(1)
Radiology – Neuroradiology Section, S. Paolo Hospital, Bari, Italy
Great advances have been made in recent years regarding the treatment of spondyloarthropathies.
The aim of spondyloarthritis (SpA) treatment is to control the signs and symptoms of the patient, to prevent joint damage, and to maintain the patient’s quality of life and ability function.
The treatment of spondyloarthritis must be tailored to each patient’s individual case, including the grade of the general conditions, the effectiveness of specific therapies, and the occurrence of any side effects.
A common treatment regimen for all the spondyloarthropathies (ankylosing spondylitis, reactive arthritis, psoriatic arthritis, enteropathic arthritis, and undifferentiated spondyloarthropathy) includes medication and daily exercise (to relax the muscles and reduce joint pain).
The nonsteroidal anti-inflammatory drugs (NSAIDs) are still the first stage of medication in treating the pain and stiffness, but these drugs can cause important side effects or not be effective [1].
The second-line medication is the so-called disease-controlling antirheumatic drugs (sulfasalazine, methotrexate, and corticosteroids) used in the rheumatic and psoriatic arthritis, but these drugs do not have an effectiveness in the ankylosing spondylitis.
New and most promising drugs for ankylosing spondylitis are the biologics, the TNF-blockers. TNF-alpha (tumor necrosis factor-alpha) is a cytokine involved in the inflammatory process. Excess amounts of TNF-alpha have been associated with various forms of inflammatory arthritis.
The treatment with TNF-blockers is recommended after the failure of NSAIDs. The TNF-blockers are very effective drugs and also show a sustained and stable long-term response [2].
The effectiveness of all these drugs can be monitored by MRI imaging. Longer periods of treatment are needed to see further effects of anti-TNF treatment on spinal inflammation as detected by MRI [3, 4].
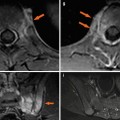
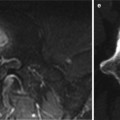
MRI is considered the most sensitive imaging method for detecting inflammatory changes of the spine and sacroiliac joints in the diagnosis of early lesions and follow-up after pharmacological therapy [3, 5].
The active inflammatory lesions are best visualized on fat-suppressed T2-weighted or STIR sequences [6]. This technique has been increasingly used in practice to assess disease activity and to monitor and evaluate therapeutic response [7, 8].
The fat saturated T1-weighted sequences, used after the administration of the contrast agent, seem to be a more specific depiction of inflammatory spinal lesions [6, 9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree