The role of magnetic resonance imaging in evaluating patients with inflammatory arthritides has evolved with the recent introduction of drugs capable of modifying disease activity and natural history. In conditions like rheumatoid arthritis, active synovitis and bone marrow inflammation precede and predict bone and cartilage erosion. These imaging findings identify patients who can be treated early and aggressively to prevent future morbidity. Similarly, in gout and other crystalline disorders, specific diagnosis aided by imaging may lead to earlier medical and surgical management. Infected joints need the most rapid identification to institute immediate therapy and prevent irreversible cartilage destruction.
In joints afflicted by degenerative and traumatic arthritis, magnetic resonance (MR) imaging techniques currently emphasize direct morphologic and biochemical imaging of the articular cartilage. Other arthritides primarily destroy cartilage through an inflammatory mechanism. The diagnosis of these conditions, which include primary inflammatory, crystal-induced, and septic arthritides, is typically accomplished with a combination of clinical evaluation, laboratory studies, and radiographs. Radiographs, however, are relatively insensitive to small erosions, and even combined with clinical features cannot prognosticate the disease course. Additionally in these conditions, synovitis and bone marrow changes often precede and predict later chondral disease. A major goal of MR imaging is to identify these precursor lesions before arthritis progresses to bone erosion and cartilage destruction.
For rheumatoid arthritis (RA), seronegative spondyloarthropathies, and related conditions, early diagnosis and staging has become imperative, now that targeted drugs are available to quell the inflammation before cartilage damage occurs. Gout and other crystalline diseases can also affect bone, articular cartilage, and supporting tissues over time, and these complications can be mitigated or avoided with medical and, in some cases, surgical intervention. Septic arthritis, especially bacterial, can irreversibly destroy cartilage and bone in a few days, making immediate diagnosis mandatory so that combined surgical and medical management can be instituted. This article reviews the role of MR imaging in the evaluation of patients with inflammatory, crystalline-induced, and infectious arthritides.
Inflammatory arthritides
The inflammatory arthritides, which include RA, juvenile idiopathic arthritis (JIA), and the seronegative spondyloarthropathies, are a diverse group of systemic diseases that affect the musculoskeletal systems of genetically susceptible individuals. Immune dysregulation, whether in response to an autoantigen or infectious agent, defines a common pathophysiology of activated synovium with pannus formation, resulting in cartilage and joint destruction. Inflammation of extra-articular synovium presents as bursitis and tenosynovitis. Systemic involvement of other organs such as the eye, skin, and viscera can result in significant morbidity and may be prominent features of disease.
RA affects all ethnic groups worldwide, with peak incidence in the fourth through sixth decades of life. Severity is variable, ranging from self-limited to progressive debilitating disease. The classic presentation begins with symmetric involvement of the wrists, metacarpophalangeal joints, and proximal interphalangeal joints. The prevalence of the spondyloarthropathies parallels that of the HLA-B27 haplotype, characterized by axial inflammation of the spine and sacroiliac (SI) joints, and asymmetric peripheral arthritis of the lower extremities and small distal joints of the hands. Enthesitis (inflammation at the attachment of tendon, ligament, or joint capsule), rather than synovitis, is the primary pathologic lesion of the spondyloarthropathies that distinguishes them from RA. JIA describes a heterogeneous group of chronic arthritic conditions with features of rheumatoid and seronegative disease. By definition, JIA presents before age 16 years, but active disease often continues into adulthood. The knee is the most commonly affected joint.
Precise diagnosis of the inflammatory arthritides can be difficult. Classification criteria include a combination of clinical signs and symptoms, radiographic findings, and serologic testing. However, clinical features of the various arthritides may overlap one another, or with other conditions like connective tissue disorders. Radiographs cannot detect synovitis or other soft tissue inflammatory changes that characterize the early stages of disease, and may be relatively insensitive in detecting late findings of erosions and cartilage thinning. Serologic testing is often nonspecific and does not predict disease severity, with one notable exception. Anticyclic citrullinated peptide (anti-CCP) antibody is up to 98% specific for RA, is present in early disease in 70% of patients, and is associated with greater radiologic damage over time compared with RA patients with negative anti-CCP serology.
Historically, treatment of RA and related conditions consisted of steroids and nonsteroidal anti-inflammatory drugs, which improved symptoms but did not prevent disabling and disfiguring joint damage. The advent of disease-modifying antirheumatic drugs (DMARDs) has dramatically changed the management of RA. These drugs prevent joint destruction, especially when initiated early. It is therefore essential to accurately assess disease activity, progression, and response to therapy. The immune cascades, resultant drug targets, and role of MR imaging have been most thoroughly investigated in adult-onset RA.
MR Imaging Technique
The MR imaging examination for inflammatory arthritis should cover critical joints, with adequate spatial resolution to demonstrate erosions and adequate contrast resolution to show bone edema and synovitis. Because rheumatoid and related arthritides commonly affect the hands and/or wrists, screening and staging studies typically image these joints as a surrogate for disease activity throughout the body. Dedicated, extremity MR imaging scanners may be used to detect erosions in hands and wrists, but the lower field strength units on the market are not as sensitive as high-field magnets for detecting bone edema, and there is high intermachine and interobserver variability for identifying synovitis and bone edema using these scanners. In addition, the small field of view for some permanent magnet scanners limits the examination to just a few joints. When using a whole-body scanner for the hands and wrists, a local coil is mandatory to achieve the necessary signal to noise ratio. Imaging can either be performed unilaterally (typically the most symptomatic or the dominant side) with a small whole-volume or surface coil, or bilaterally. The authors have found that bilateral examinations are well tolerated by patients who are positioned decubitus in the scanner, with flexion of their hips, knees, shoulders, and elbows (a modified fetal position), and with their hands in an extremity coil slightly cranial to their heads ( Fig. 1 ). Bilateral imaging is useful whenever symmetry or asymmetry of the findings will affect diagnosis and management.

