Fig. 8.1
Microwave ablation (MWA) in a 64-year-old man with hepatocellular carcinoma (HCC) adjacent to the gallbladder. The tumor size is 2.4 × 2.1 × 1.9 cm. The distance between the gallbladder and tumor is about 1 mm. (a) Preablation contrast-enhanced ultrasound scan (CEUS) shows an HCC lesion (long arrow) located adjacent to the gallbladder (short arrow). (b) A 21-G thermal monitoring needle (long arrow) is inserted to the wall of the gallbladder; the tumor (short arrow) is adjacent to the gallbladder. (c) A 15-G microwave antenna (long arrow) gives out emission, while thermal monitoring needle (short arrow) is used throughout the ablation procedure. (d) A hyperechoic region (long arrow) covers the lesion along the axis of antennas, gallbladder (short arrow). (e) The temperature is measured by the thermocouple. If the temperature reaches 56 °C, microwave emission stops immediately and restarts when the temperature becomes lower than 45 °C. (f) CEUS shows that the tumor adjacent to the gallbladder is still incompletely ablated (long arrow) 3 days after the first session, and then the second MWA session is performed under CEUS guidance. (g) Magnetic resonance imaging (artery phase) shows that the tumor area (long arrow) is totally ablated by microwave (at 1 day after the second session), without injury of the gallbladder (short arrow)
Dehydrated, sterile, 99.5 % ethanol is injected into the tumor very slowly (approximately 1 mL per min) by assistants through one to two 21-G PTC needles at exactly the same time as microwave emission to enlarge the coagulation zone proximal to the gallbladder by diffusion of ethanol. The amount of absolute ethanol injected is determined according to the size and location of the tumor empirically with a gross dose of 5–10 ml. The diffusion of ethanol is also monitored on grayscale US to avoid injecting ethanol into vessels or the gallbladder. All ethanol injections are planned beforehand.
Percutaneous MWA combined with ethanol ablation is performed at the same treatment time.Ethanol is injected slowly during the ablation when microwave emitting. This will enlarge the coagulation zone by the diffusion of hot ethanol.
8.2.3 Clinical Effect
From January 2005 to December 2012, 160 patients with 162 malignant liver tumors adjacent to the gallbladder underwent percutaneous MWA in our hospital. The patient population included 121 men and 39 women (age range, 30–86 years; mean age, 59.6 years). The maximum diameter of the tumors ranged 2.88 ± 1.39 cm × 241±1.31 cm. Eighty-four tumors were located <0.5 cm from the gallbladder and 78 tumors were located 0.6–1.0 cm from the gallbladder. There are 150 patients with primary liver cancer and 10 with metastatic tumors. All patients were successfully treated. There were no treatment-related deaths and no major complications such as cholecystitis or gallbladder perforation in the patients. Complete ablation was achieved in 96.9 % (157/162). During a median follow up of 15 months (range 4 to 27 months), 29(17.9%, 29/162) patients died of progression of primary disease. Among them, four patients grew liver metastases and lost effective treatment. The tumor recurred in local site in five patients; two patients were treated by ethanol ablation and the other three patients by partial hepatectomy, transcatheter arterial chemoembolization, and liver transplantation therapy. Among the five patients, three patients died of tumor progression and two patients died of cardiopulmonary diseases.
The ablation zone was well defined on contrast-enhanced CT/MRI and contrast-enhanced US and shrank gradually over time (Figs. 8.2 and 8.3).



Fig. 8.2
MWA in a 77-year-old man with HCC adjacent to the gallbladder. The tumor size is 3.1 × 3.0 × 3.0 cm. The distance between the gallbladder and tumor is 3 mm. (a) Preablation MRI scan shows an HCC lesion (long arrow) located adjacent to the gallbladder (short arrow). (b) Conventional ultrasound shows that two microwave antennas (long arrow) are placed in the tumor (triangle arrow) and one temperature monitor (short arrow) is placed at the tumor margin during the WMA procedure. (c) MRI (coronal section) shows the tumor area (long arrow) totally ablated by microwave (at 1 month after treatment), without injury to the gallbladder (short arrow). (d) MRI (coronal section) shows the tumor area totally ablated by microwave (at 1 year after treatment). The ablation area (long arrow) shrinks obviously, without injury of the gallbladder (short arrow)

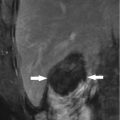
Fig. 8.3
MWA in another 73-year-old man with HCC adjacent to the gallbladder. (a) The tumor size is 4.3 × 3.8 × 3.4 cm. The distance between the gallbladder and tumor is 2 mm. Preablation MRI (T2 phase) scan shows an HCC lesion (long arrow) located adjacent to the gallbladder (short arrow). (b) MRI (portal phase) shows tumor area totally ablated by microwave (at 3 months after ablation). The margin of the ablated area (long arrow) is the wall of the gallbladder (short arrow)
Fang et al. reported 27 hepatic tumors were treated with laparoscopic cholecystectomy (LC) and 16 patients were treated with laparoscopy-assisted MWA [16]. Eighteen lesions were identified to be close to the gallbladder. Laparoscopic cholecystectomy (LC) was first performed. MWA was guided by LC and LUS. The power was 60 W and the time of the therapy was 6–7 min. Complete ablation was achieved in 25 lesions and incomplete ablation in two lesions. There was no mortality in this group. Fang argued that laparoscopic ultrasound (LUS) made a more complete scan to detect the tumors than ultrasound did, and the bleeding in needle ways was easy to control under laparoscopy.
The above reports presented two different kinds of approaches with relatively large cases.
However, the gallbladder wall is incrassate and more collateral circulation can be found in severe liver cirrhosis. Although the thick gallbladder wall can provide more ablation area, collateral circulation would result to massive hemorrhage and would not be helpful in the isolation or resection [17].
8.2.4 Complication
Major complications of thermal ablation to malignant liver tumors adjacent to the gallbladder may include acute cholecystitis or gallbladder perforation, which is different to those in other area [14]. But there are no acute cholecystitis and perforation that appeared in our hospital and in Fang’s report. Thickening of the gallbladder wall, which is not accompanied with acute cholecystitis, was noted 1–3 days after MWA in 51 (31.5 %) patients. The thickness of the gallbladder wall ranged from 3 to 8 mm. There are 39 cases of thickening of the gallbladder wall in the group of tumors located within 0.5 cm of the gallbladder and 12 in the group of tumors located within 0.6–1.0 cm of the gallbladder.
Minor complications are fever, pain, right-side pleural effusion, and nausea like other MWA treatments. After treatment in our hospital, 24 patients experienced grade 1–3 pain at the puncture site according to the standardization of terms and reporting criteria for image-guided tumor ablation [18]. Severe abdominal pain that required the administration of analgesics was noted in ten patients. Thirty-two patients had a fever of 37.5–39.8 °C which persisted for 1–5 days, and nausea occurred in 76 patients. Right-side pleural effusion occurred in seven patients. In Fang’s report, six patients had right upper abdominal pain or precordial region pain, and nine patients had fever. One patient had 480 ml of bloody fluid in the first day, and two patients had mild to moderate dose of ascitic fluid.
8.3 Other Kinds of Ablation and Approach
The most ablation treatments are performed by ultrasound imaging guidance approach. The mainly ablation techniques are focus on MWA, RFA and ethanol ablation, while there are a few reports in laser ablation, high intensity focus ultrasound (HIFU) and cryoablation.
Other imaging-guided approaches include CT, MR, or ultrasound guidance. However, because of the specificity of the gallbladder, which makes the organ easier to detect and observe under ultrasound, and because the gallbladder is a cavity visceral organ, which easily leads to inflammation and perforation, most ablations to malignant liver tumors adjacent to the gallbladder are performed under an ultrasound guide which could be a real-time monitor and make the puncture procedure accurate to avoid gallbladder damage.
The venture of this approach needs more reports. The venture of this approach needed more reports. The cost is higher than the imaging-guided percutaneous approach and the patients are under carbon dioxide pneumoperitoneum.
8.3.1 RFA
Local RFA of liver tumors adjacent to the gallbladder is a feasible and safe procedure, which is first reported by Chopra et al. [19]. More investigators come to the same conclusion regarding with the feasibility and safety of RFA in liver tumors adjacent to gallbladder [20–22].
Sang et al. reports 45 patients with 46 HCC (mean size, 2.2 cm) adjacent to the gallbladder (1.0 cm) treated with RFA using an internally cooled electrode system [20]. The article is the major report of RFA for tumors adjacent to the gallbladder. An electrode was inserted into the tumor either parallel (n = 38) or perpendicular (n = 8) to the gallbladder wall. All procedures were performed under real-time sonographic guidance. The mean time for application of RFA was 12 min (range, 6–15 min). There were no major complications such as cholecystitis or gallbladder perforation in the patient population. Three minor complications were noted: one case of vasovagal syncope and two cases of bilomas. Eight patients complained of severe pain, and pain was controlled with analgesic. Eight patients presented with low-grade fever. Nausea occurred in three patients. Right-side pleural effusion occurred in one patient. Focal wall thickening of the gallbladder adjacent to the RFA zone was noted in 14 cases. Four cases had residual tumors noted which abutted the gallbladder. Two residual unablated tumors were treated again with a second session of RFA, and no residual unablated tumor was seen on 1-month follow-up. Six tumors showed local tumor progression as seen on late follow-up. They drew a conclusion that the direction of electrode insertion (perpendicular), tumor size (>3 cm), and tumor location (a tumor that abutted the gallbladder) were associated with an increased risk of early incomplete treatment, and RFA of an HCC adjacent to the gallbladder can be performed safely and effectively with proper selection of patients and electrode direction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree