(3)
Department of Emergency and Critical Care Medicine, Hiroshima University, 1-2-3 Kasumi, Minami-ku, Hiroshima 734-8551, Japan
3.1.1 Introduction
The biggest challenge in a radiation disaster is the loss of important elements of the medical response system due to the impacts of radiation. Thousands of workers, fire fighters, and military personnel are mobilized to engage in the restoration activities, and evacuation of residents is urgently performed, while the local emergency medical response system may lose its ability to function effectively. The specific features of a radiation disaster are characterized as follows:
1.
The local emergency medical system is partially or completely lost because of the impact of radiation.
2.
Release of massive doses of radioactive materials makes it difficult to set up any safety zone for the command center near the disaster site.
3.
Radiation dose monitoring systems may not work, and information on radiation may not be available in a timely fashion.
4.
It usually takes an extended time period to ensure that the damaged facility is under control. In the early phase, severe acute radiation syndrome may be encountered, and isolated trauma cases or severe acute radiation illnesses, with or without contamination, are frequently observed during this period.
5.
Displaced people may have to stay in shelters or other places for months or even years. This can lead to severe public healthcare issues.
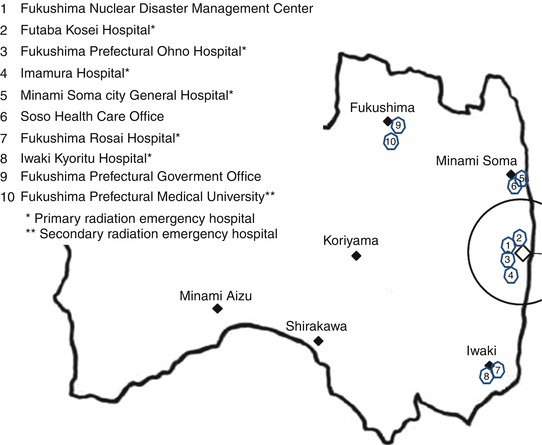
3.1.2 Reestablishment of a Medical Response System in the Region
Soon after the accident, the local medical system, including the emergency medical services system, may not function properly due to the risks of radiation and the designation of an evacuation zone. At this stage, a mass casualty event (MCE) in the accident site may occur, and hospital patients and/or elderly persons in care facilities may commence with evacuation. In Fukushima, not only all hospitals and care facilities in the region but also the primary radiation emergency medical hospitals were forced to close because of the evacuation order (see Sect. 3.1.8). Hundreds of hospital patients and elderly persons at care facilities were hurriedly transported out from the evacuation zone. Exactly at the same time, an explosion occurred at the nuclear power plant. This was the moment when the medical needs suddenly expanded. In that sense, an emergency medical response in a radiation disaster is quite similar to that in other types of major disasters such as a huge earthquake.
3.1.2.1 Planning for Medical Responses in an MCE and Evacuation of Inpatients
The role of each component of the emergency response system, i.e., the nuclear facility, fire departments, police, hospitals, military, and the local and national government must be determined during advance planning. The focus should be on field care and patient triage; decontamination, transportation, and distribution; and hospital-based acute care and treatment for radiation injuries. Also, protocols for secondary transfer to other facilities out of the disaster region and methods of transportation should be drawn up. Ideally, medical advisers who are familiar with the local emergency medical system, and specialize not only in radiation emergency medicine but also disaster medicine, should be designated in planning. In the event of a radiation disaster, these medical advisers will join the command center to coordinate the activities (Morimura et al. 2012).
In evacuation planning, essentials that need consideration include distribution of hospitals and care facilities, number of patients in the area, available vehicles, evacuation routes, estimated time for evacuation, and available hospitals and facilities for evacuees (Yamamoto 1993). Medical teams should be mobilized to attend to the patients for evacuation. The role of the medical team will start before evacuation, as proper care may not have been provided for patients, due to the establishment of the restricted zone. Therefore, the medical team should triage patients, provide medical care as needed before evacuation, and arrange appropriate methods of transportation (Fig. 3.1). If possible, medical care should be continued during and after evacuation. The medical team, consisting of doctors, nurses, technologists for radiological examinations, and logistics personnel, should be trained for a radiation emergency and be appropriately equipped with necessary items such as personal protective equipment (PPE) and radiation meters.


Fig. 3.1
Evacuation of inpatients supported by Disaster Medical Assistance Teams (DMATs). Ambulances and Japan Self-Defense Force (JSDF) vehicles were mobilized to the collection area (upper photo). Patients were triaged and provided care before transportation (lower photo)
Reestablishment of a medical response system in a radiation disaster should be planned in advance. Based on the simulated spread patterns of contaminated areas and available medical resources, i.e., hospitals, fire departments, and access, several alternative plans should be determined.
In the event of a disaster, establish a medical response system as soon as possible to prepare for MCE and evacuation. In accord with the plan, mobilize all available regional and national resources to the area to strengthen the local medical response system. In order to achieve these goals, local authorities as well as the national government must understand the consequences of a radiation disaster and make plans to reestablish an emergency medical response system suited for the specific medical needs in the region.
3.1.2.2 General Concepts in Prehospital Emergency Response
Although a radiation disaster is quite rare, its effects will be devastating not only for the individuals but also for the whole society and the nation. However, most of the medical resources required in a radiation disaster can be provided with structural and functional resources for disaster medicine with specific requirements for protection from radiation. Proper understanding of radiation is fundamental to saving the lives of victims as well as minimizing the effects of radiation on the rescuers and victims.
3.1.2.2.1 Basic Understanding Required for Medical Response
Radiation effects on individuals can be from external and/or internal dose. Emergency personnel should always keep in mind the basic principle of protection from external radiation: distance, time, and shield. Also, they should avoid internal contamination (refer to Chap. 2). By observing the basic principle of protection, one can control the effects of radiation.
Initial information is usually very scarce in radiation disasters as with other types of disasters. In any situation where involvement of radioactive materials is suspected, absorption of radioactive materials should be minimized as much as possible by wearing personal protective equipment (PPE) with an effective mask for radioactive materials (Fig. 3.2). The full face mask should be checked for appropriate filters and/or charcoal before use and no leak must be observed when the mask is put on the face. By using radiation survey meters and a personal dosimeter, one can determine radiation doses and estimate how much individuals are exposed to externally.
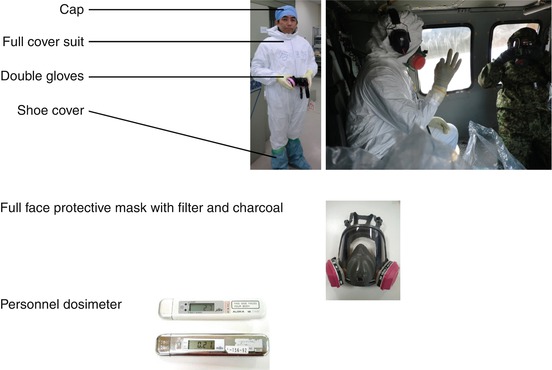
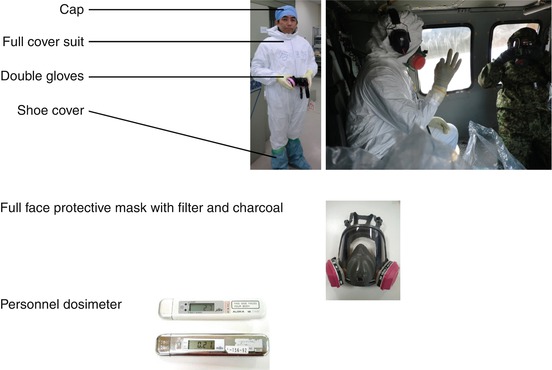
Fig. 3.2
Personal protective equipment (PPE) required for field missions
Until involved radioactive materials are determined, one can anticipate the most likely sources of radiation based on information of the site, types of operation, and nature of the accident (Table 3.1) (International Atomic Energy Agency [IAEA] 2002a). For example, in a nuclear accident, radioactive iodine (131I, 133I) and cesium (137Cs, 134Cs), besides radioactive gases, i.e., 85Kr and 133Xe, are likely to be released into the atmosphere when a nuclear fuel container is breached during the operation of a nuclear reactor. In addition, heavy metals such as 90Sr and 239Pu might contaminate soil or water adjacent to a damaged reactor.
