Metastatic Lesions of the Bones
Todd M. Blodgett, MD
Alex Ryan, MD
Hesham Amr, MD
Key Facts
Terminology
Bone metastases, metastatic lesions to bone, secondary bone tumors
Imaging Findings
More than 80% of metastases to bone are located in axial skeleton where red marrow blood flow is high
Vertebrae, ribs, and hips
FDG PET generally ineffective for tumors that are not FDG avid
Prostate cancer, highly mucinous tumors, occasionally renal cell carcinoma
Also limited in some sclerotic metastases
o Reveals marrow lesions in FDG-avid disease prior to cortical effects (often before bone scan becomes positive)
CT may miss many early infiltrative or osteolytic lesions
CT has higher sensitivity for osteoblastic/sclerotic bone metastases
F-18 NaF PET: Excellent PET bone agent, currently not reimbursed by Medicare and most third party payers
Top Differential Diagnoses
Degenerative Processes, Arthropathies
Healing Fracture or Bone Injury
Iatrogenic: Vertebroplasty, Kyphoplasty
Physiologic Activity
Primary Bone Tumors
Pathology
Most common childhood primaries: Neuroblastoma, Ewing sarcoma, rhabdosarcoma
TERMINOLOGY
Abbreviations and Synonyms
Bone metastases, metastatic lesions to bone, secondary bone tumors
Sclerotic/osteosclerotic metastases
Osteolytic metastases
Definitions
Malignant extension to bone, often by carcinoma, due to direct extension, retrograde venous flow, or hematogenous metastasis
IMAGING FINDINGS
General Features
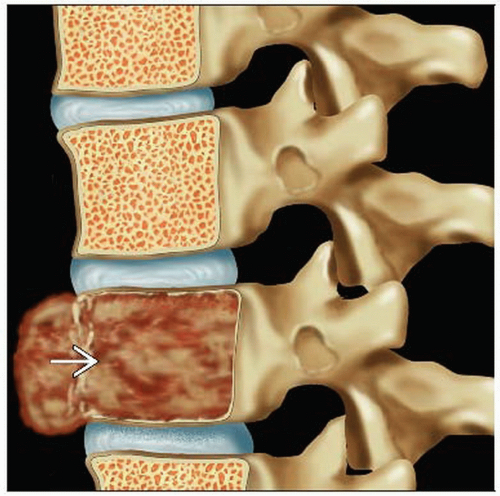
Best diagnostic clue: Typical presentation includes scattered lesions in areas of osteoblastic or osteolytic activity
Location
Seeding occurs mostly in red marrow where blood flow is high
(80%) axial skeleton
Spine, pelvis, ribs, sternum, calvaria, proximal limb bones
Random distribution typical
More common proximally in long bones
Cortical involvement can occur secondary to direct invasion
Size: Ranges from small, solitary lesion to replacement of the entire marrow space
Morphology
Often infiltrating, elongated, or expansile
Focal or regional pattern more characteristic of fracture or arthropathy
May not be identifiable on CT
Imaging Recommendations
Best imaging tool
PET/CT very sensitive for detection of bone metastases
FDG PET sensitive for osteolytic lesions and CT sensitive for osteoblastic lesions
PET/CT more sensitive and specific than bone scan for delineation of disease and for surgical planning
Tc-99m whole body bone scan often used as initial screening due to low cost
Sensitivity 80-90%, better than plain radiograph or CT but nonspecific
More sensitive than FDG PET for osteoblastic lesions
Plain film correlation for further characterization/ambiguity; additional evaluation with CT or MR as necessary
Protocol advice
FDG PET/CT
Position arms above head for whole body scan
CT Findings
More sensitive for osteoblastic/sclerotic lesions
Insensitive for early infiltrative or osteolytic lesions
Early bone infiltration (before destruction) appears as increased attenuation of the normally fatty bone marrow
Increased attenuation of lesions generally correlates with lowered FDG uptake
Overall sensitivity for bone-seeking cancers: 71-100%
Spine
Posterior vertebral body almost always involved
80% also in anterior body
Enhancement often not detectable
Nuclear Medicine Findings
General applications
FDG PET/CT more sensitive and specific than bone scan
Earlier detection of FDG-avid osteolytic marrow lesions (before cortical changes become evident)
Reveals 75% more metastases from breast cancer and to long bones
Exceptions include primaries with low FDG avidity, which are typically osteoblastic
Osteoblastic metastases include prostate, highly mucinous tumors, and occasionally renal cell carcinoma
Sclerotic metastases may not be FDG avid
Prediction of bone metastasis in the absence of associated CT findings is hindered by false positives
Especially with solitary foci
PPV of lesions with negative CT and positive FDG PET: 61%
PPV of lesions positive on CT but negative on PET: 17%
PET/CT may be cost-effective following screening bone scan for more detailed evaluation of bone metastases
Restaging
Overall rate of detection of recurrence for FDG PET and CT separately were 47% and 96%
Following therapy, “flare” phenomenon may present
Treated lesions may have increased FDG uptake during healing and osteoblastic remodeling
Bone pain may increase as well
Typically arises 4-6 weeks post-therapy and resolves within 3-6 months
May show “mixed” response, with a variety of resolved, stable, and new lesions
Response to therapy
Reduction in SUV of metastatic bone lesions following therapy is highly predictive of response
Total lesion glycolysis (TLG) changes were a poor indicator of response duration
Possibly due to lack of volume change in treated lesions
Findings/anatomy
Most common finding: Scattered osseous lesions focused in regions of red marrow, i.e., axial and proximal appendicular skeleton
Solitary lesions more likely inflammatory or degenerative than metastatic
Linear uptake along ribs (single focus of activity in ribs more likely fracture)
Vertebral mets often asymmetric and not confined to endplate
Proximal long bone involvement more common; distal long bone mets seen in lung, thyroid, and renal cell carcinoma
PET can detect tumors confined to marrow space
May have no detectable cortical remodeling and thus not be seen on bone scan
Multiple myeloma, lymphoma, leukemia
Aggressive tumors with overwhelming osteolytic/osteoblastic activity may be photopenic
Renal cell carcinoma, thyroid carcinoma, poorly differentiated anaplastic tumors
Occasionally lung, breast, neuroblastoma, myeloma
Lytic lesions may become photopenic following radiotherapy, often surrounded by reactive rim of activity
“Superscan” MDP bone scan
Diffusely increased activity due to disseminated bone lesions
May show relative absence of normal renal and soft tissue activity
Breast and prostate cancer most common causes
Findings by primary
Breast
FDG PET is sensitive for detection of predominantly osteolytic metastatic breast cancer
Decreased FDG uptake may be seen in sclerotic metastases
Treated, previously lytic metastases may have post-therapy sclerotic changes and lose FDG avidity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree