Author
n
Activity
ORR (MRI/CT) %
ORR (PET) %
OS
Comments
Haug
58
1.8 GBq
25.6
51
47 wks
Changes in SUVmax at 3 months were the only predictor of survival
Paprottka
27
2.08 GBq
59.3
–
–
Bangash
27
109–110 Gy
39.1
63
2.0–9.4 months
Longer OS if ECOG = 0 and tumor burden <25 %
Jakobs
30
1.9 GBq
61
–
11.7 months
1 toxic death
Coldwell
44
2.1 GBq
47
95
1 year OS; 86 %
The high variability in terms of efficacy with the use of RE in BC patients may be partly explained by differences in histologic tumor grading, hormone or Her-2/neu receptor status, tumor burden, performance status or treatment response to RE as assessed by CT or MRI. More recently, the change in SUVmax as assessed by 18F-FDG PET/CT before and 3 months after RE has been identified as the main independent predictor of survival (Haug 2012). A decrease of more than 30 % in the follow-up scan, compared with the baseline examination, indicated therapy response. The response definition was based on the summed percentage change in SUVmax in up to 5 of the most prominent LM, although further studies are warranted to more precisely identify the optimal method for metabolic response assessment. Finally, some authors have suggested that RE was associated with a significant mean decrease in the whole liver volume and an increase in both the diameters of the main portal vein and the splenic volume (Paprottka et al. 2011). Although these changes did not seem to correlate with clinically meaningful sequelae, longer follow-up seems advisable.
3 Lung Cancer
LM from lung cancer represent advanced and incurable disease and thus local therapies are usually contraindicated, because it is without any shown benefit in survival or quality of life. Murthy et al. (2008) described a cohort of six patients with unresectable LM from lung cancer treated with 90Y resin-microspheres after having failed systemic chemotherapy, RF ablation, or arterial embolization. RE was administered as second- to sixth-line therapy. A median dose of 36.1 mCi (range, 12.9–54 mCi) was delivered. A decrease in the size of LM (one patient) and stable disease (two patients) were reported. One patient had a mixed response, and two patients had progression of disease. One grade 3 and one grade 4 liver toxicity occurred. All patients experienced grade 1/2 fatigue. Time to progression of liver disease ranged from 3 to 9 months. The authors concluded that, when the treatment was deemed effective, the duration of local disease control after one treatment seem to equal or exceed what would be expected with chemotherapy.
4 Noncolorectal Gastrointestinal Cancer
Over 200,000 gastrointestinal malignancies are diagnosed annually in the United States, and the liver is the predominant site of metastasis in most of them. Although there have been significant advances in systemic chemotherapy, most patients will eventually succumb to their disease. As a result, much effort has been put forward to develop methods of local liver tumor ablation aimed to achieve improved outcomes.
With the exception of gastric cancer, surgical results for other gastrointestinal primaries remain highly disappointing. The distinctive natural histories and the lower chemoresponsiveness of these tumors turn into a shorter projected survival for advanced disease than for CRC. Therefore, alternative approaches are eagerly awaited in order to bring some hope of long-term survival. For this reason, RE is being increasingly incorporated into treatment strategies, since its effectiveness may rely more on the dependence of a given tumor on its vascular supply than strictly on its chemosensitivity. Moreover, it may be possible to overcome steep dose-response curves for chemotherapy effect by attaining more protracted and locally concentrated levels of radiation near the tumor.
4.1 Pancreatic Cancer
Although pancreatic adenocarcinoma frequently metastasizes to the liver, until now hepatic resection for this disease has never been shown to result in a survival benefit (Takada et al. 1997). Indeed, patients with LM from pancreatic adenocarcinoma usually have a dismal prognosis. Cao et al. reported the results of RE with 90Y resin-microspheres in seven patients with histologically proven pancreatic cancer. Two patients achieved a partial response, whereas stable disease was observed in one patient. Interestingly, one of the responding patients survived for nearly 15 months after RE (Cao et al. 2010). Gibbs et al. (2010) investigated the utility of 90Y resin-microspheres in combination with weekly 5-Fluorouracil (600 mg/m2) in 15 patients with LM from pancreatic adenocarcinoma. Overall response rate was 23 %, with a median progression-free survival of 5.6 months and a median OS of 6.2 months. Extra-hepatic progression was the main cause of death. Further studies of RE in this setting should help to clarify the role of this approach in terms of safety and efficacy.
4.2 Gastric Cancer
Liver metastasis is one of the most common failure patterns of this disease after surgery along with peritoneal dissemination and extensive lymph node metastases. Although isolated LM can be found in 5–9 % of patients with gastric cancer (Koga et al. 1980; Sakamoto et al. 2003; Okuyama et al. 1985), metastatic liver tumors are frequently accompanied by peritoneal dissemination and multiple metastases in both lobes of the liver (Hiratsuka et al. 2003), resulting in a curative resection rate of only 10–15 % (Ochiai et al. 1994). Several authors have reported on limited experiences of liver metastasectomy in selected patients with gastric cancer, with 5 years survival rates ranging from 0 to 38 % (Miyazaki et al. 1997; Ambiru et al. 2001). Intrahepatic recurrence following hepatectomy is found in up to 60 % of the patients. Some variables independently associated with poor survival include bilobar metastasis and a maximum tumor diameter of 4 cm (Ochiai et al. 1994). To date there have been no reports of RE specifically designed for patients with gastric cancer. Cianni et al. (2006) reported on 29 patients with liver metastases that had shown progression despite multiple chemotherapy lines treated with SIR-Spheres. Primaries included pancreas, oesophagus, and gastric cancers. Patients with bilirubin levels greater than 1.8 mg/dL and greater than 20 % lung shunting were excluded. The investigators obtained a response in all cases by imaging or tumor markers. The authors concluded that RE was safe and effective for this pretreated population.
4.3 Cancer of the Biliary Tract
Intrahepatic cholangiocarcinoma (ICC) is a rapidly fatal epithelial cancer originating from the intrahepatic bile ducts whose incidence has increased in developed countries worldwide. The great majority of patients have unresectable disease at the time of diagnosis and most of them ultimately relapse in the liver. Several palliative treatment options are available, including systemic chemotherapy, TACE, radiofrequency ablation, liver transplantation or external-beam radiotherapy. Radiation dose remains a key factor in the local control of this type of tumors. Increased rates and lengths of palliation as well as improved survival have been reported in patients treated with a boost of RT to the tumor as compared with those treated with whole-liver RT alone (Mohiuddin et al. 1996). Moreover, the median survival of patients who received RT doses higher than 70 Gy resembles that seen in surgical series (Dawson 2000). Progression-free survival is also improved in patients who were treated with higher doses of RT. The improved outcome with increasing RT dose does not seem to depend entirely on the fact that smaller tumors received higher doses, because there was not a significant association between dose and tumor volume.
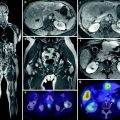
In view of this clinical background, 90Y microspheres RE is emerging as a promising tool in the management of ICC, primarily vascularized by the hepatic artery, given its ability to deliver radiation doses as high as 1,000 Gy to the tumor while sparing the normal tissue. Besides some preliminary case reports suggesting that both, inoperable gallbladder carcinoma and ICC could be safely treated with this procedure (Wijlemans et al. 2011), several groups have reported on the outcome of 90Y RE for the treatment of this disease. Saxena et al. (2010) treated 25 unresectable ICC patients with a partial response being observed in 6 (24 %), stable disease in 11 (48 %), and progressive disease in five patients (20 %). The median survival was 8.1 months, although patients with peripheral tumor type and ECOG score of 0 had the best outcome, with survival times reaching 18 months. Ibrahim et al. treated 24 ICC patients during a 4 years period. On imaging follow-up, 27 % of the patients achieved a partial response. By using EASL guidelines, 77 % of the patients showed a >50 % tumor necrosis. The median survival for patients with an ECOG performance status of 0, 1, and 2 was 31.8, 6.1, and 1 month, respectively, whereas it was 31.8 and 5.7 months for patients with peripheral versus peri ductal-infiltrative tumors (Ibrahim et al. 2008). Coldwell et al. described 23 patients with nodular cholangiocarcinoma treated with SIR-Spheres. All patients had previously received two chemotherapy regimens. The mean activity infused was 1.5 GBq, with a mean tumor dose of 150 Gy. After a median follow-up time of 14 months, median survival was not reached, with 19 of 23 patients being alive at the time of the analysis (Coldwell and Kennedy 2006).
More recently, Hoffmann et al. aimed to retrospectively determine prognostic factors in 33 patients with unresectable ICC treated with RE. Most of them had been pretreated with chemotherapy. Response was assessed at 3 months intervals according to RECIST criteria. Overall, 12 patients achieved a partial response, 17 had stable disease and 5 had progressive disease. Median time to progression and overall survival were 9.8 and 22 months, respectively. Survival times were significantly longer in patients with an ECOG status of 0, tumor burden <25 %, and tumor response to RE (Hoffmann et al. 2012). Other prognostic factors include the presence of portal vein thrombosis (Ibrahim et al. 2008), extensive tumor vascularization in the MAA-SPECT and metabolic response by FDG-PET (Haug et al. 2011).
The results of these trials warrant further prospective investigation. A summary of currently available clinical results with the use of 90Y microspheres RE in ICC is provided in Table 2.