Table 3.1
Types of radiation accidents, effects, and major source of dose
Accident | Critical organ | Major source of dose |
|---|---|---|
Reactors (power, research, ship) | Whole body (bone marrow) | Gamma |
Skin | Beta | |
Thyroid | Radioiodine | |
Spent reactor fuel storage or reprocessing | Whole body (bone marrow) | Gamma |
Industrial and medical gamma sources (sealed) | Whole body (bone marrow) | Gamma |
Skin | Gamma | |
Industrial and medical gamma sources (damaged, unsealed) | Whole body (bone marrow) | Gamma |
Skin | Beta | |
Pu – weapons damage or manufacture | Lung | Alpha |
The effects of radiation after a nuclear reactor accident are mainly due to released radioactive vapors, dust, and nuclear fallout (the radioactive particles that fall to the ground, trees, grass, or buildings). High levels of ambient radiation are mainly due to gamma rays emitted from released radioactive materials. In emergency situations, the International Commission on Radiological Protection (ICRP) (2007) sets no dose restrictions for saving lives if and only if the benefit to others clearly outweighs the rescuer’s own risk. To prevent the development of catastrophic situations, radiation exposure for emergency personnel must not exceed the range from 500 mSv up to 1,000 mSv in order to avoid acute radiation injuries.
Among radioactive materials released in a nuclear reactor accident, 131I and 137Cs are the major health hazards. In addition to wearing PPE, those who are younger than 40 years old will be advised to take potassium iodide (KI) to prevent deposition of radioactive iodine in the thyroid gland. When the use of KI is indicated, it should be prepared prior to the field mission. The indicated level of weighted, committed dose equivalent to the thyroid is 50–100 mSv (IAEA 2011). However, in a field mission, estimation of thyroid doses is quite difficult and impracticable. Therefore, prophylactic administration of KI is recommended for those who are about to engage in activities in an environment where large doses of radioactive iodine is likely to be released.
Persian blue (PB) is indicated in case of radioactive cesium absorption. PB is an inert medication and expected to block the reabsorption process in the small intestine.
Experiences from Fukushima Accident: At 6 am on 15 March 2011, the No. 4 reactor building exploded and the No. 2 reactor building was severely damaged. Following these events, the radiation level reached its peak at 9 am on the same day, which was 11,930 μSv/h at the main gate, 900 m west from the damaged reactor building in Fukushima Daiichi nuclear power plant (NPP) (The National Diet of Japan 2012). On 16 March, we flew from Fukushima Medical University to pick up a worker who sustained chest injury and contamination at Fukushima Daini NPP. To reduce the effects of radiation, we wore PPE, monitored dose rate, and minimized the time of stay on the site. Figure 3.3 shows the time we left Fukushima Medical University at 10:23 (upper left), arrived at the site (10:48), picked up the worker (10:52), moved into the helicopter (10:53), and left the site. By limiting the time, the total exposure dose was controlled to 12 μSv, one quarter of the dose of a single chest X-ray.


Fig. 3.3
Reducing time in the field to minimize radiation exposure
3.1.2.2.2 Goals of Prehospital Emergency Medical Response
In a radiation disaster, the main goals of prehospital emergency medical response are:
1.
To manage the on-site response taking specific features in a radiation disaster into consideration
2.
To triage victims in order to maximize the survival of the most who are facing with life-threatening conditions
3.
To treat injuries resulting from an emergency situation and radiation exposure
Management of On-Site Response in Radiation Disaster
When a radiation disaster occurs, the restricted area is established soon and only authorized personnel are allowed to enter. Therefore, the facility personnel who have been adequately trained in techniques of radiological survey, rescue, and basic life support are to provide emergency first aid for injured persons until emergency responders from the fire department arrive.
Due to the effects of radiation, the safety zone where victims are collected, triaged, and treated in case of MCE may not be available nearby (National Center for Injury Prevention and Control 2010). In addition, wearing PPE makes it quite difficult for rescue personnel to communicate, perform triage, and provide first aid in the field. In the first explosion that took place on 12 March at the No. 1 reactor building of Fukushima Daiichi NPP, no triage was performed in the field. The only triage that was performed in the Fukushima accident was at the second explosion on 14 March and the triage was done at a site 4 km away from the plant.
It is recommended that in the event of a radiation disaster, an in-house triage and treatment area should be established on-site where dose rates are reasonably low and there is easy access from the field (Fig. 3.4). The area should have at least an adequate ventilation system, a decontamination room with warm shower, a treatment room, and an area with beds for short stay.
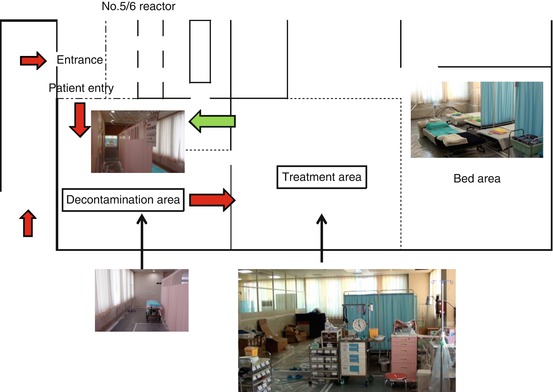
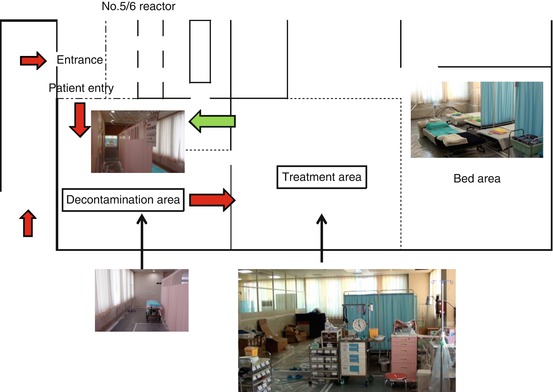
Fig. 3.4
Example of an in-house decontamination and treatment area (the emergency room of Fukushima Daiichi NPP)
Emergency medical personnel have an important role in on-site response. This is because no medical facilities are available due to the establishment of the restricted area and poor access from outside. The medical team ideally consists of emergency physicians, radiologists, nurses, and radiological technologists. However, the medical team usually comes very late after other responders, and the timing of arrival on the scene depends on radiation levels, access to the restricted area, and available medical resources of the region. The actions of the medical team should be fully incorporated into the joint emergency response in accord with ordinary approaches for MCE (National Center for Injury Prevention and Control 2010).
The medical team approaching to the accident scene should:
Monitor radiation levels using radiation survey meters and check external dose with personal dosimeter
Look for evidence of hazardous materials other than radioactive materials
Gather information on the exact location, number of casualties, access to the scene, and other emergency services on-site
Well-established command/control and good communication/collaboration/cooperation among related personnel are prerequisites for well-coordinated activities. However, the austere environment, such as exists in a radiation disaster, usually does not allow for this in the conventional manner.
With these limitations, the purpose of medical activities on the scene is to maximize the survival of the majority by triage and by preventing traumatic injuries or illness that would lead to a life-threatening condition, to assess possible contamination, and to perform procedures to control the spread of contamination.
Triage and On-Site Decontamination
Because radiation exposure does not lead to any immediate life-threatening conditions, whereas mechanical injuries or medical problems do, the general emergency medical approach can be applied in the event of a radiation disaster, that is, “Treat life-threatening conditions first!” Therefore, the treatment priority used in prehospital trauma care or cardiovascular life support, and medical triage such as simple triage and rapid treatment (START) triage comes first in MCE (Fig. 3.5) (Benson et al. 1996).
Fig. 3.5
Prehospital triage in a radiation disaster
After the patient is stabilized, radiological triage can be started. Radiation levels above background indicate the presence of contamination. In Fukushima, however, difficulties were often encountered in performing accurate radiological evaluation due to high background dose levels. The clinical symptoms such as nausea, vomiting, and diarrhea may constitute the prodromal signs of acute radiation syndrome (Table 3.2) (IAEA 2002b), which requires special attention because early essential actions are required at hospitals.
Unlikely | Probable | Severe | |
|---|---|---|---|
Nausea | – | ++ | +++ |
Vomiting | – | + | +++ |
Diarrhea | – | −/+ | −/+ to +++ |
Hyperthermia | – | – | −/+ to +++ |
Hypotension | – | – | + to ++ |
Erythema | – | – | −/+ to ++ |
CNS dysfunction | – | – | −/+ to ++ |
Once again, there should not be any delay in providing life-saving treatments if it is difficult to perform radiological assessment. If victims are trapped in a vehicle or collapsed building, life-saving maneuvers should be provided during extrication.
Remember that radiation exposure or contamination does not cause immediate signs or symptoms; therefore, if accident victims are unconscious, disoriented, burned, or otherwise in distress, look for causes other than radiation.
Criteria for on-site decontamination of the patient are shown in Fig. 3.6 (IAEA 2006). These criteria indicate the level of skin contamination which could represent a hazard from direct irradiation of the skin, from intake by inadvertent ingestion, or that could indicate that the person has already inhaled or ingested significant amounts of radioactive material. Only one ambient dose rate criterion of 1 μSv/h is provided for use by the first responder. The ambient dose rate criteria were established at levels for strong gamma emitters that can be easily detected under emergency conditions but still correspond to contamination levels more than 100 times below those at which severe deterministic health effects would be expected.