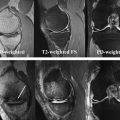
Short repetition time/echo time (TR/TE) spin-echo or fast spin-echo (T1-weighted) images are ideal for visualizing bone marrow, erosions, and synovial thickness. Water-sensitive sequences with fat suppression (T2-weighted fast spin-echo or short-tau inversion recovery [STIR]) demonstrate joint and tenosynovial fluid, marrow edema, soft tissue nodules, and tendons. Fat-suppressed T1-weighted images obtained after intravenous administration of gadolinium-based contrast are used to distinguish enhancing synovitis from nonenhancing effusions (unlike on T2-weighted and STIR images, where both the inflamed synovium and joint effusion demonstrate high signal intensity from increased water content) ( Figs. 2 and 3 ). Contrast-enhanced images demonstrate more findings than T2-weighted images alone, but more importantly, synovial enhancement represents active disease, even in patients with clinical remission. Contrast administration also adds specificity to the examination because whereas small erosions and marrow edema may occur in some patients without inflammatory arthritis, enhancing synovitis and enhancing marrow lesions are rare or absent in healthy subjects. Postcontrast imaging should occur within 10 minutes of injection, as contrast diffusion into the joint space may limit differentiation between synovium and any accompanying joint fluid. Definitions of common MR imaging abnormalities in inflammatory arthritis are summarized in Table 1 .


| Abnormality | MR Imaging Definition |
|---|---|
| Synovitis | Synovial enhancement of a thickness greater than the width of normal synovium |
| Bone edema | Ill-defined lesion in trabecular bone with signal characteristics consistent with increased water content (low T1-weighted and high T2-weighted signal intensity) |
| Bone erosion | Juxta-articular sharply marginated bone lesion with characteristic signal intensity (loss of normal cortical and trabecular T1 signal intensity, and quick postcontrast enhancement indicating pannus within the erosion) that is visible in 2 planes with a cortical break seen in at least 1 plane |
| Tenosynovitis | Increased water content or abnormal enhancement adjacent to a tendon in an area with a tendon sheath |
| Peritendonitis | Increased water content or abnormal enhancement adjacent to a tendon in an area without a tendon sheath |
| Tendonitis | Abnormal thickening and/or signal characteristics consistent with increased water content or abnormal enhancement within a tendon |
| Tendinopathy | Morphologic abnormality (thickening, attenuation or disruption) and/or signal characteristics consistent with increased water content or abnormal enhancement within a tendon |
| Periarticular inflammation | Increased water content or abnormal enhancement at extra-articular sites including periosteum (“periostitis”) and entheses (“enthesitis”), but not the tendon sheaths (“tenosynovitis”) |
| Bone proliferation | Abnormal periarticular (enthesophyte) or articular (ankylosis) bone formation |
The anatomic coverage and imaging planes should address the target joints of the suspected arthritis. For RA, the entire wrist (including the distal radioulnar joint) and at least the metacarpophalangeal joints should be included with both coronal and transverse images ( Fig. 4 ). In psoriasis and disease with more distal distributions, the coil should be positioned to include all of the finger joints and sagittal images can be substituted for coronal images ( Fig. 5 ). The same imaging principles apply when performing MR imaging for other peripheral joints: the examination should use a local coil closely matched in size to the affected joints, image in at least 2 planes, and consist of a combination of short TR/TE, water-sensitive, and postcontrast sequences.


Rheumatoid Arthritis
RA, the most common inflammatory arthritis, affects approximately 25 men and 54 women per 100,000 population. Although the genetic and immune abnormalities responsible for RA have not been fully elucidated, studies indicate that an antigen-specific T-cell response in the synovium initiates an immune cascade, leading to synovial proliferation and pannus formation that subsequently erode subchondral bone and to release of proteases that destroy articular cartilage. Synovitis is responsible for joint pain and swelling, morning stiffness, and development of rheumatoid nodules. In the late stages, fibrosis within the joint can lead to ankylosis (more commonly in JIA than in adult-onset RA), disuse osteoporosis, and muscle atrophy.
Clinical criteria defined by the American College of Rheumatology (ACR) establish a diagnosis of RA. Radiographic findings of joint space narrowing, bony erosion, and joint deformity support the diagnosis and were incorporated into early, validated grading systems. However, these features do not appear until after irreversible joint damage has occurred; ideally an imaging method could show soft tissue and bone findings at an earlier stage, when DMARD therapy would have the most value. MR imaging is currently the ideal imaging modality fulfilling that role.
Guidelines for the use of MR imaging as an outcome measure in RA have been studied and validated by the Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) group, leading to an RA MR imaging scoring system (RAMRIS) for the wrists and metacarpophalangeal joints. The group’s scoring parameters and imaging recommendations, image reference atlases, and sample score sheets are published. Quantified measurements of synovitis, bone marrow edema, and bone erosion correlate with clinical and histologic inflammatory markers, predict disease progression, and demonstrate response to therapy; these findings have also been extrapolated to describe the salient MR imaging features of RA in locations other than the hands and wrists.
The earliest MR imaging finding of RA is synovitis, characterized by thickened synovial tissue and periarticular enhancement on T1-weighted images obtained after intravenous gadolinium-based contrast administration. Symmetric synovitis typically affects the wrists, hands, and feet early in the disease, often first attacking the second and third metacarpophalangeal or finger proximal interphalangeal joints (see Fig. 4 ). In some patients, RA can be accurately diagnosed using MR imaging before they meet the ACR definition. Sugimoto and colleagues found that MR imaging evidence of synovitis in the wrists, metacarpophalangeal, or proximal interphalangeal joints bilaterally, combined with only one clinical finding—either a positive serum rheumatoid factor or arthritis affecting 3 or more joints—predicted development of RA with a 94% accuracy, better than the 81% to 84% accuracy with the traditional diagnostic criteria. Using MR imaging evidence of synovitis to support a diagnosis of early RA is highly sensitive even in patients with absent anti-CCP antibodies. More importantly, regardless of the stage of the disease, MR imaging showing active synovitis is a strong predictor of later erosive disease and affects the decision to begin DMARD therapy in many rheumatology practices.
Bone marrow edema, represented by poorly marginated low signal-intensity foci in the marrow compared with muscle on T1-weighted images and hyperintensity on fat-suppressed, water-sensitive, and STIR images ( Fig. 6 ), is a second important imaging finding in early RA. Histologically these regions actually represent true osteitis with cellular inflammatory infiltrates, not edema (free water) per se, although the term bone “edema” is commonly used nevertheless. There is growing evidence that these infiltrates of activated lymphocytes and osteoclasts may mediate development of erosions from the inside of the bone, which would represent a second mechanism (in addition to bone invasion from the outside by pannus) of erosion formation. Bone edema usually occurs in the presence of synovitis and within the subchondral bone ( Fig. 7 ), but it may occasionally be seen without accompanying synovitis and deeper within bone. In the hands and wrists, the presence of bone edema is the strongest predictor of future development and progression of erosions as well as an independent prognosticator of poor functional outcome.


The third key imaging finding in RA is bone erosions, characterized by circumscribed regions of marrow replacement along articular surfaces associated with disruption of the overlying cortex. Necessitating that erosions meet these criteria in 2 imaging planes will increase specificity and further help distinguish erosions from bone edema ( Fig. 8 ). Erosions are considered a relatively late, irreversible finding in RA, rarely occurring in the absence of synovitis ( Fig. 9 ). Nevertheless, because MR imaging is so much more sensitive than radiographs, it is common to find erosions on MR images even in cases where early disease was expected based on normal radiographs ( Fig. 10 ). Only 20% to 25% of erosions identified on MR imaging will eventually become evident radiographically, and those that do will typically undergo several years of growth before they become visible. Whereas isolated erosions may occur in the normal population, increasing in incidence with age, multiple erosions or erosions seen in the presence of synovitis are highly associated with RA, even in patients with negative serologic tests for anti-CCP antibodies.



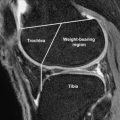
Joint space narrowing from diffuse cartilage loss and focal chondral erosions are features of RA that can be demonstrated on MR imaging, although this is much easier to appreciate in larger articulations rather than in the hand and wrist joints ( Fig. 11 ). Measurements of cartilage volume are excluded from the MR imaging scoring system because of poor reliability in the small joints of the hand and wrist. Similarly, while tenosynovitis often appears in RA patients, scoring of tendon and tendon sheath disease does not enter into systematic scoring systems ( Figs. 12 and 13 ). Rheumatoid nodules are the most common extra-articular manifestation of RA and usually form on the extensor surfaces of the elbow, hand, foot, heel, and ischial tuberosity. These nodules may present as either solid or cystic masses depending on the stage of histopathologic evolution. Although these nodules can be identified with MR imaging, they are typically clinically evident.



In instances when MR imaging of the hands and wrists is normal but there is still strong suspicion of early RA, there may be added value to performing MR imaging examination of the dominant forefoot to assess the metatarsophalangeal joints. After the hands and feet, the cervical spine is the most common site of RA involvement. Larger joints, such as the knee, ankle, and elbow, are usually involved later in the disease ( Fig. 14 ). Synovial proliferation and fluid accumulation within these joints result in expansion of the joint capsule with formation of adjacent bursae ( Fig. 15 ). In large joints, tendon rupture as a result of chronic tenosynovitis or adjacent bursitis is a frequent cause of morbidity in patients with long-standing RA similar to the finger tendons. Commonly involved tendons include the posterior tibialis and rotator cuff ( Fig. 16 ).




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree