renal artery embolization: • Angiographic unit with digital fluoroscopy (preferably pulsed fluoroscopy to reduce radiation dose) • Standard 5F to 6F vascular sheath • Standard 4F or 5F selective angiographic catheters (Cobra-2, Simmons-1) with 0.035-inch guidewires • High-flow coaxial microcatheters (0.025- to 0.028-inch lumen) with appropriate microwires • Embolization agent: ethanol and ethiodized oil, or polyvinyl alcohol particles (<500 µm)
Management of Renal Angiomyolipoma
Clinical Relevance
Indications
Equipment
Radiology Key
Fastest Radiology Insight Engine