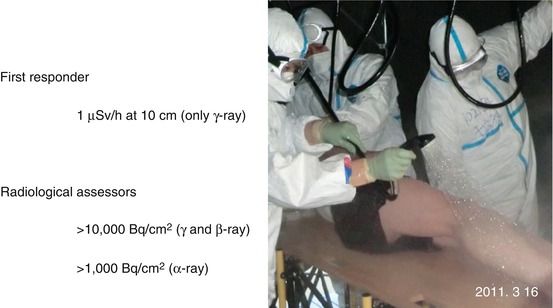
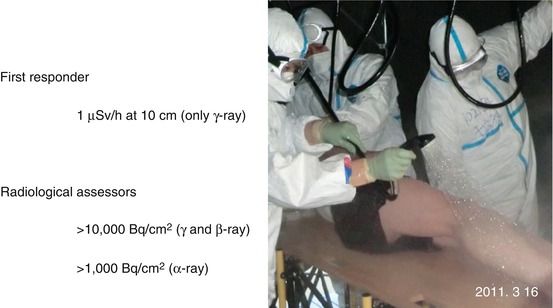
Fig. 3.6
Criteria for on-site decontamination
For external contamination, removing outer clothes may get rid of 90 % of radioactive materials attached to the clothes. Wet decontamination using warm water is recommended when feasible. If field decontamination cannot be performed, wrap the contaminated body parts or cover the patient with a sheet or blanket before transportation.
In Fukushima, sufficient water for decontamination was not available due to a massive number of evacuees and disruption of water supply caused by the earthquake. In these circumstances, simply wiping the contaminated skin with wet towels or paper may be recommended.
In cases where absorption of radioactive materials has occurred or is unavoidable, early administration of antidotes or chelates is recommended if the benefits of the medication outweigh the adverse effects of the medication itself (refer to Chap. 2).
Treatment in Prehospital Emergency Settings
Wearing personal protective equipment (PPE) makes it difficult for emergency medical personnel to perform simple activities such as taking vital signs or physical examination. In addition, the victims may be wearing PPE themselves, which interferes with clinical examination such as checking verbal responses, observing respiration or pulse, and performing life-saving maneuvers (Fig. 3.7). Depending on the safety of the scene, i.e., dose rate and any other hazards, it should be determined if provision of initial care on the scene is appropriate.


Fig. 3.7
Evaluation of the victim wearing personal protective equipment (PPE) in an in-house triage area
Example of On-the-Scene Evaluation and Treatment
If the victim is unresponsive, remove the face mask and evaluate level of consciousness (LOC) first. In treating patients with life-threatening conditions, the primary ABCDE approach is usually used (Nolan et al. 2010). The A stands for airway, B for breathing, C for circulation, D for dysfunction of central nervous system, and E for exposure. Any of the airway problems such as disturbed airway due to decreased LOC, airway trauma, or foreign body obstruction should be treated first. In chest trauma, prompt recognition of tension pneumothorax, respiratory failure due to flail chest, and/or pulmonary contusion is essential.
However, examination of the chest is impractical in the field when the victim wears PPE. In this situation, one should focus on breathing only. Only if no respiration or agonal breathing is observed, start cardiopulmonary resuscitation (CPR) if it is possible. Likewise, checking the pulse or capillary refilling is not practical. Observe external bleeding only, and stop active bleeding manually if found.
If the victim is transported to the facility room, ordinary advanced trauma life support or cardiovascular life support may be provided if medical resources are available. Remember, any problems in ABCDE should be managed before radiological survey is started.
In spite of the austere circumstances in a radiation disaster, levels of prehospital emergency care provided in the field should be appropriate to avoid any adverse conditions during transportation.
3.1.3 Establishment of a Command Center
The command center will be positioned in a safe area and as close to the accident site as possible. This location will serve as the center for communication and coordination of all activities to control the emergency and to manage public protection measures. However, in a radiation disaster, the effects of radiation may make it difficult to set up the command center near the site.
