Author
No of pts
Power (W)
Ablation time (mins)
Spleen ablation ratio (%)
WBC level
PLT level
Fever (%)
Pain (%)
Hydrothorax (%)
Transient hemoglobinuria (%)
Delayed hemorrhage (%)
Ecchymosis (%)
Liang P et al. [14]
20
70–90
10
30.9 ± 13 (16–58)
Peaked at 7 days then decreased
Peaked at 14 days then decreased
80
70
20
70
No
No
Jiang YZ et al. [32]
5
70–120
27.2 (10–44)
7.04–28.60
Peaked at 2–3 days then decreased
Peaked at 6 months then remained at normal level
No
No
No
No
20
No
Han JB et al. [33]
13
60
30
34.20 ± 1.72
Higher significantly
Increased significantly
No
No
No
No
No
No
Yi YX et al. [34]
16
60
30
35.73 ± 4.04
Higher significantly
Increased significantly
No
No
No
No
20
13
22.5 Assistant Techniques
Thermal monitor instrument can be used for avoiding overheating and assessing accurate treatment efficacy. Put one to two thermocouples about 0.5 cm away from the target and the hilar vessels. It can reduce the occurrence rate of residues and injury of major vessels.
For tumors located in the upper pole of the spleen or hypersplenism which have no approach toward the lower pole of the spleen, establishment of the left artificial pleural effusion before ablation can help keep the approach safe by exposing the lesion clearly. Besides, it can effectively reduce the pulmonary complications and referred pain. The detailed procedure is just the same as artificial pleural effusion combined with MWA of liver tumors. The volume of the normal saline is usually about 500–1,000 mL.
22.6 Therapeutic Efficacy Assessment
For secondary splenomegaly and hypersplenism, the coagulation size and volume of one ablation can be estimated according to the results of a previous in vivo study [19], while the exact ablated splenic volume can be calculated using 3D contrast-enhanced CT scans with a section thickness of 1.25 mm 7 days after ablation. For microwave ablation of spleen tumors, all patients undergo CEUS examination 1 day after MVA to assess the efficacy. Once residues are found, further course is planned. Patients without residues enter the follow-up protocol which consisted of contrast-enhanced CT/MRI and/or CEUS at 1, 3, and 6 months after MW ablation and every 6 months thereafter. For thermal ablation for trauma, blood routine and CT are helpful to assess the status of hemorrhage.
22.7 Clinical Efficacy of MWA
22.7.1 Secondary Splenomegaly and Hypersplenism
Results of selected clinical studies are summarized in Table 22.1. Most of the reports showed a result that the more volumes were ablated (over 40–50 %), the better the clinical outcomes were. WBC level, PLT level, and liver functions reached a peak level at a short time after treatment, but decreased overtime. According to Duan et al. [26], partial MW ablation of the spleen improved levels of peripheral lymphocyte subsets. Percentages of CD3+ and CD4+ cells increased rapidly one month after MW ablation therapy. According to the latest study data in China, they evaluated the effects of MWA in 38 patients (M:F = 25:13; age range, 45–65 years) with hepatic cirrhosis caused by hepatitis B and C (30:8). At a follow-up period that ranged from 3 to 24 months, the ratio of ablation volume ranged from 20 to 40 %. Blood cells (mainly PLT and WBC) started to increase at the 1st week, and 45 % (17/38) of patients peaked at 3 months, 32 % (12/38) at 6 months, 13 % (5/38) at 12 months, and 10 % (4/38) at 24 months. The clinical symptoms of fatigue, bleeding gums, and skin ecchymosis definitely improved.
22.7.2 Spleen Tumor
According to our latest study data, we evaluated the feasibility and effects of MWA in seven patients (M:F = 2:5; age range, 32–56 years) with two benign splenic nodules (diameter range, 5.9–6.3 cm) and six malignant nodules (diameter range, 1.3–2.9 cm). A single antenna was used in two patients and two antennae were used in five patients. The power outputs were 50–60 W for 420–1,030 s. For some patients with the nodules located in the upper pole of the spleen (3/4), establishment of the left artificial pleural effusion was taken. All the eight nodules showed no progress for 4–48 months (Fig. 22.1). Almost half of the patients (4/7; 2 are benign and 2 are malignant) were still alive at the end of follow-up. The other three malignant patients died from primary tumor progression.


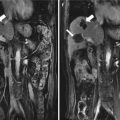
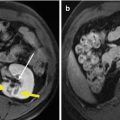
Fig. 22.1
Transverse images and coronal images in a 58-year-old man with a single-focus (2.1 × 1.9 cm) colon cancer metastasis. Transverse contrast-enhanced magnetic resonance imaging (MRI) scan (a) and coronal contrast-enhanced MRI scan (c) before ablation show a well-demarcated tumor (arrow) adjacent to the splenic hilum with mild hyperintensity at arterial phase. Transverse contrast-enhanced MRI scan (b) and coronal contrast-enhanced MRI scan (d) obtained 12 months after ablation show a hypointense zone (arrow) corresponding to treated region
22.8 Complication
Possible complications including intraperitoneal hemorrhage, pleural effusion, fever, pain, and skin burn should be closely observed. For trauma, only one case of massive postoperative bleeding 24 h after laparoscopic RFA was reported, which finally underwent laparotomy for a total splenectomy. For splenic metastasis, there exists the possibility of residuum, peritoneal metastasis, and abdominal incision.
22.9 Other Local Thermal Ablations on the Spleen
22.9.1 Radiofrequency Ablation (RFA)
RFA is more widely used in the spleen worldwide according to the literature published. The indications of RFA for spleen ablation are quite similar with MWA [25], and the application is explored. It is mainly used in hypersplenism, spleen tumor, and spleen trauma at present. Hashemieh M et al. [27] studied the use of RFA on the spleen due to thalassemia, with a result that RFA reduced thrombocytopenia in thalassemic patients with splenomegaly but did not change the hemoglobin levels or transfusion intervals. For hypersplenism, the splenic RF ablation shows good short-term effects. But in the long term, outcomes depended on the ablation volume. Feng et al. [20] demonstrated that hypersplenism syndromes in patients with more than 50 % of the spleen ablated were well controlled. The results were even more prominent when the ablation volume was greater than 70 %. Based on 5 years of follow-up data, after weighing risks and benefits, they concluded that the ideal ablation volume should be between 50 and 70 %. For splenic tumors, Marangio et al. [28] performed RFA on colorectal splenic metastasis. The pathological analyses showed a complete necrosis in the core of the ablated tumor lesion and vital tumor in the peripheral zone. But the result was still encouraging. For splenic injury, Stella M et al. [24] reported the first case of conservative management of a spleen trauma using a cool-tip needle electrode with radiofrequency at 2005. Then Dai et al. [29] reported a case of RF-assisted hemostasis from iatrogenic splenic injury at 2010. A tear at the splenic tip was made during an abdominal operation on the colon. After a failure of using hemostatic agents, 4 min of RF ablation was performed. CT scan of the abdomen showed a minimal degree of splenic infarction. Julien Jarry [30] showed three cases on radiofrequency fulguration of the spleen under laparoscopy to stop iatrogenic hemorrhage. Complete hemostasis was achieved in a median time of 10 min without additional treatments. The blood loss was minimal with no blood transfusion, and splenic hemorrhage is not recurrent during the 20-month follow-up period.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree