Authors
Tumor number
Tumor size (cm)
Antenna type
Frequency (MHz)
Complete reaction (%)
Local recurrence (%)
Complication (%)
Median follow-up (months)
Liang et al. [18]
12
2.5
Cooled tip
2,450
100
0
0
11
Carrafiello et al. [19]
12
2.0
Cooled tip
915
100
0
0
6
Muto et al. [21]
10
2.75
Cooled tip
915
100
0
0
13
Bai et al. [22]
23
2.8
Cooled tip
2,450
94.4
0
0
20
Yu et al. [23]
46
3.0
Cooled tip
2,450
98
0
0
20.1
Castle et al. [24]
10
3.65
Cooled tip
915
NA
38
40
18
Except the short-term and intermediate-term studies of MWA in RCC which were reported by our group previously, now we are collecting the patient volume and prolonging the follow-up to provide further clinical effect results of MWA for small RCC. The results showed that US-guided MWA was performed for 102 renal tumors (size range, 0.6–4.0 cm; mean size, 2.7 ± 0.9 cm) in 97 patients (70 men and 27 women; age range, 22–87 years; mean age, 65.0 ± 14.4 years) between April 2006 and December 2013. There were 92 patients with one nodule and five patients with two nodules. Among all the 102 lesions, 32 (31.4 %) lesions were located adjacent to the bowel or renal pelvis (distance between tumor margin and bowel/renal pelvis less than 5 mm). Ninety-seven patients received a total of 119 session (mean 1.2 ± 0.4, from 1 to 2) treatments with MWA for all the tumors. Eighty-five nodules were successfully treated by one MWA session, and 17 nodules were offered two sessions. Desired temperatures were attained in no more than 1,080 s (range, 150–1,080; mean, 448.8 ± 168.1 s). Median follow-up was 23.7 months (range, 3–89.4 months). Based on follow-up imaging, TE was achieved in all the tumors and metastasis-free and LTP-free rates were 94.8 % (92/97) and 98.0 % (100/102), respectively. Two LTPs were discovered at 5 and 32 months after MWA with an initial nodule size of 2.7 and 3.7 cm, respectively. Therapeutic options offered to patients with LTP included radiotherapy for one patient and radical nephrectomy for one patient. Eight of the 97 patients died during follow-up as a result of non-RCC causes in six patients (one stomach bleeding, one heart failure, one hepatocellular carcinoma, one liver failure, and two coronary heart disease, respectively) and RCC progression cause in two patients after MWA. The 1-, 3-, and 5-year overall survival rates were 98.4, 96.7, and 96.7 %, respectively. The 1-, 3-, and 5-year disease-free survival rates were 96.0, 88.3, and 84.3 %, respectively. The ablation zone was well defined on contrast-enhanced MRI/CT and contrast-enhanced US, and it gradually shrank with time (Figs. 17.1, 17.2, and 17.3). Six major complications (5.0 %, 6/119) occurred after 119 MWA sessions including one hepatic encephalopathy with liver dysfunction, one urinary fistula that had diabetes and high-risk tumor location adjacent to the renal collecting system, one bowel perforation with tumor adjacent to the colon, one arteriovenous fistula, one pleural effusion, and one ascites needing drainage. The hepatic encephalopathy patient was successfully treated by intravenous hepatoprotective medicine for 1 week, and the urinary fistula patient was cured by intravenous anti-infective and antidiabetic medicine for 10 days. Bowel perforation was cured by enterostomy and intravenous anti-infective for 40 days. Arteriovenous fistula was successfully treated by percutaneous injection of thrombin at fistula with a 21 gauge needle and the patient discharged 3 days later. Two effusion patients were treated by drainage and recovered 2–3 days later. Another minor complication case of perinephric hematoma occurred which was controlled by medicine therapy. MWA showed no significant side effect on patient’s serum urea nitrogen and creatinine level. And renal function in patients with preablation renal insufficiency did not worsen enough to necessitate dialysis.








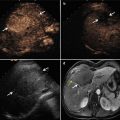
Fig. 17.1
Microwave ablation (MWA) in an 87-year-old man with right renal cell carcinoma (RCC), who was unable to undergo nephrectomy because of coronary heart disease. (a) Preablation conventional ultrasound (US) scan shows a hypoechoic lesion with rich blood supply (arrows). (b ) Contrast-enhanced US before MWA shows tumor enhancement in arterial phase with the size of 4.0 × 3.6 cm (mark). (c) Conventional US shows two microwave antennas (long arrow) are placed in the tumor and one temperature monitor (short arrow) is placed at the tumor margin during the MWA procedure. (d) Conventional US shows hyperechoic ball formed by microwave emitting covers the tumor. (e) Contrast-enhanced US shows no enhancement of the ablation zone at 3 days after treatment (mark)

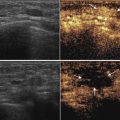
Fig. 17.2
MWA in a 45-year-old man with right RCC adjacent to the renal pelvis. (a) Preablation arterial phase magnetic resonance imaging (MRI) scan shows one heterogeneous enhancement of neoplasm (arrow) near the renal pelvis with the size of 2.4 × 1.9 cm. (b) Arterial phase MRI scan obtained 2 months after ablation shows hypoattenuating ablation zone (arrow) without enhancement. (c) Scan obtained 12 months after ablation shows hypoattenuating ablation zone (arrow) without enhancement corresponding to treated region. (d) Scan obtained 24 months after ablation shows diminishing hypoattenuating ablation zone (arrow) without enhancement

Fig. 17.3




MWA in a 51-year-old man with left RCC, who has a solitary kidney for nephrectomy for right RCC 1 year ago. (a) Preablation MRI scan shows one hypoattenuating neoplasm (short arrow) near the renal pelvis (long arrows) with the size of 3.0 × 2.6 cm. (b) Arterial phase MRI scan obtained 64 months after ablation shows hypoattenuating ablation zone (arrows) without enhancement and there is no renal pelvis injury
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree