, Valery Kornienko1, Alexander Potapov2 and Igor Pronin3
(1)
Department of Neuroradiology, Burdenko Neurosurgery Intitute, Moscow, Russia
(2)
Department of Neurotrauma, Burdenko Neurosurgery Insitute, Moscow, Russia
(3)
Department of Neuroradiology, Burdenko Neurosurgery Institute, Moscow, Russia
Abstract
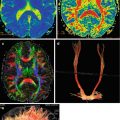
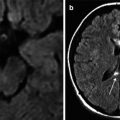
Chapter 5 focuses on peculiarities of the regional cerebral blood flow in hemispheric structures studied by CT perfusion method when using the simultaneous intracranial and cerebral perfusion pressure monitoring in patients with severe traumatic brain injuries. Patients were divided into three groups: with diffuse axonal injury, with diffuse axonal injury in combination with cortical-subcortical contusions and epidural-subdural hematomas, and with hemorrhagic or nonhemorrhagic focal contusions accompanied by epidural-subdural hematomas.
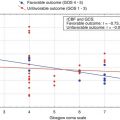
These studies showed that the three examined groups of patients with relatively similar severity of traumatic brain injury (comatose state at admission) had different variants of brain damage, different cerebral perfusion pressure, and different regional cerebral blood flow response.
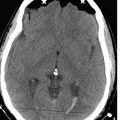
The data obtained confirmed the clinical and predictive value of brain displacement in neurosurgical pathology. Intracranial hemorrhages; development of focal, hemispheric, or diffuse edema and ischemia; and brain swelling caused by hyperemia lead to disturbance of the relationship between intracranial volume and pressure followed by a lateral and axial shift of the brain. It was determined that the degree of basal cistern compression as an indicator of cerebrospinal fluid space depletion was a significant predictive criterion correlating with the cerebral perfusion pressure. Intracranial hypertension with reduced cerebral blood flow and cerebral perfusion pressure is considered the predominant pathophysiological phenomenon of severe brain injury.
5.1 Clinical Material
Clinical material included 40 patients with severe TBI, aged 16–54 years (average 31 ± 10.4), 29 males and 11 females. Brain trauma was caused by traffic accidents in 27 cases (67.5 %), assaults or fights in 10 (25 %) cases, and falls from one’s own or great heights in 3 (7.5 %) cases. Twelve patients had DAI of I–III CT categories (Marshall et al. 1991); 15 patients had DAI combined with focal cortical-subcortical contusions, including 5 patients with subdural hematomas. CT in 13 patients (32.5 %) revealed prevailing features of focal contusion; in 6 of them it was combined with epidural or subdural hematomas. Twenty-six patients (65 %) had concomitant trauma.
The severity of brain injury according to Glasgow Coma Scale at admission ranged 4–8 (average 6 ± 1.5) (Teasdale and Jennett 1974). Thirteen of 40 (30 %) patients had a lucid interval before admission; 19 (47.5 %) of 40 patients underwent surgery for intracranial hematomas, impressed skull fractures, and basal CSF leakage; 10 (25 %) of 40 patients underwent decompressive craniectomy (uni- or bilateral) due to increased intracranial hypertension and inefficient conservative treatment.
Four healthy volunteers without history of neurological disease or significant head trauma were studied using the same CT perfusion parameters; age range was 21–36 (mean = 30) (Pronin et al. 2007).
Table 5.1 shows the main characteristics and statistical data on the analyzed group of patients, including TBI severity by GCS, coma duration, outcome by GOS, CT findings, and ICP and CPP monitoring data.
Table 5.1
Summarized data on clinical and instrumental studies
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
N | Age, gender | DAI category | Contusion type | Hematoma type | SAH | IVH | Midline shift | Basal cisterns | GCS | Coma duration | GOS | Min CPP | Max ICP | Ischemia, % | Hyperemia, % | Surgery type |
1 | 18 F | 3 | No | – | 3 | 1 | 0 | 3 | 4 | 6 | 3 | 55 | 35 | 37.5 | 0 | VSH |
2 | 23 F | 3 | No | – | 2 | 0 | 0 | 3 | 5 | 11 | 3 | 60 | 18 | 50 | 0 | |
3 | 37 M | 1 | No | – | 0 | 0 | 0 | 1 | 7 | 2 | 5 | 87 | 23 | 66 | 0 | |
4 | 24 M | 1 | No | – | 2 | 1 | 0 | 1 | 5 | 27 | 3 | 50 | 40 | 12.5 | 0 | |
5 | 22 F | 3 | No | – | 3 | 0 | 0 | 4 | 4 | 17 | 3 | 23 | 55 | 25 | 0 | Rcr, L |
6 | 17 M | 1 | No | – | 0 | 0 | 0 | 3 | 7 | 3 | 5 | 65 | 15 | 0 | 12.5 | |
7 | 23 M | 3 | No | – | 3 | 1 | 0 | 4 | 4 | 7 | 1 | 24 | 50 | 12.5 | 0 | |
8 | 29 M | 1 | No | – | 0 | 0 | 0 | 1 | 7 | 6 | 4 | 73 | 16 | 25 | 0 | |
9 | 22 F | 3 | No | – | 3 | 1 | 0 | 4 | 4 | 5 | 1 | 50 | 30 | 30 | 0 | DEC R + L |
10 | 30 M | 1 | No | – | 0 | 0 | 0 | 1 | 7 | 14 | 4 | 86 | 15 | 25 | 12.5 | |
11 | 29 F | 2 | No | – | 1 | 0 | 0 | 1 | 5 | 6 | 3 | 86 | 27 | 25 | 0 | |
12 | 17 F | 1 | No | – | 0 | 0 | 0 | 1 | 7 | 4 | 4 | 60 | 20 | 0 | 25 | |
13 | 26 M | 2 | 2 | – | 1 | 0 | 0 | 2 | 7 | 10 | 5 | 59 | 40 | 12.5 | 0 | |
14 | 20 M | 1 | 2 | – | 2 | 0 | 0 | 1 | 7 | 12 | 4 | 74 | 26 | 50 | 0 | |
15 | 23 M | 3 | 2 | – | 2 | 0 | 0 | 3 | 7 | 8 | 3 | 75 | 15 | 12.5 | 12.5 | Sfr |
16 | 34 M | 3 | 2 | SDH, R | 3 | 0 | 12 | 3 | 4 | 8 | 3 | 67 | 28 | 25 | 0 | DECSDHr |
17 | 38 M | 3 | 2 | SDH, L | 3 | 1 | 5 | 2 | 4 | 15 | 1 | 60 | 50 | 0 | 50 | Rcr SDHr |
18 | 37 M | 1 | 2 | SDH, L | 3 | 0 | 2 | 1 | 8 | 11 | 4 | 95 | 48 | 75 | 0 | |
19 | 31 M | 2 | 2 | – | 3 | 0 | 0 | 2 | 7 | 14 | 4 | 59 | 30 | 12.5 | 0 | |
20 | 51 F | 3 | 2 | – | 3 | 1 | 4 | 3 | 5 | 10 | 3 | 55 | 22 | 25 | 0 | DEC L |
21 | 16 F | 2 | 2 | SDH, R | 3 | 1 | 3 | 2 | 7 | 7 | 5 | 50 | 40 | 25 | 0 | DEC R, SDHr |
22 | 26 M | 2 | 2 | – | 3 | 0 | 6 | 2 | 6 | 7 | 4 | 50 | 20 | 33 | 0 | |
23 | 25 M | 2 | 2 | 3 | 0 | 5 | 2 | 8 | 17 | 3 | 90 | 28 | 12.5 | 0 | ||
24 | 17 F | 3 | 1 | SDH, R | 3 | 0 | 7 | 2 | 7 | 9 | 4 | 55 | 20 | 50 | 37.5 | Oser SDHr |
25 | 38 F | 3 | 2 | 3 | 0 | 0 | 3 | 4 | 9 | 1 | 50 | 35 | 25 | 0 | DEC R | |
26 | 20 M | 2 | 2 | – | 3 | 0 | 5 | 3 | 5 | 6 | 4 | 80 | 32 | 12.5 | 12.5 | |
27 < div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|