MR imaging, because of its multiplanar capability and superior soft tissue contrast resolution, is the preferred modality to assess osseous and soft tissue structures around the hip joint. This article reviews the clinical presentation, disease process, and imaging findings of important congenital and acquired osseous disorders of the pediatric and adult hip.
Key Points
- •
MR imaging, because of its superior contrast, plays a vital role in the workup of osseous abnormalities of the hip.
- •
MR imaging is an excellent modality to diagnose early Legg-Calvé-Perthes disease and slipped capital femoral epiphysis when radiographs are negative.
- •
MR imaging is essential to differentiate transient synovitis from other serious abnormalities, such as septic arthritis and osteomyelitis.
- •
Avascular necrosis is characterized by the “double line” sign on MR imaging.
- •
MR imaging plays an important role in the assessment of occult fractures, particularly in patients with osteoporosis.
Introduction
Painful conditions of the hip are often difficult to assess clinically, which leads to a reliance on imaging for diagnosis. Although radiography remains the cornerstone of investigation, MR imaging, because of its superior soft tissue resolution, has emerged as the preferred modality for evaluating osseous and soft tissue abnormalities around the hip. This article summarizes the clinical presentation, underlying disease processes, and essential radiologic features of common conditions affecting the osseous structures in the pediatric and adult hip. The first part reviews the pediatric hip conditions of Legg-Calvé-Perthes (LCP) disease, slipped capital femoral epiphysis (SFCE), and developmental dysplasia of the hip (DDH). The second part of the article discusses the clinical features and MR imaging findings of avascular necrosis (AVN) and proximal femoral fractures.
Introduction
Painful conditions of the hip are often difficult to assess clinically, which leads to a reliance on imaging for diagnosis. Although radiography remains the cornerstone of investigation, MR imaging, because of its superior soft tissue resolution, has emerged as the preferred modality for evaluating osseous and soft tissue abnormalities around the hip. This article summarizes the clinical presentation, underlying disease processes, and essential radiologic features of common conditions affecting the osseous structures in the pediatric and adult hip. The first part reviews the pediatric hip conditions of Legg-Calvé-Perthes (LCP) disease, slipped capital femoral epiphysis (SFCE), and developmental dysplasia of the hip (DDH). The second part of the article discusses the clinical features and MR imaging findings of avascular necrosis (AVN) and proximal femoral fractures.
LCP disease
LCP disease is an idiopathic ischemic necrosis of the proximal femoral epiphysis. It usually affects children between 3 and 12 years of age, most commonly between 5 and 7 years. The disease occurs bilaterally in 8% to 20% and is 4 to 5 times more common in boys than girls. Caucasians are more commonly affected with this disease, with a reported annual incidence ranging between 5.1 and 15.6 per 100,000. Most patients with LCP disease have delayed skeletal maturation.
Although the causes of LCP disease is unknown, impairment of the blood supply to the femoral head by extrinsic compression of vessels or intravascular occlusion is believed to be the cause. In some cases, more than one episode of infarction occurs.
Most affected children present with limping caused by groin, thigh, or referred knee pain. The symptoms may sometimes be intermittent. The clinical examination may show restricted internal rotation and muscle atrophy around the hip. The standard radiologic evaluation should include supine anteroposterior neutral (AP) and external rotation-abduction (frog-leg) positions. These views should be obtained at the initial evaluation and follow-up studies.
Radiographic Findings
Radiographic findings of LCP disease are the result of osteonecrosis and subsequent repair. In the early stages of LCP disease, all or some of the following signs may be seen on radiographs: small and sclerotic proximal femoral epiphysis (compared with the contralateral side), ossification center lateralization, and subchondral fissure (crescent sign). Ossification center lateralization is caused by overgrowth of the acetabular cartilage and femoral head cartilage. Subchondral lucency or fissure is commonly seen in the frog-leg position ( Fig. 1 A, B). This fissure appears as a thin line paralleling the outer contour of the anterolateral aspect of the epiphysis. As the disease progresses, resorption and reossification continue simultaneously, giving the fragmented appearance of the femoral head. In advanced stages, flattening and fragmentation associated with deformity, broadening, and lateral subluxation of the femoral epiphysis are seen. These changes are accompanied by broadening and shortening of the femoral neck, with cystic changes along the physis ( Fig. 2 A).
MR Imaging Findings
MR imaging has proved to be sensitive even in the early phase of LCP disease when radiographs are normal or equivocal. MR imaging provides more accurate evaluation of the extent of involvement, staging, prognosis, and complications. A strong correlation exists between the contrast-enhancing areas on MR imaging and the viable tissue of the femoral epiphysis, which is an important factor in predicting prognosis. MR imaging features are variable, depending on the different stages of the disease (ie, necrotic, revascularization, and reparative phase).
Early (necrotic) stage of the disease
On T1-weighted images, linear hypointensity along the periphery of the epiphysis, multiple hypointense lines traversing the epiphysis, or loss of the high signal intensity (normal fat signal) may be seen. On T2-weighted or STIR images, hypointense signal is usually seen in the epiphysis, but bone marrow edema can sometimes cause hyperintense signal (see Fig. 1 C, D). In some cases, the subchondral fracture shows a curvilinear T1 signal hypointensity and T2 signal hyperintensity (crescent sign). The contrast-enhanced images show nonperfusion of the infarcted areas. Reactive synovitis of the involved hip is a constant finding on MR imaging. It is manifested by hypointense T1 signal and hyperintense T2 signal hip effusion with synovial enhancement.
Revascularization and reparative stages of the disease
Resorption and replacement of the dead bone occur simultaneously in these phases, giving the fragmented appearance. Heterogeneous signal intensity is usually seen on T1- and T2-weighted sequences and heterogeneous enhancement correlates with the reossification process. The new vascularized deposited bone shows high signal (marrow fat) on T1 and enhances after gadolinium administration. MR imaging can be used to assess the various deformities of the epiphysis, physis, and metaphysis that may be seen in these stages, and can help predict the outcome of LCP disease (see Fig. 2 B, C). More than 50% involvement of the epiphysis or more than 20% of lateral extrusion of the epiphyseal cartilage is associated with poor prognosis.
The treatment of LCP disease is rest and restricted physical activity until the reparative phase has been established, in which the epiphyseal fragmentation has stabilized and the epiphyseal height is slowly restored.
SCFE
SCFE is a Salter-Harris type 1 shearing fracture of the proximal femoral physis caused by the repetitive stress of weight-bearing. It is the most common hip disorder in adolescents during the period of accelerated growth. The rate of incidence is 10.8 per 100,000 children. SCFE is 2 to 4 times more common in boys than girls. The age of presentation is different between the genders because of difference in puberty; for girls it ranges from 8 to 15 years, with the average incidence at 11 to 12 years; for boys it ranges from 10 to 17 years, with the average incidence at 13 to 14 years. SCFE can be bilateral in 37% of cases, with 18% of them diagnosed simultaneously in both hips at the initial presentation. Most second hip slips occur within 18 months of the first slip. SCFE is more common in black children and observed more frequently in warm weather. SCFE has several predisposing factors, but obesity is the most significant factor; approximately half of the affected children are heavier than the 95th percentile for their age. Other factors include endocrine disorders (primary hypothyroidism, pituitary dysfunction, growth hormone deficiency, and hypogonadism), metabolic disorders (rickets and malnutrition), renal failure osteodystrophy, radiation therapy, chemotherapy, prior hip dysplasia, and Down syndrome. When SCFE is diagnosed in a child younger than 10 years of age, an underlying metabolic or endocrine disorder should be strongly considered.
Children with SCFE usually present with limping and hip or thigh pain, but one-fourth complain of knee pain. Clinical examination may show limited internal rotation and flexion of the hip.
Depending on the degree of femoral head displacement, the slip is classified as preslip (no displacement), mild (displacement less than one-third the diameter of the metaphysis), moderate (displacement between one-third and two-thirds the diameter of the metaphysis), and severe (displacement more than two-thirds the diameter of the metaphysis).