In Fukushima, the Fukushima Nuclear Disaster Management Center, where the off-site center was set up to function as a disaster headquarters in nuclear disaster management, was located 4 km from the Fukushima Daiichi NPP. Because of the power and communication failure due to the earthquake, and soaring levels of radiation dose, the center was soon closed (The National Diet of Japan 2012). Although the off-site center were relocated to the Fukushima Prefectural Government office in Fukushima City, practical on-site managements for restoration operations was performed by the command center established at the Japan Football Association’s (JFA) National Training Center (known as J-Village), 20 km south from the Fukushima Daiichi NPP (Fig. 3.8). The J-Village served as the headquarters of the Japan Self-Defense Force (JSDF), the fire departments, and Tokyo Electric Power Company (TEPCO) from soon after the accident occurred. The radiation dose rate was within acceptable ranges there, and it had accommodation facilities and a huge football ground suited for a helicopter base. Also, this center was used as a screening site and functioned as a gateway to Fukushima Daiichi NPP of the workers. The J-Village had all the necessary requirements of a command center in a nuclear accident.


Fig. 3.8
J-Village JFA National Training Center
In preparation, appropriate alternative sites for the command center should be determined in advance, taking factors such as distance, access, and simulated plume dispersion patterns into consideration.
3.1.4 Information on Radiation
Radioactive plume does not spread in a concentric fashion. It spreads while changing its direction quickly due to wind direction, geographic features, and weather conditions. Therefore, information on dose rate and/or prediction of spread pattern of radiation is critical to reduce health risk for all individuals. In Japan, a System for Prediction of Environmental Emergency Dose Information (SPEEDI) had been developed and was expected to play a key role in a severe nuclear accident. However, this sophisticated radiological information system failed due to the strong earthquake in Fukushima (The National Diet of Japan 2012). Instead, mobile monitoring posts had to be introduced to monitor dose rates. However only seven public data spots were available in Fukushima Prefecture, and the results were not provided in a timely fashion (Fukushima Prefectural Government 2011a).
Emergency personnel should monitor radiation dose frequently and protect themselves. For public safety, monitoring of ambient dose rate is required at key spots such as shelters, residential areas, schools, hospitals, and government offices. Portable monitoring posts should be mobilized to these areas as soon as possible after the accident, and the information should be shared openly among all citizens via any method available such as TV, radio, mobile phone, and Internet.
3.1.5 Development of a Sustainable Local Emergency Medical System
Within a short time after an accident occurs, many individuals will get involved in the restoration operations in the accident facility. In Fukushima, the reestablishment of temporary cooling facilities for the three damaged reactors and the spent fuel pool of the No. 4 reactor building was the first priority, followed by development of stable cooling systems to achieve a stable cold shutdown of the reactors, removal of radioactive debris and rubble, establishment of breakwaters, and installation of a covering container over the No. 1 reactor building. These operations continued until the end of 2011. From 11 March 2011 through 31 March 2012, a total of 19,594 workers were involved in the restoration operations at the Fukushima Daiichi NPP (TEPCO 2012).
3.1.5.1 Emergency Medical Needs of the Workers
In the first month after the accident occurred (March 2011), a total of 67 workers sought emergency medical care including those injured in two hydrogen explosions. Of note is that the majority of them complained of medical problems such as general fatigue and sickness which were unconnected to the levels of radiation dose. Until 30 June 2012, a total of 264 workers had been treated at the site (Fig. 3.9). Three deaths occurred in April, August 2011, and January 2012. Two cases developed cardiac arrest due to acute myocardial infarction. Another case with uncontrolled diabetes died of severe sepsis.
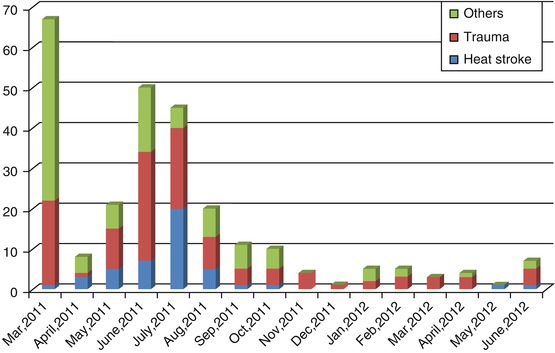
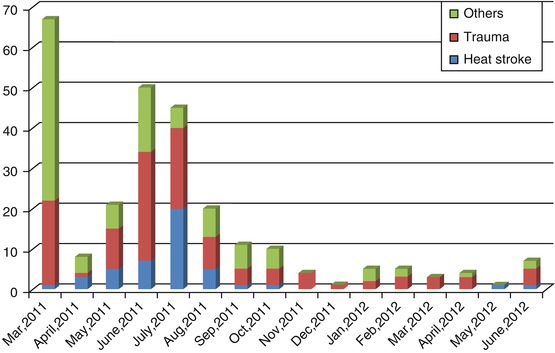
Fig. 3.9
Injuries and illnesses treated at Fukushima Daiichi NPP
Among emergency care required, trauma accounted for 49.6 % (131 cases). Most of them were observed in the first 5 months after the accident occurred (from 12 March through July 2011). Regarding severity of trauma, only one patient exceeded Injury Severity Score (ISS) of 15. Fortunately, no trauma death was reported. Only six cases were contaminated, all of which occurred in March 2011.
Heat stroke was another concern as the summer season approached. This was because the workers needed to wear PPE. There was an increase in the incidence of heat stroke in May, June, and July. The total number of heat stroke victims was 44, and most of them were treated in Fukushima Daiichi NPP. Only two cases required hospital admission. Repeated advice was provided by TEPCO to all personnel in the Fukushima Daiichi NPP such as wearing cooling jackets under protective suits, taking rest and sufficient fluids regularly, and avoiding any activities from 2 to 4 pm.
3.1.5.2 Irradiation Dose of the Workers
Ninety-six percent of the workers at Fukushima Daiichi NPP were exposed to less than 50 mSv. All of those whose radiation doses were greater than 100 mSv were exposed soon after the accident. A total radiation dose of greater than 200 mSv was observed in nine workers. Of these, two workers were exposed to greater than 600 mSv with 678 mSv being the highest of all (Figs. 3.10 and 3.11). This worker was engaged in data sampling at No. 3 and 4 reactor building and refueling missions near No. 1 reactor building from 12 March through 15 March. He wore a full face mask with dust filters but without charcoal filters that absorb radioactive iodine. He did not take potassium iodide (The National Diet of Japan 2012).
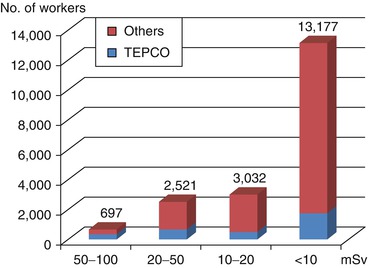
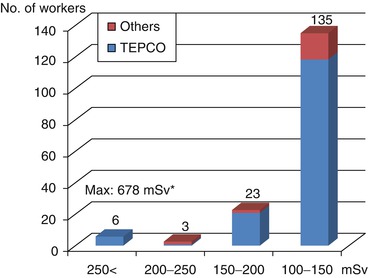
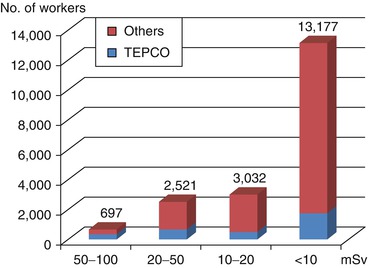
Fig. 3.10
Total radiation dose (<100 mSv) of workers who were involved in recovery operations
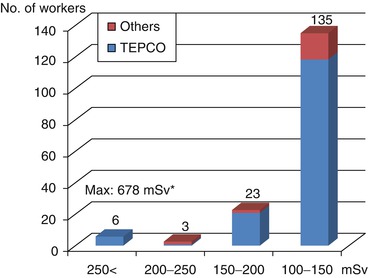
Fig. 3.11
Total radiation dose (>100 mSv) of workers who were involved in recovery operations (11 Mar 2011 to 31 Dec 2011) *Max: 678.08 mSv (Ext. 88.08 mSv, Int. 590 mSv)
The workers who had greater than 100 mSv of irradiation dose were regular employees hired by TEPCO. On the other hand, most of those with less than 20 mSv radiation dose were hired by other companies.
Fortunately, no acute radiation syndrome was observed among the affected people in the Fukushima accident.
In a nuclear reactor accident, it usually takes many years to complete decommissioning of the plant. In Fukushima, it took 2 years after the accident occurred before fuel removal from the spent fuel pool commenced. It is likely to take 10 years before the start of fuel debris removal and 30–40 years to complete the decommissioning process (TEPCO 2011). Due to the impact of radiation, medical resources have already diminished. In particular, the number of doctors and nurses has decreased since the beginning of the accident in Fukushima.
In these difficult circumstances, it will become quite challenging to develop a sustainable emergency medical system in the affected region. Strong support from the national government and authorities will be required to develop a system which meets the medical needs in the disaster-stricken area (see Sect. 3.1.8).
3.1.6 Major Public Health Consequences Following Evacuation
The establishment of a restricted zone in a radiation disaster forces large numbers of residents out of the area, where they will stay at temporary shelters or other places for long periods of time. Life conditions in shelters may lead to various types of health issues such as outbreaks of infections, mental stress, and cardiovascular diseases (Math et al. 2008; Ueda et al. 2012; Sun et al. 2013). Sudden changes in lifestyle in unfamiliar places may result in behavioral problems due to poor adaptation to new circumstances. Medical attention will be required from various healthcare disciplines.
In Fukushima Prefecture alone, the number of displaced residents was 86,308 in March 2011, and it reached the peak at 99,205 in June 2011 (Fukushima Prefectural Government 2011b). In addition, the number of residents who voluntarily moved out of Fukushima Prefecture increased from 38,896 in March 2011 to 62,831 in 12 months.
After the Great East Japan Earthquake, more than 460,000 people were displaced to about 2,400 shelters throughout Japan. According to the report on disaster-related death in the Great East Japan Earthquake issued by the Reconstruction Agency of Japan (2012), 2,688 people died at shelters or temporary houses by 31 March 2013. They are called disaster-related death (DRD). DRD is defined as a death caused by deterioration of underlying medical problems due to poor medical access or illnesses arising from poor living environments such as temporary shelters, in a disaster. Ninety percent of DRDs were over 66 years old, and more than one third died within 1 month after the quake. The number of deaths among three Tohoku prefectures was highest in Fukushima (1,383 deaths). The government report indicated that the impacts of the nuclear accident might be the major reason for higher mortality of displaced elderly in Fukushima (Reconstruction Agency of Japan 2012). Another study reported that the impact of the disaster on the excess mortality of institutionalized elderly in Fukushima was most significant in the immediate aftermath because of undesirable living conditions and poor access to medical care (Yasumura et al. 2013). In addition, relocation of these elderly was unavoidable because of the shortage of medical resources in the region, which had a lasting impact on mortality due to continuing changes in nutritional, hygiene, medical, and general care conditions.
Many healthcare professionals headed for the disaster-stricken areas. In less than 2 months after the quake, approximately 24,000 medical personnel were involved in medical activities in Tohoku regions (Table 3.3) (Health and Labor Ministry 2011). However, these medical resources may not have been utilized effectively in Fukushima because concerns over radiation existed; information on radiation and the situation of the vulnerable people was not properly shared nor was sufficient communication among related personnel established during the disaster response (Tanigawa et al. 2011; Tanigawa and Ohjino 2013).
Table 3.3
Medical teams and professions involved in medical activities in the Great East Japan Earthquake from 11 March through 25 May 2011
Teams and healthcare profession | No. of personnel (no. of teams) |
|---|---|
DMAT | Approximately 1,500 (approximately 340 teams) |
Medical team from national hospitals | 471 (92 teams) |
Medical team from medical associations | 10,354 (2,178 teams) |
Pharmacist | 1,619 |
Nurse | 1,217 |
Dentist | 220 |
Physical therapist | 60 |
Public health specialist | 6,238 (186 teams) |
Mental healthcare team | 2,093 (52 teams) |
Although the Fukushima accident was combined with a huge earthquake and tsunami, our experiences clearly indicate that the magnitude of the impact of evacuation and displacement on individuals and the society was extremely significant. Proper understanding of radiation by medical personnel as well as citizens cannot be overemphasized. Public healthcare officials and related organization should be well prepared for such an event so that all available medical resources will respond efficiently and effectively to the needs of the region in a radiation disaster.
3.1.7 Summary
The basic goals of prehospital emergency medical response in radiation disaster are the same as other types of disasters. The concept of triage in MCE and treatment priority in the field can be applied likewise. The only difference is the need for protection from the effects of radiation. However, the impacts of radiation on the society including the local emergency medical system are significant. Also, precious medical resources in disasters can be maximally utilized in a radiation disaster. A sustainable emergency medical and public healthcare system which adapt to this specific situation should be developed to cope when any emergency medical needs arise.
3.1.8 Experiences from the Initial Medical Response in Fukushima Accident
In Fukushima, the radiation emergency medical system had been developed within the frame of the national radiation emergency medical system. Six hospitals were designated as the primary radiation emergency medical facility which assumed roles in providing initial treatment and decontamination for victims and one as the secondary radiation emergency hospital (Fig. 3.12).