, Mark J. Jameson2, Matthew A. Hubbard3, Max Wintermark4 and Sugoto Mukherjee5
(1)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
(2)
Division of Head and Neck Surgical Oncology, Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health System, Charlottesville, VA, USA
(3)
Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health Systems, Charlottesville, VA, USA
(4)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(5)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
Abstract
A bewildering variety of lesions occurs in the maxilla and the mandible. Although a specific diagnosis of these can be difficult on imaging, it is important to be familiar with the key imaging characteristics of a few common entities and to be facile at detecting imaging signs of aggressive neoplastic, inflammatory, and infectious processes. This chapter describes a fundamental approach to commonly encountered jaw lesions; it does not address dental or temporomandibular joint pathology in detail.
11.1 Introduction
A bewildering variety of lesions occurs in the maxilla and the mandible. Although a specific diagnosis of these can be difficult on imaging, it is important to be familiar with the key imaging characteristics of a few common entities and to be facile at detecting imaging signs of aggressive neoplastic, inflammatory, and infectious processes. This chapter describes a fundamental approach to commonly encountered jaw lesions; it does not address dental or temporomandibular joint pathology in detail.
11.2 Anatomy
The term “jaws” refers to the teeth-bearing bones including both the mandible and the maxilla. Because of their arched contour, the anatomic positions anterior and posterior are somewhat inexact, and the terms mesial (toward the midline) and distal (toward the molars) are favored.
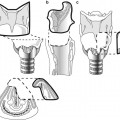
The mandible is comprised of a body and paired rami, coronoid processes, and condylar processes. The ramus meets the body at the angle. The midline of the body is the mandibular symphysis (Fig. 11.1). The buccal surface of the mandible attaches multiple muscles: the lateral pterygoid at the condylar process, the medial pterygoid at the posterior-inferior ramus near the angle, the temporalis at the coronoid process, and the masseter at the ramus. The temporalis, medial pterygoid, and masseter close the jaw. The lateral pterygoid opens the jaw and moves it from side to side (Fig. 11.2).
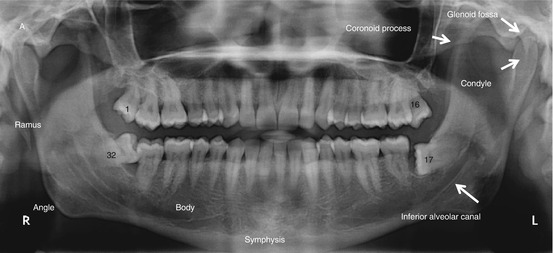
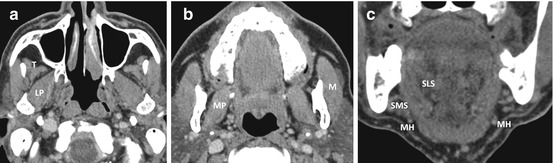
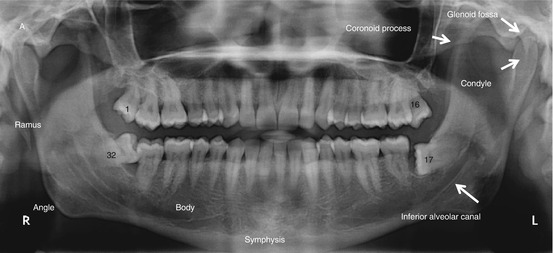
Fig. 11.1
Orthopantomogram depicting mandibular anatomy and teeth numbering
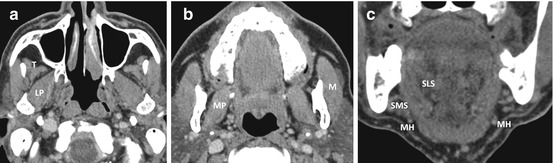
Fig. 11.2
Muscles attached to the mandible. LP lateral pterygoid, MP medial pterygoid, M masseter, T temporalis, MH mylohyoid, SMS submandibular space, SLS sublingual space
The lingual surface of the ramus contains the inferior alveolar foramen through which pass the inferior alveolar nerve and artery into the canal of the same name. The inferior alveolar nerve, a branch of the mandibular (third) division of the trigeminal nerve (V3), exits the mandible through the mental foramen on the buccal aspect of the body. The mental foramen is generally in line with the longitudinal axis of the second premolar.
The lingual surface of the body attaches to the mylohyoid muscle at the mylohyoid line. The left and right mylohyoid muscles combine to form a sling that separates the submandibular and sublingual spaces (Fig. 11.2). Posteriorly, the mylohyoid sling has a free margin where the two spaces are contiguous. In the midline, the lingual surface contains the genial tubercle that attaches to the genioglossus superiorly and the geniohyoid inferiorly. Below the genial tubercle on each side is a shallow groove for the attachment of the anterior belly of the digastric.
The alveolar process of both the mandible and maxilla supports the teeth. The mandibular alveolar process tapers distally to a triangular plateau called the retromolar trigone (Fig. 11.1). Lateral to this is a depression, the retromolar fossa, limited externally by a ridge contiguous with the coronoid process called the temporal crest. Squamous cell carcinomas arising from the mucosa in this region can present with early osseous and deep space invasion.
The temporomandibular joint (TMJ) is formed by the articulation of the mandibular condyle with the concave glenoid fossa in the temporal bone which is positioned just posterior to a convex articular eminence. The TMJ space is divided by a biconcave fibrocartilaginous disc that moves in conjunction with the mandibular condyle.
The 32 adult teeth are bound to dental sockets in the alveolar processes by the periodontal ligaments that form the lucencies around the tooth roots seen on radiographs. The teeth may be named by descriptors including the side, the jaw (mandibular or maxillary), the position (lateral/medial, first/second/third), and the tooth type (incisor, canine, premolar, molar) or by a single number from 1 to 32, starting at the right upper jaw and ending in the right lower. Children have 20 deciduous teeth which are numbered from the right upper jaw to the right lower. The teeth have occlusal, buccal, lingual, mesial, and distal surfaces.
11.3 Imaging Evaluation
Plain radiographs and pantomograms are extremely useful in the initial evaluation of the jaws. It is possible to characterize some small jaw lesions definitively using plain films alone. Lesions greater than 2 cm are better evaluated with CT or MRI. In a setting of suspected odontogenic infection, osteomyelitis, or osteonecrosis, CT is the modality of choice. CT is also useful in the detection of osseous invasion by malignancy. The role of MRI is limited to those cases where CT or plain radiography is equivocal.
11.4 Benign Lesions
11.4.1 Cystic Lesions
It is important to note that the term “cystic” as used here refers to the imaging appearance (bone lysis with resulting cystic appearance) and does not necessarily indicate a pathological characteristic. Radiographically, these lesions present as discrete, well-marginated, sometimes expansile osteolytic lesions.
The vast majority of small discrete lytic jaw lesions are periapical cysts. These are associated with chronic infection that progresses from the pulp of a tooth through its root into the alveolar bone. Initially, a periapical granuloma is formed, which transforms with time into a sterile cavity (Fig. 11.3).


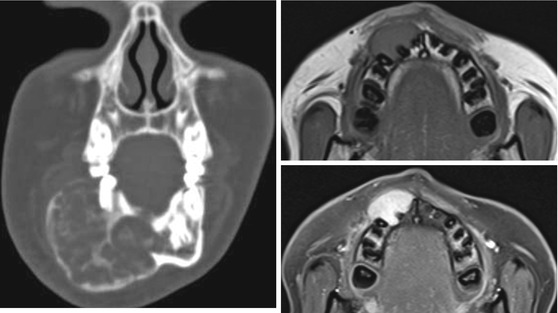
Fig. 11.3
Typical periapical granulomas on CT
Dentigerous cysts arise from odontogenic epithelium around the crown of an unerupted tooth, usually a molar. They typically appear as a well-defined expansile lytic lesion which contains an unerupted tooth. Very rarely, an ameloblastoma may arise from the lining of a dentigerous cyst (Fig. 11.4).
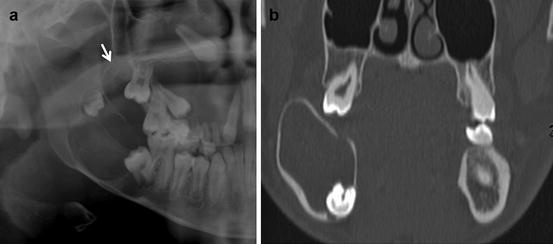
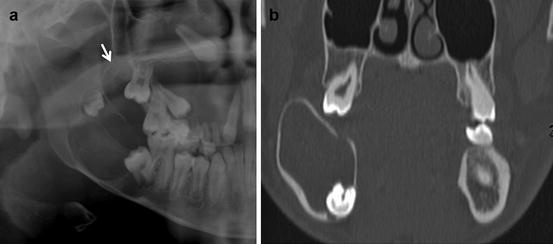
Fig. 11.4
Dentigerous cyst. Radiograph (a) and CT (b) images of dentigerous cysts. A typical dentigerous cyst is an expansile unilocular lesion containing an unerupted tooth. Occasionally more than one cyst may be present (arrow, a)
Odontogenic keratocysts are lined by stratified squamous epithelium and contain keratin. They tend to grow along the long axis of the mandible, insinuating themselves between the dental roots and thus do not contain a tooth. When multiple odontogenic keratocysts are seen, a diagnosis of basal cell nevus (Gorlin’s) syndrome must be entertained. This syndrome is characterized by the appearance of nevoid basal cell carcinomas at a young age (Fig. 11.5).
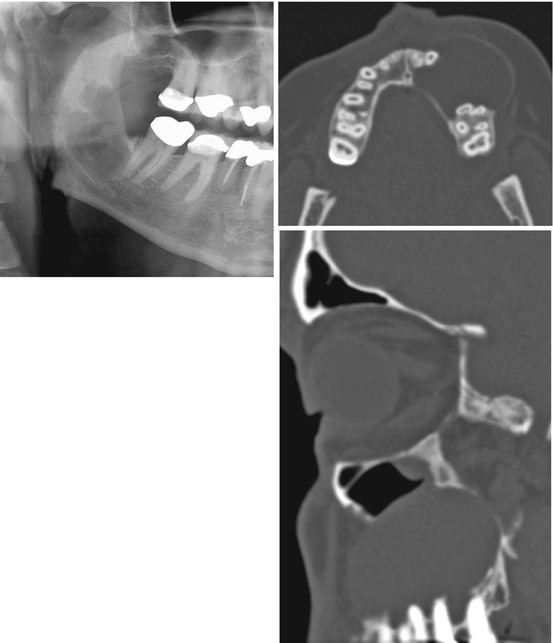
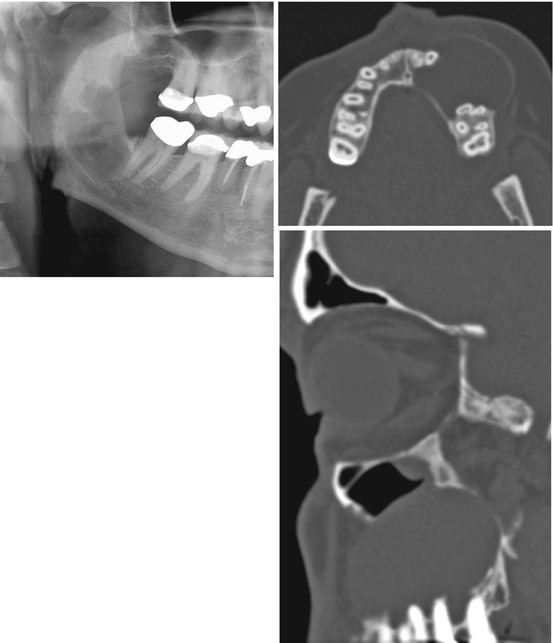
Fig. 11.5
Odontogenic keratocyst. A typical OKC is expansile, is unilocular, and does not contain an unerupted tooth. Multiple odontogenic keratocysts suggest Gorlin’s syndrome, a condition characterized by multiple nevoid basal cell carcinomas in childhood, cardiac and ovarian fibromas, and macrocephaly along with higher incidence of medulloblastomas
Unicameral bone cysts, similar to those seen in the long bones, may also be encountered in the maxilla and mandible of young people. They are well-defined expansile lesions with no other distinguishing characteristics. They are postulated to arise as a consequence of liquefaction of an intraosseous hematoma.
A Stafne cyst or cavity is a developmental variation found at the angle of the mandible. They may be bilateral and contain a rest of salivary glandular tissue.
Fissural cysts occur along mandibular and maxillary embryonic fusion lines. The most common fissural cyst is the nasopalatine duct (incisive canal) cyst seen between the premaxilla and the hard palate in the midline. These are usually incidentally detected but occasionally erode into the oral cavity forming a submucosal mass on the anterior hard palate (Fig. 11.6).
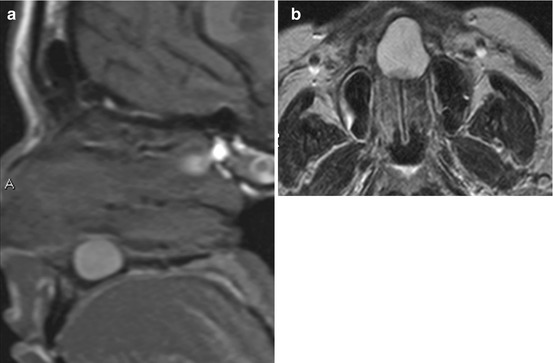
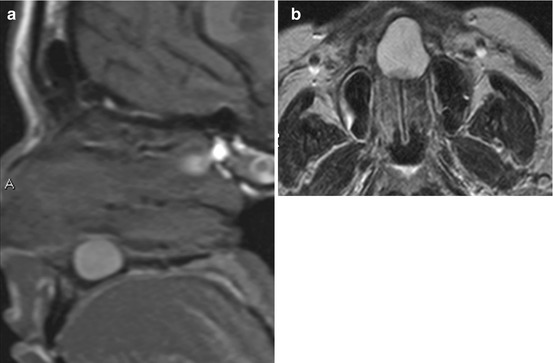
Fig. 11.6
Incisive canal or nasopalatine duct cysts. (a, b) Are examples of incisive canal cysts. They occur in the midline at the junction of the hard palate and premaxilla and are usually found incidentally. Occasionally they may be large enough to cause cosmetic deformity. Rarely secondary infection may occur. The high T1 signal of the cyst contents in these images reflects elevated protein concentration
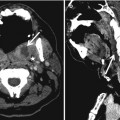
Ameloblastomas (Fig. 11.7) are benign tumors arising from odontogenic epithelium that appear as unilocular or multilocular expansile lytic masses. When septations are present, they can produce a characteristic “soap bubble” appearance. Although ameloblastomas tend to breach the cortex and extend into adjacent soft tissues, only a tiny fraction is malignant. Ameloblastomas can exhibit enhancing papillary projections that distinguish them from other radiographic cysts (lytic lesions) that are not tumors; these projections can sometimes be seen on contrast-enhanced CT but are more reliably detected with MRI.
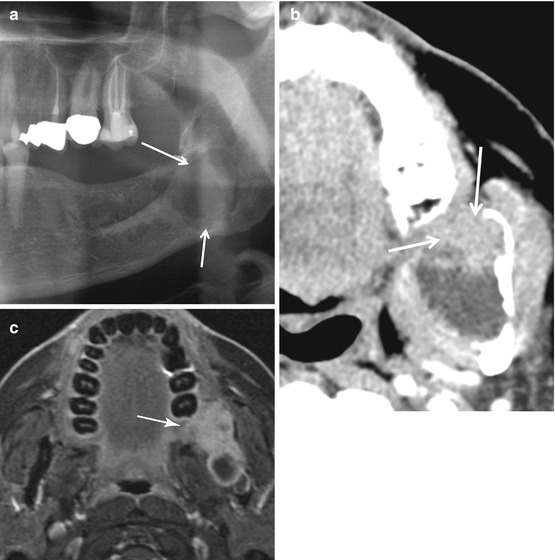
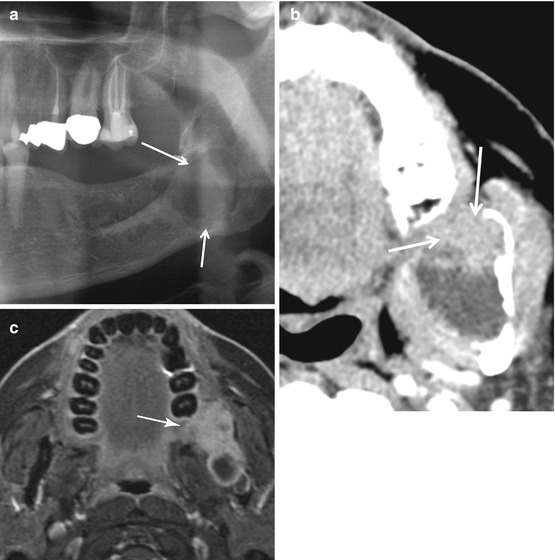
Fig. 11.7
Ameloblastoma. The radiograph (a) demonstrates a lytic multiloculated lesion. The contrast-enhanced CT (b) depicts the solid papillary projections (arrow) that characterize this tumor. Ameloblastomas can sometimes be unilocular. When a benign lesion cannot be definitively excluded on radiography, it is prudent to obtain a cross-sectional study to characterize the internal architecture of these lesions and establish the diagnosis as in the fat-suppressed contrast-enhanced image, (c) (Courtesy of Dr William P. Dillon, University of California, San Francisco), where solid areas of enhancement are evident
When one encounters a lytic expansile jaw lesion in a middle-aged or older patient that does not conform to the appearance of one of the more typical benign cysts discussed above, a contrast-enhanced CT or MRI must be recommended to characterize it further. These can demonstrate the enhancing papillary projections that, when present, are highly suggestive of ameloblastoma. Ameloblastomas are treated with wide excision as they have a tendency to recur.
Odontogenic myxomas are benign but locally aggressive expansile tumors seen in young adults; they may be indistinguishable from ameloblastomas (Fig. 11.8).


Fig. 11.8
Odontogenic myxoma. These tumors resemble ameloblastomas on imaging and must be suspected when an expansile multiloculated lesion is encountered in a young patient
Aneurysmal bone cysts of the jaws present as expansile multilocular masses containing characteristic blood-fluid levels on MRI. They resemble giant cell lesions, a category that includes brown tumors of hyperparathyroidism, giant cell reparative granulomas, and true giant cell tumors. Brown tumors are unilocular lesions that may be associated with loss of the lamina dura, a finding typical of the bone resorption of hyperparathyroidism. Giant cell reparative granulomas and giant cell tumors are multilocular expansile lesions that may be indistinguishable from ameloblastomas and aneurysmal bone cysts (Fig. 11.9).