Table 2
Clinical outcome of RE in ICC patients
Author | n | Activity | Response | PFS | OS |
|---|---|---|---|---|---|
Saxena | 25 | 1.76 GBq | 24 % (48 % SD) | – | 9.3 months 2 years OS; 27 % |
Hoffman | 33 | 1.54 GBq | 36.4 % | 9.8 months | 22 months |
Haug | 26 | – | 22 % (MRI) 78 % (PET) | 51 wks | |
Ibrahim | 24 | 105 Gy | 27 % | 14.9 months |
5 Melanoma
Ocular melanoma is an aggressive disease that usually metastasizes to the liver. Overall survival rates have been reported to decrease to less than 1 year after the development of metastases. Although some rare long-term survivors have been reported after hepatectomy, most patients present with unresectable liver disease (Lejeune et al. 1992). Kennedy et al. (2009) reported their experience on 11 patients treated with RE with a mean activity of 1.55 GBq. PET-CT at 3 months showed a response in all patients. More recently, Klingestein et al. (2012) retrospectively evaluated the outcome of 13 metastatic uveal melanoma patients after RE as salvage therapy. Most patients had already undergone dacarbazine-based chemotherapy. The mean activity administered was 1.7 MBq. Eight patients achieved a partial response, and the median survival time after RE was 7 months.
6 Renal Cell Carcinoma
For renal tumors (Wilms’ or adenocarcinoma), the survival times after hepatectomy are close to those achieved for colorectal primaries (Schwartz 1995). Surgical resection of LM in this disease remains a component of total oncologic treatment in carefully selected patients. Factors significant for positive outcome benefit usually include complete resection and a large interval from primary resection to the development of subsequent hepatic metastases. Since these factors are only found in a minority of patients, the role of alternative liver-directed therapies is being actively investigated. A recent report investigated the safety and efficacy of yttrium-90 RE in six patients with liver-dominant renal cell carcinoma refractory to immunotherapy and targeted agents. The median dose delivered was 1.89 GBq. Three patients achieved a complete response, and one additional patient had a partial response. These patients are alive at 64, 55, 17, and 7 months after treatment, respectively, (Abdelmakssoud et al. 2012).
7 Mixed Neoplasia
Jakobs et al. (2007) reported results on 39 treated patients that included metastatic pancreatic cancer, carcinoma of unknown primary, ICC, thymus carcinoma, malignant melanoma, and choroid melanoma. Some evidence of activity was noted, with a median time to progression of 8 months (range 3–11 months). Lim et al. (2005) prospectively evaluated the efficacy and safety of 90Y microspheres in 46 patients with unresectable primary or secondary hepatic malignancies. Tumor types included patients with adenocarcinoma of unknown primary and single cases of hepatic angiosarcoma, gastrointestinal stromal tumor (GIST), ocular melanoma, gastric cancer, pulmonary carcinoid, cholangiocarcinoma, and prostate cancer. With the exception of the single patient with a GIST, activity was not seen in any other tumor type. Popperl et al. (2005) reported on 23 patients with unresectable hepatic malignancies who were not suitable for resection and were no longer responding to polychemotherapy and/or other local forms of treatment. Primary tumors in the mixed group included thymic carcinoma and choroidal melanoma. The mean activity of treatment was 2,270 MBq. Follow-up data showed a marked decrease of FDG uptake, a decrease in tumor marker levels, and unchanged or slightly decreasing lesion size (on CT) in 10 of 13 patients. Wong et al. (2005) described 19 patients with unresectable chemotherapy-refractive hepatic metastatic disease of various origins treated with SIR-Spheres. The median absorbed dose for the tumor was 76 Gy. By PET criteria, 15 of patients (79 %) showed response to therapy, whereas four (21 %) showed no response. Yu et al. (2006) reported on 49 patients with CRC, pancreatic, breast, carcinoid, lung, thyroid, squamous cell, renal-cell, gastrointestinal stromal tumor, and endometrial cancer who underwent 78 administrations of SIR-Spheres. All patients had undergone previous multiple-agent chemotherapy, which had failed. The mean dose of resin-microspheres administered was 0.83 GBq, which translates to 42 Gy absorbed dose. A RECIST response rate of 29 % and a PET response rate of 79 % were noted. Mean and median survival times were 305 and 175 days, respectively. Jakobs et al. (2006) presented midterm results on 88 patients who received 118 administrations of SIR-Spheres. Forty-five of them had CRC, whereas the remaining cases comprised pancreatic, breast, NET, lung thyroid, squamous-cell, GIST, thymus, melanoma, and endometrial cancers, and HCC. All patients had undergone prior chemotherapy. The mean dose infused was 0.83 GBq for lobar and whole-liver treatments. The mean absorbed dose was 42 Gy. The response rate according to RECIST criteria was 18 %, whereas the functional response rate according to PET was 62 %. Mean and median survival times were 285 days and 180 days, respectively. Unfortunately, the inclusion of such a heterogeneous tumor types in these studies adds little to the data on efficacy and reinforce the need for specific disease directed-trials.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree