Fig. 23.1
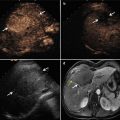
A 39-year-old woman who suffered from adenomyosis for about 5 years, with visual analogue scale (VAS) of 10, hemoglobin 106 g/l. Her uterine size was 11.5 cm × 9.0 cm × 11.3 cm, and the lesions are mainly located in the anterior wall. For her desire to reserve her uterus, she accepted microwave ablation (MWA). (a) Microwave antenna inserted into endometrial-myometrial area and the needle tip (small arrow) close to the far end of lesions (area between large arrows; the yellow arrow indicates endometrium). (b) Two microwave antennas (arrows) worked and the surrounding area turned to hyperechogenic (c) After 60 W × 300 s, by two antennas, the non-perfused area (white star) in contrast-enhanced ultrasound (CEUS) was insufficient, and the triangle means the area that needs supplementary treatment. (d) After supplementary treatment, CEUS was performed again. The non-perfused area was 62.22 % of the lesion, and the triangles indicate the residual disease. (e) Magnetic resonance imaging (MRI) (T2WI) before MWA, which shows the enlargement of the junctional zone (greater than 12 mm) especially in anterior wall with ill-defined margins. And the area between the white long arrows is the target area that needs to be ablated. (f) ce-MRI, 3 days after MWA; the non-perfused area size was sufficient. (g) Three months after MWA, CEUS shows the non-perfused area (between white arrows). The hyperechoes (yellow arrows) in the grayscale sonography are antenna passages. Her menstrual VAS declined to 0, and hemoglobin reached 134 g/l
3.
To avoid damage of the intestinal tract, patients should fast at least 12 h before ablation. Besides, people who have thick abdominal wall always need a bowel preparation. The bladder is another easily injured organ, especially when it is evacuated. Indwelling urinary catheter and occlusion for more than half an hour can solve this matter properly. Because the fully filled bladder can be recognized readily under ultrasound, it can avoid being bladder punctured directly by MWA antenna. The second function of the urinary catheter is to adjust the position of the uterus slightly and make the antenna reach the optimal point. What’s more, the operator needs to observe the color of urine during the therapy.
4.
To avoid vaginal mucosa scalding by thermal gas from the uterine cavity during ablation (once occurred in fibroid ablation), fold fine mesh gauze into ball and infiltrate with cold normal saline, and put two or three of these balls into the patient’s vagina. Besides, these gauze balls also can adjust the uterus’ position to some extent.
5.
For the patients with no clear endometrium under US, putting urinary catheter into the uterine cavity is a commonly used way to make the uterine cavity easy to distinguish. Thus, when MWA is performed, the operator can keep the hyperecho away from the catheter and protect the endometrium easily.
23.7 Therapy Procedures
US-guided MWA should not be performed during the menstrual or ovulatory period.
Patients adopt a supine position. Ablation is performed under intravenous conscious sedation using sodium propofol. Although intestinal tract preparation is done before therapy, a percutaneous approach could have the risk of inadvertently puncturing the bowel in some patients. Pushing the abdominal wall little by little, using a pressed probe before percutaneous puncture, keeps the intestinal tract away from the antenna. Of note is that the shapes of coagulation necrosis are spheroid but not a rigorous sphere. Thus, the needle tip is not inserted into the center of the endometrial-myometrial area, but close to the far end (Fig. 23.1a). Although the border may be poorly defined, the presence of subendometrial linear striations, subendometrial echogenic nodules, asymmetric myometrial thickness, and inhomogeneous hypoechoic areas can be used to identify the margin of nidus in the myometrium [17]. Besides, MRI can also help to recognize the lesion. When the endometrial-myometrial area is less than 3 cm, one antenna is enough, while if it is larger than 3 cm, two antennas are suitable. 50–60 W is the commonly used power in the treatment. The whole procedure is under ultrasonogram monitoring [18]. The antenna could be repositioned until the hyperechogenic signal reaches 3–5 mm from the serosa (Fig. 23.1b) and CEUS shows the non-perfused area reached at least 50 % of the endometrial-myometrial area (Fig. 23.1d). However, once the hyperechogenic signal is found in the uterine cavity, the ablation should be stopped immediately to avoid endometrium impairment.
