Authors
No. of patients
Tumor size (cm)
Image guidance
Microwave frequency (MHz)
Output power (W)
Follow-up period (month)
Complete ablation (%)
Local treatment response (%)
Survival rate
1
2
3 years
He et al. [5]
12
2.0–6.0
Ultrasound
2,450
100
20 (6–40)
56.3 %
100 %
N/A
N/A
N/A
Lu et al. [6]
69
2.2 (0.8–5.5)
CT
915
60
36
N/A
78.3 %
66.7 %
44.9 %
24.6 %
Little et al. [7]
23
1.9 (0.8–5.7)
CT
2,450
180
7.3 (3–19)
N/A
88 %
N/A
N/A
N/A
Carrafiello et al. [8]
16
3.8 (2.8–4.7)
CT
915
45
1–18
94.1 %
N/A
N/A
N/A
N/A
Liu et al. [9]
15
2.4 (0.8–4.0)
CT
2,450
180
12 (6–18)
56 %
69 %
N/A
N/A
N/A
Wolf et al. [10]
50
3.5 ± 1.6
CT
915
60
10
N/A
67 ± 10 %
65 %
55 %
45 %
Belfiore et al. [11]
56
3.0 ± 0.9
CT
N/A
55
3–36
N/A
100 %
69 %
54 %
49 %
Feng et al. [12]
20
3.7 (2.0–4.6)
CT
2,450
65
12.4 (3–24)
57.1 %
100 %
40 %
10 %
N/A

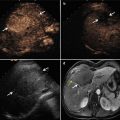
Fig. 25.1
Images of a 76-year-old patient with right lobe squamous cell carcinoma who had complete response from microwave ablation. (a) Computed tomography scan pre-microwave ablation shows the approximately 3.7 × 2.9 cm mass with high attenuation in the right lobe (arrow). (b) Computed tomography scan at 1 month shows that the ablation range completely covers the tumor and a cavitating structure developing at the site of the ablated lesion (arrow). (c) Computed tomography scan at 12 months shows the tumor shrank with complete necrosis, along with small persistent cavitation (arrow)
The advantages of MWA in the treatment of lung tumors are its safety, efficiency, less invasiveness, easy performance, low cost, and decreased associated hospitalization as compared with traditional pneumonectomy. MWA represents a potential safe and effective percutaneous technique in the treatment of lung malignancies, with a potential optimistic impact on patients’ survival. MWA may be a valid treatment option in lung malignancies and it may improve survival in patients that are not suitable to surgery.
25.2 MWA in Breast Cancer
As widespread screening for breast cancer is detecting more women at younger ages and earlier stages, the need for minimally invasive, cosmetically preferable approaches to its treatment is growing. For small breast carcinomas, the survival difference between mastectomy and breast-conserving surgery with combined radiation therapy is not striking, and the latter approach has been accepted as a standard of care by both patients and doctors. However, about 20 % of patients are not satisfied with the cosmetic outcomes after such breast-conserving therapies.
Ablative techniques are now being applied to the treatment of primary breast tumors, perhaps offering an alternative to surgical excision. Clinical experiences of using MWA for breast cancer are limited. Focused microwave phased array thermotherapy was used in the treatment of breast tumor before 2010, with a complete ablation rate of 0–8 % [13–15]. This microwave treatment system uses transcutaneous opposing microwave waveguide applicators and produces a phase-focused microwave field in the compressed breast to heat and destroy high-water-, high-ion-content tumor tissue with tumoricidal temperature over 43 °C by externally focused 915 MHz microwave energy [16, 17]. The first pilot study of the feasibility and efficacy of ultrasonography-guided percutaneous microwave coagulation of small breast cancers was carried by Zhou and colleagues in 2012 [18]. Thirty eight (93 %) of 41 cases patients were diagnosed with invasive ductal carcinoma and three (7 %) were diagnosed with ductal carcinoma in situ. The mean greatest diameter of the tumor was 2.5 cm ± 0.8 (range, 1.0–4.0 cm). The microwave irradiation frequency is 2,450 MHz and output power of 40 W was selected. The irradiating segment of 2 mm in length is 1 cm away from the shaft tip. The mean time to reach complete ablation was 4.48 min, ranging from 3 to 10 min. Thirty seven of 41 cases (90 %) showed complete tumor coagulation. Of three ductal carcinoma in situ cases, only one (33 %) achieved complete tumor necrosis. Complete ablation was achieved in 36 (95 %) of 38 invasive ductal carcinoma cases. To avoid heat injury to the overlying skin, noninvasive skin surface temperature probes were applied to the skin and fans provided constant air cooling [13]. All of the trials conducted up to now have followed ablative therapies with surgical excision, and axillary dissection was performed if the sentinel node contained metastatic cancer or if no sentinel node was found [17]. In this manner, both the completeness of ablation and the margin status can be assessed.
Recently, we treated one patient with breast fibroadenoma 1.2 × 0.6 × 1.1 cm with percutaneous MWA under ultrasound guidance (Fig. 25.2a–d). The microwave irradiation frequency was 2,450 MHz, and output power of 20 W was selected. The total radiation time was 250 s. Postprocedural contrast-enhanced ultrasound examination showed complete ablation of the mass (Fig. 25.2e, f). The only side effect in the patient was pain, which did not require any treatment and resolved spontaneously. The patient was satisfied with the cosmetic result after treatment. The use of ultrasonography-guided percutaneous MWA in the management of breast fibroadenoma is safe and with favorable cosmetic results compared to surgical treatment, although it may require long-term follow-up. The limited follow-up and the fact that only one patient was treated make it incapable to assess the long effects of the mass reduction degree and local sensation change. Several concerns should be considered in MWA. First, patient selection before ablation is very important. Patients with ductal carcinoma in situ are unsuitable for MWA. Second, ultrasonography may underestimate the extent of the tumor, which can cause incomplete ablation. MR imaging should be considered to evaluate the extent of the tumor, guide the placement of the antenna, monitor the procedure, and evaluate the efficacy of the therapy. Third, the time and extent of sentinel lymph node mapping and complete axillary dissection should also be taken into consideration before ablation. The absence of cellular viability in the tumor tissue must be demonstrated by the long-term follow-up in patients who do not undergo surgery. Comparison of the local tumor progression and survival rates between patients treated with MWA and patients treated with the standard therapy should also be assessed. However, MWA represents exciting new approach to in situ tumor treatment.