Type 0
Pedunculated intracavitary
Type 1
<50 % intramural
Type 2
≥50 % intramural
Type 3
Contacts endometrium, 100 % intramural
Type 4
Intramural
Type 5
Subserosal ≥50 % intramural
Type 6
Subserosal <50 % intramural
Type 7
Subserosal pedunculated
Type 8
Others (specify, e.g., cervical, parasitic)
1.
Menorrhagia. Defined as prolonged or excessive bleeding at regular intervals, generally blood loss greater than 80 ml per cycle [20] and the blood routine test showing HGB <110 g/L
2.
“Bulk” symptoms. Including excessive pelvic fullness often resulting in urinary tract symptoms (e.g., urinary urgency and frequency), gastrointestinal symptoms (e.g., constipation), and low back pain secondary to pressure
3.
Patients younger than 45 years old and have the strong demand to reserve uterus
4.
Reproductive dysfunction. Patients who are with infertility due to uterine fibroids and require to give birth after treatment
5.
Patients, nulliparous, younger than 30 years old, with average diameter of fibroids >5 cm, though without obvious clinical symptoms and not suitable for treatment under laparoscope and hysteroscope
24.3 Contraindications
1.
Menstrual period, gestation, or lactation period.
2.
Fibroids enlarge quickly in short time and cannot rule out canceration.
3.
Patients with uncontrolled pelvic inflammatory disease.
4.
Severe coagulation disorders, platelet less than 50 × 109/L, prothrombin time >25 s, prothrombin activity <40 %.
5.
Cancer cells found out by cervix TCT examination.
6.
Fibroids classified as type 7 or type 8 according to FIGO classification.
24.4 Evaluation of the Patient for PMWA
24.4.1 Preablation Preparation
All patients considering PMWA require a thorough gynecologic evaluation. The treatment procedures, the expected curative effect, and the potential complications as well as the potential hazardous effect on fertility and adjacent organs are needed to explain in detail to the patients. The applications for treatment and written informed consent will be signed by all the patients. The patients need to take routine blood, urine, and stool examinations along with a test measuring bleeding and clotting time and electrocardiography (ECG).
Contrast-enhanced magnetic resonance imaging (ce-MRI), 2D gray-scale and color Doppler ultrasonography, and pre-contrast-enhanced ultrasonography (CEUS) are performed to evaluate the site, size, and blood supply of the fibroid.
24.4.2 Preclinical Assessment and Imaging
Diagnostic imaging studies are essential not only to confirm the suspected diagnosis of fibroids but also to rule out other malignancies. ce-MRI and transabdominal and endovaginal ultrasounds are extremely helpful in identifying and localizing uterine fibroids. A very small percentage of patients with uterine fibroids will develop leiomyosarcomas (0.2–0.3 %) [21]. If clinical concern for uterine sarcoma exists, image-guided biopsy is indicated.
Women with multiple large fibroids are often adequately evaluated. We devoted specifically to the risk of recurrence after PMWA because of the multiplet [22]; for the sake of safety, we just, in one procedure, ablate the dominant fibroids (the larger fibroids and the main reason of symptoms) and leave alone the smaller ones (<4 cm and not for the symptom reason). For the large type 2 to type 6 fibroids with the diameter >8 cm, we must inform patients the risk of re-ablation, because of the theoretical reason that large coagulation necrosis area may lead to persistent vaginal discharge or bleeding risk.
24.5 MW Ablation Therapy Procedures
24.5.1 Equipments and Procedures
24.5.1.1 MW Tumor Coagulator
A KY 2,000 MW tumor coagulator (Kangyou Medical instruments, Nanjing, China) with a frequency of 2,450 MHz can radiate continuous and pulse MW emission modes. The needle antenna is 15 G in diameter and 20 cm in length. The distance from the aperture of the MW emission to the needle tip is 5–11 mm; the emission aperture is 1 mm. For the antenna, an internal water cycle cooling system is used to lower the temperature of the needle shaft.
24.5.1.2 Sonography System
Using sonography system with a puncture-guided device and low MI contrast-enhanced function. The frequency of the probe is 2.5–4.5 MHz.
The ablation is performed under intravenous conscious sedation. A catheter is inserted and the bladder is filled for a half hour prior to the ablation in order to observe the location of the urinary bladder and its wall before the ablation. The patients receive a supine position. Under ultrasound guidance, if we cannot exclude the possibility of carcinomatous change of fibroid, a biopsy of the fibroid is performed via percutaneous puncture with an 18-gauge core needle for three slips of pathological diagnosis. Along the path of the biopsy, the MW antenna is then inserted into the center of the fibroid. For temperature measurement in real time during the ablation, one thermal couple is placed at a site of 0.5 cm inside the tumor adjacent to the urinary bladder if the fibroid is located at the anterior wall of the uterus, or adjacent to the rectum if the fibroid is located at the posterior wall. The output energy of the MW is set at 50 W. Based on experience from the previous study [23–26] of using MW ablation in vivo griskin, coagulation zones can be induced covering 4.3 cm × 3.1 cm × 2.8 cm (one antenna,50 w, 300 s), 5.1 cm × 3.6 cm × 4.1 cm (one antenna,50 w, 600 s), 5.7 cm × 5.6 cm × 4.8 cm (two antennae,50 w,300 s), and 6.7 cm × 5.9 cm × 5.3 cm (two antennae,50 w, 600 s). A single antenna is used for fibroids with mean diameters <5 cm and with lower perfusion; double antennas are used with an inter-antenna distance of 1 cm for fibroids with mean diameters ≥5 cm or those <5 cm in mean diameter but with rich blood supply. For larger fibroids with mean diameters ≥5 cm, the ablation is first performed using two antennas with 50 W for 300 s, then the antennas are withdrawn by 1 cm for a second ablation. For fibroids with non-spherical volumes, the margin of the thermal field is controlled at the shortest axis diameter, and the antenna is then withdrawn along the long axis or reinserted into the unablated zone for another ablation session. Computer-aided dynamic temperature measurement of microwave-induced thermal distribution is used during multiple-electrode coagulation [27].
During the ablation, variations in the echo from the fibroid are monitored by real-time ultrasonography. The MW therapy is stopped when the hyperecho (caused by microbubbles generated during MW emission and representing roughly the ablation zone) covers the whole nodule [26] or when the measured temperature reaches 60 °C [27], because temperature correlates well with the extent of the coagulation necrosis to ensure that the tumor tissue is completely necrosed. The surveillance of the three-dimensional margin of the high echo was achieved with 2D imaging through continuous scanning in cross sections. When the MW therapy ended, the CEUS is performed. If the CEUS showed the non-perfusion volume ≥80 %, the treatment can be stopped.
24.6 Post-ablation Care
After the PMWA procedure, the patient is transferred to the recovery room and given immediate oxygen and electrocardiograms (ECG) for 30 min.
After recovery, the patient is transferred to the ward and kept for 12 h under close observation for side effects and complications. During the observation time, the patients have access to painkillers and antibiotics. The necessary conditions will be discussed in another section below.
24.7 Efficacy Assessment and Patient Follow-Up
The therapeutic efficacy of PMWA has been documented by:
1.
Assessment of enhanced imaging
2.
Volume reduction of the ablated fibroids
3.
Dosage of HGB
4.
Patients’ reported symptom and quality of life (use UFS-QOL to assess the changes of patients’ symptoms and quality of life [28])
5.
Ovarian function (sex hormone and fertility)
6.
Recurrence or reoperation
7.
Adverse reactions and complications
The patients’ menstrual information during the first few days after PMWA were recorded. Patients are requested to come back for a recheck at regular intervals thereafter (3, 6, and12 months and then 1 year). An ultrasound scan, appropriate blood work, and the UFS-QOL assessments were obtained at every follow-up visit. MRI and CEUS are the imaging modalities of choice after PMWA [29]. Generally speaking, submucosal fibroids have a higher chance to discharge necrotic masses and larger discharged tissue volume than intramural fibroids, while the subserous uterine fibroids are nearly impossible to discharge necrotic masses because of no connection with the vagina [30]. There are reports of women with pedunculated subserosal fibroids who have sloughed necrotic fibroids into the pelvis after UAE [31, 32]. Hence, we do not recommend PMWA for fibroids of this type. The long-term effect of PMWA on ovarian function has not been completed understood; however, studies on ovarian-related hormone and effects on fertility are under way.