All vital signs need to be monitored during the whole procedure. The color of urine and gauze balls also should be observed to monitor the bleeding timely.
23.8 Post-ablation Observation
Patients’ temperature, hemorrhage, abdominal pain, and routine blood, urine, and stool tests should be paid close attention to after ablation. From these results, the doctor should judge whether infection and surrounding organ injury have occurred.
Post-ablation ce-MRI is performed within 3 days to evaluate both the possible injury to the surrounding organs accurately and the range of the non-perfused area [19] (Fig. 23.1f). Figures 23.1, 23.2, and 23.3 show the changes of different types of adenomyosis after MWA.



Fig. 23.2
A 35-year-old woman who suffered from adenomyosis with severe dysmenorrhea (VAS 10), hemoglobin 82 g/l. Her uterine size was 8.0 cm × 7.3 cm × 8.2 cm, and the lesions are mainly located in the posterior wall. (a) MRI (T2WI) before MWA, enlargement of the junctional zone especially in the posterior wall, the area between the white arrows is the target area that needs to be ablated. (b) After ablation CEUS was performed and the area between the white arrows shows the non-perfused lesions. The yellow arrow indicates endometrium. (c) ce-MRI, 3 days after MWA; the area between the white arrows shows the lesions in the posterior wall turned to non-perfused

Fig. 23.3
A 43-year-old woman with diffused adenomyosis. Her uterine size was 10.5 cm × 8.7 cm × 7.9 cm. (a) MRI (T2WI) before MWA, enlargement of the diffused junctional zone in the whole uterus; in the posterior wall a small leiomyoma could be found (white arrow). (b) After ablation CEUS was performed and the area between the white arrows shows the non-perfused lesions. The yellow arrow indicates endometrium. (c) Three days after MWA, ce-MRI shows most of the area of the uterus turned to non-perfused (between arrows)
Uterine volumes, hemoglobin, CA125, the questionnaire Uterine Fibroid Symptom and Quality of Life, and dysmenorrhea levels could be used to evaluate effectiveness. Also, serum gonadal hormonal changes and possible complications related to MWA should also be recorded.
According to the reported references, our department has performed the largest number of cases in adenomyosis ablation, so the therapeutic efficacy and experiences of our department will be introduced to make a reference (Table 23.1).
Table 23.1
Comparison of minimally invasive therapy of adenomyosis
Author | No. of patients | Therapy | Operating time (min) | Non-perfused volume ratio (%) | Improvement of symptoms (%) | |
|---|---|---|---|---|---|---|
Within 1 year | Over 1 year | |||||
Kim et al. [30] | 43 | UAE | N/A | 72.1 | 93 | N/A |
Chen et al. [34] | 168 | UAE | N/A | N/A | N/A | 82.4–83.9 |
Pelage et al. [35] | 18 | UAE | N/A | N/A | 80–94 | 55 |
Zhang et al. [32] | 202 | HIFU | 102 | 71.6±19.1 | 79.2 | 79.8 |
Fan et al. [36] | 10 | HIFU | 120–240 | 62.5±21.6 | N/A | N/A |
Zhang et al. [12] | 21 | MWA | 12 | 60–80 | 99.3 | N/A |
Yin et al. [33] | 178 | RFA | N/A | N/A | N/A | 93.3–96.4 |
Uterine enlargement, menorrhagia, and dysmenorrhea are the three most common clinical presentations of adenomyosis. Thus, the decrease of uterine volume and dysmenorrhea level as well as the increase of hemoglobin (hb) can conclude the treatment is effective directly. In our latest perspective study, we performed MWA in 145 patients with a median age of 39.38 years, average uterine size was 278.76 cm3. Most of them show notable improvements after ablation. The size of uterus at 3, 6, 12, and 18 months’ follow-up indicates a decrease of 46.75, 46.88, 44.53, and 32.84 %, respectively, when compared with baseline. And the 3 months’ reduction rate reached 46.75 %, which is much more than UAE and HIFU in literatures [20–22]. These may be because MWA has a relative high thermal efficiency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree