Fig. 20.1
Procedures of microwave ablation (MWA) in a 50-year-old woman with recrudescent pheochromocytoma, who had undergone surgical resection for right pheochromocytoma (size, 10 × 8 × 6 cm). (a) Six months after the surgery, conventional ultrasound scan shows a right adrenal lesion with the size of 3.2 × 2.3 cm, which is then treated with MWA. (b) Thirty months after the first MWA, the ablated lesion (1) volume is decreased, and a new lesion (2) is found. (c) Contrast-enhanced ultrasound before the second MWA shows tumor enhancement in arterial phase with the size of 3.0 × 2.5 cm. (d) Through artificial liquid chest catheterization (arrow), normal saline (star) is injected between the right lung and liver, which may prevent the right lung from heat injury during MWA. (e) MWA procedure is performed. (f) Contrast-enhanced US shows no enhancement of the ablation zone 3 days after MWA


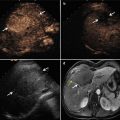
Fig. 20.2
MWA in a 64-year-old man with left adrenal metastasis (3.1 × 2.6 cm), who had hepatocellular carcinoma treated with transarterial chemoembolization 1 year ago. (a) Contrast-enhanced ultrasound scan obtained before ablation shows tumor enhancement (arrow) at arterial phase. (b) T2WI on MRI scan obtained before ablation shows a well-demarcated tumor (arrow) on the left adrenal. (c) MRI scan obtained 6 months after ablation shows hypointense ablation zone (arrow) at the site of treated left adrenal tumor, suggesting the absence of new tumor progression. (d) MRI scan obtained 15 months after ablation shows hypointense ablation zone (arrow) of treated left adrenal tumor
20.7 Other Treatments of Adrenal Tumors
20.7.1 Radiofrequency Ablation
RFA is performed by using the alternating current via radiofrequency pulses to create friction, which can result in the heating of cells and resultant cell death and/or tissue necrosis [7]. RFA is being increasingly used for cure or palliation of different tumors in the liver, kidney, lung, musculoskeletal system, and adrenal glands. However, percutaneous RFA of adrenal tumors is still a relatively new procedure compared with the more widespread application for hepatic and renal tumors [14]. For adrenal tumors, RFA has been used a little more widely than MWA. The literatures demonstrate the successful use of RFA as a technique in the adjuvant treatment of primary functional adrenal neoplasm and adrenal malignancies. According to the study of Mendiratta et al., RFA was employed in 13 patients with symptomatic functional adrenal neoplasm no more than 3.2 cm in diameter. (Ten patients with aldosteronoma, one patient with cortisol-secreting tumor, one patient with testosterone-secretingtumor, and one patient with pheochromocytoma) [7]. All patients experienced resolution of clinical symptoms or syndromes including hypertension, hypokalemia, Cushing’s syndrome, or virilizing symptoms. Technical success was confirmed in all cases by immediate post-procedure imaging. The mean clinical follow-up was 41.4 months (range, 12–106 months). All patients demonstrated resolution of clinical findings 1 year after treatment. For the patients with aldosteronoma, improvements in hypertension management were noted. The mean blood pressure before ablation was 149/90 mmHg, which decreased to 122/77 mmHg at a mean of 2.8 months after ablation and 124/75 mmHg at a mean of 41.4 months. There were two minor complications including one small pneumothorax and one limited hemothorax, neither of which required overnight admission. Lo et al. performed CT-guided RFA on a 71-year-old patient with painful bilateral adrenal metastases from lung cancer [15]. The left adrenal mass was 4.7 cm and right mass was 4.3 cm. The patient experienced marked relief in pain bilaterally after the treatment. On further follow-up of 6 months, the patient noted a lack of endocrine sequelae and continued pain relief.
RFA treatment has limitations. It is difficult to treat all adrenal tumors because some of them are hypervascular and the size of tumor is too big. Combination therapy with RFA and adrenal arterial chemoembolization has been confirmed as a safe therapeutic option that can lengthen survival among patients with adrenal metastasis from hepatocellular carcinoma [16]. Six patients with eight adrenal metastatic lesions were treated. The mean maximum diameter was 5.2 ± 1.8 cm (range, 3.5–8.0 cm). One patient has isolated adrenal metastatic lesions, but the other five patients had four associated intrahepatic lesions and three extra-adrenal distant metastatic lesions. Tumor enhancement of all eight adrenal tumors ceased on contrast-enhanced CT scans and no major complications were related to combination therapy. During the mean follow-up period of 37.7 ± 27.6 months (range, 4.0–70.9 months), two of eight adrenal tumors (25 %) had local tumor progression. The median survival time was 24.9 months; however, three patients treated for both intrahepatic and extrahepatic lesions survived longer than 4 years.
Brook et al. described the imaging findings after RFA of 14 patients with adrenal tumors [2]. Immediate soft tissue findings after RFA included fat stranding around the adrenal gland in 13 patients (93 %) and air bubbles in 12 patients (86 %). A fat rim sign was found in 60 % of patients at long-term follow-up. In addition, the author reported that the expected side effects were found in 35 % of patients: in two patients adjacent liver parenchyma was ablated, in two patients the diaphragmatic crus was injured, and in two patients local hematoma occurred (in one patient, both adjacent liver and diaphragmatic crus were ablated). Complication rate was 14 %, including one case of small pneumothorax and one case of small hemothorax.
20.7.2 Cryoablation
Cryoablation relies on rapid freezing and thawing to cause rupture of cell membranes resulting in cell death [1]. Cryoablation probes are inserted in the target lesion and temperatures from −80 °C to less than −150 °C are achievable by rapidly propelling argon gas at high pressures through the probe into an area of lower pressure [17]. This change from the high to low pressure system necessitates absorption of heat from the surrounding tissues via the Joule-Thomson effect, which creates the surrounding ice ball [1]. Advantages of cryoablation rather than heat thermal ablation are the ability to see ice ball on CT and decreased degree of pain [1].
Cryoablation of the adrenal gland is a promising technique for percutaneous treatment of adrenal metastasis, with limited experience reported in the literature. Twelve patients with single adrenal metastasis were treated with percutaneous adrenal cryoablation [17]. Local control was achieved in 11 of 12 tumors (92 %) after treatment. One patient with adrenal insufficiency underwent conservative ablation and developed adrenal recurrence which was retreated. Six patients developed hypertensive crisis during or immediately after cryoablation procedure. Patients with adrenal cryoablation experienced a significant increase in systolic blood pressure, pulse pressure, and mean arterial pressure compared with kidney cryoablation patients.
20.7.3 Laser Ablation
Laser is an acronym for light amplification by stimulated emission of radiation. Laser technology directs collimated, monochromatic, coherent, and powerful light energy to a well-delimited area of tissue in a predictable, precise, and controlled manner [18]. About 80 % of tissue is destroyed by energy absorption; and because of coagulation of microvessels and ischemic injury, cell death may continue for up to 72 h after laser ablation [18]. The maximum diameter of the near-spherical lesions can reach 1.2–1.6 mm with a bare fiber; lesion size can be increased by simultaneous deployment of multiple fibers in an array [18].
Laser ablation is not widely used in adrenal tumors as RFA according to searchable literatures. Vogl et al. performed CT-guided Nd:YAG laser ablation on nine patients with nine unilateral adrenal metastases from primaries comprising colorectal carcinoma, renal cell carcinoma, esophageal carcinoma, carcinoid tumors, and hepatocellular carcinoma [10]. The mean diameter of tumors was 4.3 cm. The average number of laser applicators per tumor was 1.9 (range, 1–4) and mean applied laser energy was 33 KJ (range, 15.3–94.6 KJ). All patients tolerated the procedure well with local anesthesia and no complications occurred. Complete ablation was achieved in seven lesions; progression was detected in two lesions in the follow-up.
20.7.4 Chemical Ablation
Ethanol and acetic acid are the most common chemical ablation agents, which accomplish tumor necrosis by degenerating cellular cytoplasm, denaturing cellular proteins, and developing irreversible vascular thrombosis of small vessels supping the tumor [19]. Although chemical ablation has been used to treat neoplasm of the liver, lung, thyroid, and other organs [20–22], only a few reports treated with chemical ablation for adrenal tumor have been published [9, 19]. Percutaneous ethanol or acetic acid injection may be useful for small lesions, but they are not sufficiently effective for larger tumors. In the article of 37 patients with 46 adrenal tumors treated with CT-guided percutaneous chemical ablation [19], the complete response rate was 92.3 % (24/26) and partial response rate was 7.7 % (2/26) for primary tumors, but for metastasis, complete response rate was 30 % (6/20) and partial response rate was 70 % (14/20). Their results suggested that benign tumors less than 3 cm in diameter can be treated completely with one to three percutaneous ethanol injections, and for tumors more than 3 cm in diameter, tumor size regressed gradually after acetic acid injection. For malignant tumors, acetic acid may control or delay the malignant progression because they may be associated with higher incidence of residual or recurrent tumors [19]. For functional tumors, the level of corticosteroid in five patients with Cushing’s syndrome was normal 3 months after the procedure. However, for functional aldosteronomas, blood pressure did not decrease obviously after the procedure because of arteriolar sclerosis caused by long-term hypertension [19].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree