Omental involvement
97 %
Ascites
49 %
Serosal implants
19 %
Mesenteric involvements
16 %
Peritoneal implants
54 %
Interruption of the anterior peritoneal line
16 %
Liver metastasis
38 %
Lymphadenopathies
24 %
Gallbladder wall thickening
32 %
2.1 Ascites
Ultrasonography is a highly sensitive test in detecting ascites of small volume; (Branney and Wolfe 1995) for example, 5–10 ml ascites are clearly detectable. However, ascites is common in many benign conditions such as liver cirrhosis, portal hypertension, nephrotic syndrome, cardiac insufficiency, etc. (Runyon et al. 1988). Even if ultrasonography is often unable to distinguish between benign and malignant ascites, its presence in patients with known neoplasia is highly suggestive for neoplastic involvement of the peritoneum, and its presence in the lesser omentum (in absence of pancreatitis) is also highly suggestive for malignancy (Dodds et al. 1985). Some ultrasonographic characteristics may be helpful to differentiate benign from malignant ascites.
Frequently, in malignant ascites the fluid is echogenic (due to the presence of blood and/or neoplastic cells) (Fig. 1), septa are often present (Fig. 2), bowel loops are fixed and smashed for mesenteric involvement (Fig. 3), serosal and parietal peritoneal implants are often visible.

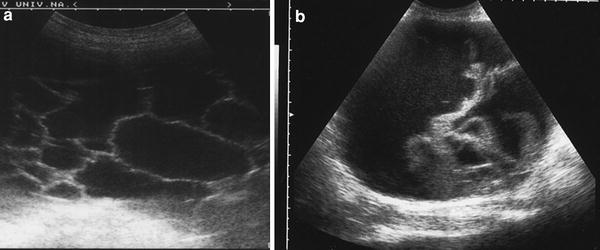
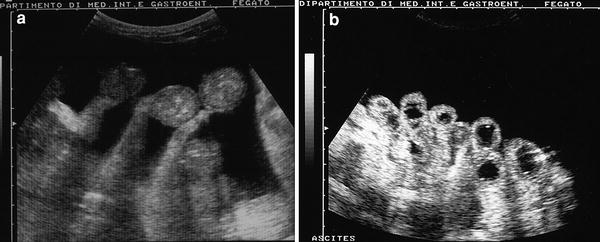

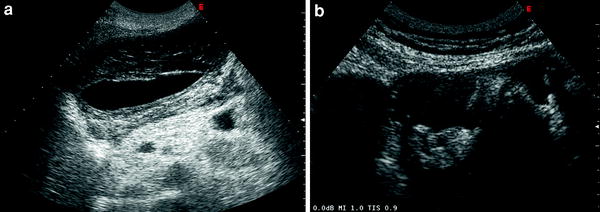
Fig. 1
Echogenic malignant ascites in a case of ovarian cancer: the fluid is echogenic with fine corpuscolated echoes and declivous sediment
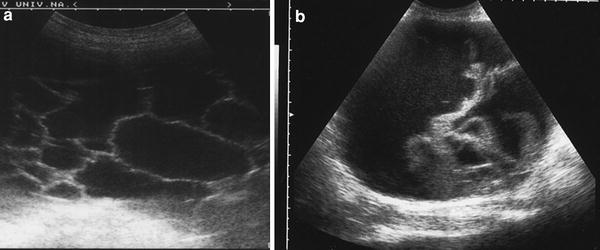
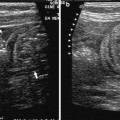
Fig. 2
a Ascites with fine hyperechogenic septa are clearly visible in malignant ascites due to pancreatic cancer. b More evident thickened hyperechogenic septa in malignant ascites due to gastric cancer
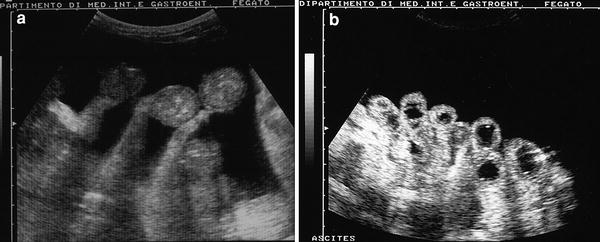
Fig. 3
a A case of benign ascites: note the bowel loops free in the anechoic fluid. b Contrary to what is seen in a, the intestinal loops are fixed and smashed in malignant ascites
Indeed, abundant ascites facilitates visualization of small nodules infiltrating parietal peritoneum, since it acts as a means of contrast (Fig. 4; Goerg and Schwerk 1991).
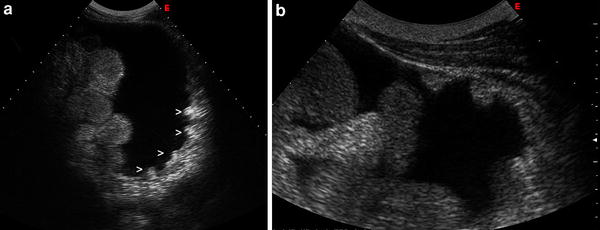
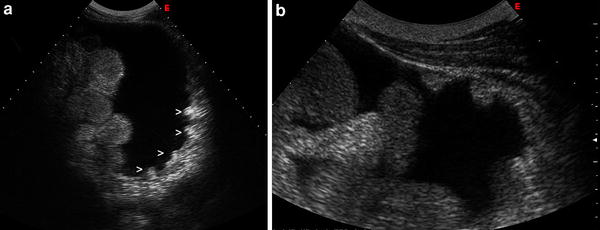
Fig. 4
a Very small nodules (>) are clearly visible on the posterior abdominal wall in a case of peritoneal involvement (colon cancer). b Small solid nodules (arrows) adhering to the anterior abdominal wall in a patient with ovarian cancer
Table 2 summarizes differential ultrasonographic characteristics between benign and malignant ascites; however, significant ascites is present in about 50 % of patients with peritoneal metastasis (Rioux and Michaud 1995).
Table 2
Ultrasonographic differential diagnosis between benign and malignant ascites
Ultrasonographic findings | Benign ascites | Malignant ascites |
|---|---|---|
Echogenic ascites | ± | + + + |
Septa | Absent | Present |
Peritoneal line | Regular | Irregular, interruption, evidence of nodules |
Omentum | Thin | “Omental cake” |
Mesentery | Free | Fixed |
Intestinal loops | Free | Fixed-smashed |
Liver metastasis | Absent | Present |
Lymphadenopathies | Absent | Present |
Other US signs | Liver cirrhosis Pancreatitis Cardiac failure | Absent |
Diagnosis of peritoneal metastatic involvement is often based on fluid analysis and ultrasound-guided aspiration of ascites is frequently used in patients with small amounts of liquid (Fig. 5).


Fig. 5
Ultrasound guided percutaneous fine needle aspiration of ascitic fluid. Note the tip of the needle clearly visible in the fluid
2.2 Omental Involvement
Stein (1977) clearly described the omental band as a new sign of peritoneal metastasis. Neoplastic infiltration of the great omentum is visualized by ultrasound as a uniformly thick, hyposonic band-shaped structure adjacent to the anterior and lateral walls of the abdomen, following the contour of the abdominal convexity and containing low-level non-structural internal echos (omental-cake) (Fig. 6). From this finding, a diffuse metastatic involvement of the omentum can probably be inferred with a high degree of reliability.
Get Clinical Tree app for offline access