24.8 Possible Adverse Effect and Complications of PMWA and Defensive Measures
24.8.1 Infection and Fever
Strict aseptic manipulation could reduce the risk of hospital-borne infections, while large area of necrotic tissue may lead to absorption fever. If the fever is caused by infection, we can give no special handling except for drinking more water. Otherwise, some measures can be taken.
24.8.2 Pelvic Pain
Use the visual analog scale to assess the pain. If the score is higher than 5–6, painkiller could be used.
The visual analog scale (VAS) is a line 10 cm in length with each end anchored by extreme descriptive. Patients are asked to mark on the line that represented their level of perceived pain intensity [33].
24.8.3 Watery Vaginal Discharge or Colporrhagia
Reduce the risk of uterine infection. When the symptom lasts for a short time, instruct the patients to pay attention to sanitation, and generally, the symptom would disappear automatically. If not or the fluid has smell, some clinical intervening measure must be taken.
24.8.4 Skin or Vaginal Mucous Membrane Burn
For skin security, water-cooled microwave ablation instrument has been applied in clinical to protect skin burn. We can stuff several vaginal yarn balls doused in physiological saline before PMWA which can protect the vagina mucosa from the hot liquid discharged from vaginal.
24.8.5 Transient and Permanent Amenorrhea
Protecting the endometrium is considered as the core measures. Some defensive measures can be taken. A 5 F double-lumen balloon urinary catheter is placed into the cervix under direct visualization. The balloon is filled with 1–1.5 ml of saline solution to fix the catheter and prevent saline backflow. Then, 1 ml sterile ultrasound gel is slowly injected through the urethral catheter. Endometrium can be marked and covered with this “protective film” from microwave heat by taking this exploratory measure. However, it is presently on its trial stage (Fig. 24.1).


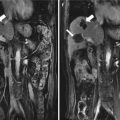
Fig. 24.1
Percutaneous microwave ablation (MWA) in a 29-year-old woman with two type 3 fibroids with the sizes of 3.4 × 3.1 cm and 4.2 × 4.8 cm who was nulliparous. Because the fibroids are in contact with the endometrium, some defensive measures were taken to protect the endometrium. A 5 F double-lumen balloon urinary catheter was placed into the cavity. The balloon was filled with 1.5 ml of saline solution (arrow a). Then, 1 ml sterile ultrasound gel was slowly injected through the urethral catheter to mark the endometrium (arrow b). On the same section of ultrasound, the fibroids cannot be shown
24.8.6 Uterine Perforation or Injuries to Adjacent Organs
First, before PMWA, nursing crux includes gastrointestinal preparation. Second, fill the posterior vaginal fornix with gauze rolls soaked in sterile physiological saline, which play a role similar to uterine manipulator. Third, if the fibroids are close to the intestine or the patient has a retroverted uterus, the investigator can puncture the posterior vaginal fornix then inject sterile physiological saline into the uterus-rectum nest before ablation to separate the fibroids from the surrounding tissue to protect the adjacent organs from heat.
