Fig. 12.1
Magnetic resonance imaging (MRI) findings in a 45-year-old woman with hepatocellular carcinoma (HCC). (a) Contrast-enhanced MRI scan shows a lesion with hyperenhancement images near diaphragm (arrow); (b) arterial phase in contrast-enhanced ultrasound (CEUS) shows one hyperenhancement lesions (arrow) with the size of 5.4 × 4.9 cm; (c) MRI scan obtained 3 months after MWA shows a signal area with no enhancement, suggestive of complete necrosis (arrow); (d) CEUS scan obtained 3 months after MWA shows a hypoechoic area with no enhancement, suggestive of complete necrosis (arrow)

Fig. 12.2
Contrast-enhanced MRI in a 56-year-old man who underwent MWA of HCC. (a) Hepatic delay phase preablation image shows an HCC (arrow); (b) hepatic T2 preablation image shows an HCC (arrow) with the size of 2.0 × 1.8 cm; (c) hepatic transverse image after 6 months of postablation shows a nonenhancing zone of hypointensity enveloping the tumor (arrow); (d) hepatic coronal plane image after 6 months of postablation shows a nonenhancing zone of hypointensity enveloping the tumor (arrow)
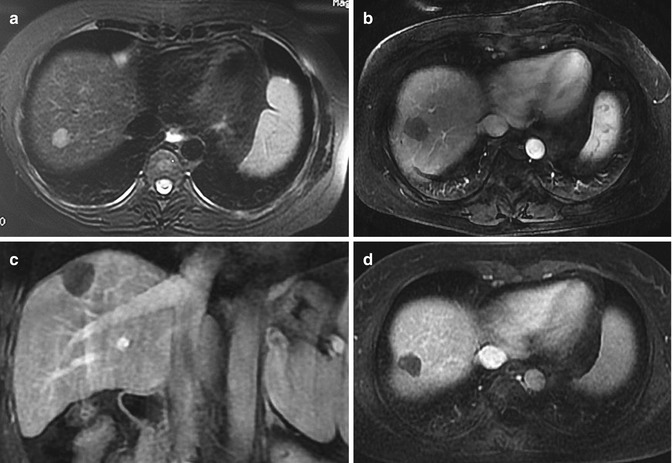
Fig. 12.3
Contrast-enhanced MRI in a 42-year-old man who underwent MWA of HCC. (a) Hepatic T2 preablation image shows an HCC (arrow) with the size of 1.6 × 1.4 cm; (b) MRI scan obtained 3 months after MWA shows a signal area with no enhancement, suggestive of complete necrosis (arrow); (c) hepatic coronal plane image after 12 months of postablation shows a nonenhancing zone of hypointensity enveloping the tumor (arrow); (d) hepatic transverse image postablation 12 months shows a nonenhancing zone of hypointensity enveloping the tumor (arrow)
This study shows that the technique effectiveness rate of MWA of tumor adjacent to the diaphragm is similar with the control group with the tumor not near the diaphragm. No obvious difference of the recurrence rate and survival rate was found between the two groups. And this research result is consistent with other reports using RFA [7, 8]. The rate of complications is low in our study. One reason is the application of the cooled-shaft antennas which could easily avoid skin burn. Another reason of low incidence rate of complications is that we performed percutaneous MWA assisted with temperature monitoring, which could avoid damage to adjacent organs.
Meanwhile, US has its limits. Some nodule adjacent to the diaphragm still cannot be displayed clearly even using artificial pleural effusion. In this situation, other MWA techniques are feasible, such as MRI-/CT-guided MWA, laparotomy MWA and laparoscope-guided MWA. But there were no reports of the application of these technologies in tumors near the diaphragm so far (Figs. 12.1, 12.2, and 12.3).
12.6 Complications
Side effects and complications of thermal ablation for lesions adjacent to the diaphragm include pleural effusion, pneumothorax, diaphragmatic muscle injury, mild bleeding, skin burn, pain, slight fever, nausea, and vomiting [9, 10]. Li et al. [5] reported nine cases (10.1 %) suffered from mild or moderate right shoulder pain which ranged in duration from 2 to 13 days, with a mean duration of 6.5 days; two cases (2.2 %) suffered from severe right shoulder pain which needed analgesics for control and ranged in 10 days’ duration, followed by mild pain for 2 months; and 21 cases (23.6 %) developed pleural effusion. Of these 21 cases, 18 cases had a small amount of pleural effusion and had the symptoms self-relieved in 1 week, and three cases had a moderate or great amount of pleural effusion and were treated by placement of a tube drain. Nausea and vomiting developed in eight cases (9.0 %) and disappeared within 1–2 days after ablation.
In our study, 227 patients had no immediate serious complications. Only seven cases (3.1 %) had a small amount of pleural effusion without special treatment. One case had a moderate amount of pleural effusion with the treatment of a tube drain, and the symptom was relieved in 1 week. Fifty cases had a low-grade fever (not more than 38.1 °C), and the temperature reduced to normal within 1–7 days without special treatments. Also, there were some patients who had moderate pain. The pain disappeared spontaneously without any special treatment within 2 weeks.
12.7 Other Local Techniques
Other local therapies have been employed to treat HCC near the diaphragm (Table 12.1).
Table 12.1
The curative effect of a variety of minimally invasive techniques in HCC near the diaphragm
Author | Method | No. of patients | Size (cm) | Technique effectiveness rate (%) | 1-year survival rate (%) | 2-year survival rate (%) | 3-year survival rate (%) | 4-year survival rate (%) | Follow-up (month) | Locoregional recurrence rate (%) |
|---|---|---|---|---|---|---|---|---|---|---|
Shiina et al. [18] | RFA | 118 | N/A | 100 | 97 | 91 | N/A | 74 | N/A | 2 |
Lin et al. [19] | RFA | 52 | ≤4 | 96 | 90 | 82 | N/A | N/A | 24.5 ± 11.3 | 18 |
Lin et al. [19] | PEI | 62 | N/A
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|