Radiographic Findings
Standard radiologic evaluation should include supine AP projection and a true lateral view. It is better to avoid the external rotation-abduction (frog-leg) position to avoid the stress on the displaced epiphysis. Before the actual slip occurs (preslip phase), the growth plate of the femoral head becomes wide and indistinct on the AP view ( Fig. 3 A). After the slip occurs, a dense line parallel to the physis appears on the metaphyseal side on the AP view (double-density). In a normal hip, a tangential line drawn along the lateral margin of the femoral neck bisects a small portion of the epiphysis (Klein’s line). In SCFE, the portion of the epiphysis lateral to Klein’s line may be absent. When the slippage occurs, the epiphysis moves medial and posterior in respect to the metaphysis. Therefore, the lateral view (or the frog-leg view if obtained) usually delineates the slip much better than the AP view (see Fig. 3 B). In the chronic SCFE cases, periosteal new bone formation can be seen along the femoral neck ( Fig. 4 ).
MR Imaging Findings
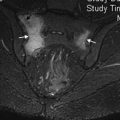
MR imaging is helpful in preslip cases or when radiographs are equivocal. The MR imaging findings of SCFE include focal or diffuse physeal widening, periphyseal bone marrow edema, joint effusion, and synovitis (see Fig. 3 C, D). Bone marrow edema is not a constant finding on MR imaging. T1 and water-sensitive sequences should be obtained in all planes to evaluate the slip, its extent, and associated abnormalities, such as osteonecrosis. The axial oblique plane through the long axis of the femoral neck is essential to evaluate subtle slippage (see Fig. 3 E). MR imaging is also helpful to evaluate the complications of SCFE and its treatment, such as slip progression, early degenerative disease, labral tears, osteonecrosis, chondrolysis, and hardware failure.
The goal of SCFE treatment is to stabilize the slip and prevent further progression, which is achieved through in situ pinning without reduction.
DDH
DDH is a term that includes a spectrum of conditions, from hip instability, anatomic dysplasia (changes in shape and dimensions), to dislocation of the hip (usually posterosuperiorly in relation to the acetabulum). It is defined as a deformity of the acetabulum with associated proper or improper location of the femoral head (congruent, subluxed of dislocated). Lax ligamentous support to the hip may also allow excessive motion and facilitate the dysplasia. Morphologic changes may occur in a newborn or during the early hip development, and the term congenital hip dysplasia should be avoided. The acetabular deformity shifts the expected vertical component of the hip joint force away from the acetabular bone surface toward the superolateral capsular-labrum-complex, which acts as a secondary stabilizer, leading to excessive tension and shear stresses. DDH may be associated with changes of soft tissues, including fibrocartilaginous hypertrophy of the labrum (denominated limbus), hypertrophy of the ridge of acetabular cartilage (neolimbus), ligamentum teres thickening, weakening of the cartilage, and hypertrophy of the acetabular fibro-fatty tissue (pulvinar). Although the exact cutoff separating normal from abnormal morphologic findings is not entirely clear, and because there is likely a continuum of this process, early diagnosis of the disease using modern imaging tests is important to minimize future harm to the hip joint and the development of premature osteoarthritis.
The prevalence of DDH is approximately 1.3 per 1000 children, and 1.2 per 1000 newborns require treatment in North America and Western Europe. Genetic and environmental factors, breech positioning, and being first born are associated with an increased prevalence of DDH. An estimated 80% of persons with DDH are girls.
Screening of DDH in newborns is performed routinely through the physical examination, including the maneuvers of Ortolani (which attempts to reduce a dislocated hip) and Barlow (which attempts to dislocate an unstable hip). The examination may be repeated periodically until the age of 12 months, because the initial examination may fail to diagnose this disorder. Ultrasound and radiographs have not been supported as screening tests. Imaging tests are used for equivocal cases with suspicious physical findings (ultrasound at 6 weeks or pelvic radiography at 4 months). Their use for high-risk cases (girls and boys in breech presentation and girls with a positive family history) is controversial.
Ultrasound Findings
Typically ultrasound is the preferred method for evaluating clinically suspected neonatal dysplasia. Advantages of ultrasound include absence of ionizing radiation, static and dynamic evaluation of the hip, low cost, and portability. The main disadvantage is the need for expertise in obtaining and interpreting the images. The study includes the evaluation of
- •
Acetabular roof angle, labrum angle, and acetabular rim shape
- •
Congruency of the joint, including a dynamic evaluation
- •
Acetabular coverage (equivalent of the radiographic migration percentage)
- •
Soft tissues: pulvinar hypertrophy and limbus interposition for reduction on the dynamic study
- •
Ossification center of the femoral head: asymmetry in dimensions and vascularization of the head
The constellation of parameters helps stage the development of the hip, and may be used in follow-up studies. Ultrasound also evaluates the congruency of the head in patients with the Pavlik harness and after its removal, and during and after closed reduction. The exact protocol to follow may vary among different institutions and societal recommendations.
Radiographic Findings
Radiographs are most useful after 3 to 6 months of age. A frontal supine projection is performed with neutral position of the hips (standing in older children). The absence of ossification during the first months of life and the ionizing radiation are major limitations of radiographic evaluation. Accessory lines of Hilgenreiner (horizontal line through the top of the triradiate cartilages) and Perkins (perpendicular to Hilgenreiner line crossing the lateral margin of the acetabular roof) are used. Some evaluated parameters are
- •
Dimensions and position of the ossification centers of the femoral heads (some asymmetry in dimensions is tolerable). The femoral head ossification center may be smaller in the affected side. The ossification center and the superomedial margin of the femoral metaphysis should project over the inner lower quadrant of the intersection of Hilgenreiner and Perkin lines.
- •
Shenton line: normal when a continuous arch is formed by the lower aspect of the superior pubic ramus and the medial margin of the femoral neck ( Fig. 5 ).
Fig. 5
Pelvic AP radiograph10-year-old patient with right hip DDH shows ( A ) disruption of the Shenton line ( solid arches ) on the right, ( B ) acetabular angle (i) formed between Hilgenreiner line ( dashed line ) and the acetabular roof line ( dotted line ), and the ( C ) center-edge angle (ce), which is the angle between a line perpendicular to the transverse axis of the pelvis ( thin solid line ) and a line through the center of the femoral head and the margin of the acetabular roof ( thick solid line ). The left side has normal center-edge angle value, but an abnormal center-edge angle is seen on the right.
- •
Acetabular index (or inclination angle): angle between the line of Hilgenreiner and the acetabular roof (variable with development; normal below 24° for 1 year of age and below 10° for adults) (see Fig. 5 ).
- •
Center-edge angle of Wiberg: angle between a vertical line perpendicular to the transverse axis of the acetabulum (as Hilgenreiner line) and a line between the center of the head and the lateral margin of the acetabular roof. This angle should be at least 26° in adults (see Fig. 5 ).
- •
Von Rosen line: superior extension of the femoral shaft, which should intersect the acetabulum.
- •
Lateral line: normal when there is a continuous arch from the lateral margins of the iliac wing and the femoral neck.
- •
Migration percentage: percentage of the femoral head lateral to the Perkin line. It should be zero in patients younger than 3 years, and up to 22% for older subjects.
- •
Medial joint space: distance between the medial margin of the ossification center and acetabular wall. This distance should be less than 1.5 mm.
Radiographs may be used before and after treatment at any age. An arthrogram of the hip may rarely be performed during closed reduction to determinate what is preventing the reduction, such as a limbus (hypertrophied labrum with fibrous and cartilaginous overgrowth) or a thickened ligamentum teres.
CT Findings
CT may be used to supplement radiographs or ultrasound before and after surgical management of the hip. The use of CT is infrequent and special care should be used, especially the implementation of a very-low-dose protocol, to decrease the dose of ionizing radiation. Also, CT has a relative high-cost. However, the use of CT is limited by not only its ionizing radiation dose but also its relatively high cost. Advantages of CT include multiplanar and 3-dimensional reconstructions and the relative speed of the study, mitigating the use of sedation.
CT evaluation includes analysis of hip congruency after reduction and casting of the hip ( Fig. 6 ) in the axial plane. In the frog-leg position, a smooth continuity should be present between the anterior aspect of the femoral neck and the pubic bone, with this line being disrupted in dislocated hips. After closed reduction with immobilization in a spica cast, a hip abduction angle greater than 55° is associated with increased risk of AVN of the head. The angle may be calculated between the femoral shaft and the sagittal plane, between the pubic symphysis and coccyx. For severe cases or later diagnosis and treatment in adults, the evaluation of acetabular morphology and version and measurement of femoral head-neck offset may also be measured, before pelvic osteotomy. Arthro-CT can demonstrate intraarticular lesions, including labral injuries, and is sensitive to the presence of chondral defects.