24.9 Results
PMWA is a minimally invasive technique for the treatment of uterine fibroid and adenomyosis by inducing tissue necrosis through heat. Most of the heat generated during MWA was accounted for the rotation of dipole molecules. The pre-ablation 2D grey-scale US showed fibroids of low echogenicity and CEUS showed enhancement within the fibroid. Immediately after MWA, the 2D grey-scale US showed the scheduled treated area was covered with hyperechoic zone and the CEUS showed no enhancement in the ablation zone and with circle enhancement in the periphery of the fibroid (Fig. 24.2). The preablation ce-MRI showed the fibroid was obviously enhanced (Fig. 24.3). After the ablation, ce-MRI showed no enhancement in the ablated zone like “black hole.” Several studies have been reported. The results are listed in Table 24.2. All of them used US to evaluate the fibroid volume. A paper published in 2011 [18] showed the shrinkage rates of the fibroid were 61.8 %, 78.7 %, 73.2 %, and 93.1 % at 3, 6, 9, and 12 months after ablation, respectively. 15 % (6/40) of patients felt pain in their lower abdomens or waists within 12 h post ablation, and the discomfort rapidly disappeared. 17.5 % (7/40) of patients had a small amount of vaginal bloody secretions within 1–2 weeks after treatment, and they recovered from the bleeding without any therapy after 1 week.



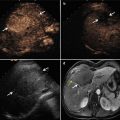
Fig. 24.2
Percutaneous MWA in a 31-year-old woman with a single subserous fibroid in posterior uterine wall. (a) Preablation two-dimensional gray-scale ultrasonography shows the hypoechoic fibroid (arrows) with the size of 4.4 × 4.9 cm. (b) Pre-contrast-enhanced ultrasonography scan obtained during the early phase after contrast injection, and at 17 s it shows homogeneous hyper-enhancement (arrows). (c) Two-dimensional gray-scale immediately after MWA shows the scheduled treated area is covered with hyperechoic zone (arrows). (d) Post-contrast-enhanced ultrasonography immediately after microwave ablation shows the ablation area is consecutively non-enhanced (arrows)

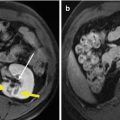
Fig. 24.3
Percutaneous MWA in a 39-year-old woman with an intramural fibroid who suffered from menorrhagia and refused surgical treatment.MWA was implemented to relieve her symptom. (a) Preablation sagittal T1W1 contrast-enhanced magnetic resonance imaging (ce-MRI) scan showed one enhancement intramural fibroid (arrows) with the size of 7.9 × 6.9 cm. (b) Scan obtained 3 days after ablation shows the ablated fibroid (red arrows) without enhancement shrink to 4.9 × 4.5 cm, which is surrounded by the unablated belt (black arrows) with 0.5 cm in width
Table 24.2
Shrinkage rates of the fibroids treated by microwave ablation
Study | Number of fibroids | Baseline (cm3) | Shrinkage rates of the fibroids | |||
|---|---|---|---|---|---|---|
3-month | 6-month | 12-month | 24-month | |||
Zhang et al. [18] | 40 | 140.1 ± 87.4 | 61.80 % | 78.70 % | 93.10 % | N/A |
Qu et al. [34] | 17 | 137.6 ± 61.3 | N/A | N/A | 44.70 % | N/A |
Chunying et al. [35] | 20 | 69.3 ± 7.3 | N/A | 75.20 % | N/A | N/A |
Jun et al. [36] | 16 | 47.8 ± 26.0 | 57.30 % | 66.80 % | 79.90 % | 92.50 % |
Based on our previous study, from October 2007 to October 2013, 240 patients were treated with PMWA in our departments (22 patients with 22 submucosal fibroids, 128 patients with 157 intramural fibroids, and 90 patents with subserosal 120 fibroids). 239 patients completed the therapy in a single ablation. One with a large fibroid diameter of 10.2 cm underwent two steps of PMWA to ensure the safety (4 months between two treatments), and the outcomes are satisfactory. All the patients with submucosal fibroids and 30 ones with intramural fibroids had iron deficiency anemia. The dosages of HGB are all recovered normally at mean 6-month follow-up.
Patient-reported symptom severity decreased from baseline (56.3 ± 19.3) to 24 months (11.8 ± 6.9), and health-related quality of life improved from baseline (50.0 ± 10.8) to 24 months (86.0 ± 12.3).
Two (0.8 %) patients encountered recurrence at 9-month and 13-month follow-up respectively and received re-ablations (recurrence is defined as the appearance of a fibroid on ultrasound examination or identification of fibroid during subsequent surgery after the initial ablation [37]).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree