MR in Head & Neck Cancer
Michelle A. Michel, MD
Key Facts
Clinical Implications
MR is optimal imaging tool for precise delineation of tumor margins and identifying perineural tumor, vascular invasion, & marrow infiltration
Excellent soft tissue contrast resolution
Often better tumor characterization, such as parotid
No ionizing radiation & rare gadolinium reactions
Less affected by dental amalgam than CT
Utility of Sequences
Multiplanar imaging important for tumor extent
T1WI delineates anatomic detail of lesion
Fat-suppression techniques on long-TR sequences increase conspicuity and better characterize lesion
T1WI C+ FS further delineates & characterizes tumor and evaluates for perineural & dural/intracranial invasion
DWI & MR perfusion may add further information
Generic Neck Imaging Protocol
Skull base to at least supraclavicular fossa
Slice thickness: 4 mm; interslice gap: 0.5-1 mm
Axial & coronal T1WI
Axial & coronal T2WI FS or STIR
Axial & coronal T1WI C+ FS
Safety Considerations
Gadolinium associated with nephrogenic systemic fibrosis (NSF) in patients with severe kidney disease
MR compatibility of implanted devices & presence of foreign bodies should be determined prior to scanning
Claustrophobia or respiratory problems hinders MR for many H&N patients
Artifacts & Pitfalls
Susceptibility artifacts degrade image quality
Swallowing and motion make neck imaging difficult
TERMINOLOGY
Abbreviations
• Magnetic resonance imaging (MR)
Definitions
• Fundamental imaging modality for evaluating head & neck cancer that does not employ ionizing radiation
CLINICAL IMPLICATIONS
Clinical Importance
MR is optimal imaging tool for precise delineation of tumor margins, orbital and intracranial extension, identifying perineural tumor spread (PNT), and determining vascular invasion & degree of marrow infiltration
Better soft tissue differentiation & contrast resolution as compared to CT
Preferred modality in suprahyoid neck (SHN)
Best for assessment of nasopharyngeal, oral cavity, sinonasal, & salivary neoplasms
Less affected by dental amalgam artifact than CT
Little motion present in SHN
No ionizing radiation
Preferred technique in patients with allergy to iodinated contrast
IMAGING APPROACHES
Staging
In setting of known malignancy, MR can be used to stage primary tumor and lymph nodes
Often obtained after initial CECT
MR evaluation of sinonasal and salivary primaries may be focused and not cover entire neck, as long as CECT covers entire neck for adenopathy
Equipment
Best images obtained with field strengths ≥ 1.5 T
Surface coils greatly improve signal:noise ratio and spatial resolution
Patients must be screened for presence of implantable devices & metallic foreign bodies prior to entering MR environment
Sequences
T1WI delineates fine anatomic detail of lesion, particularly if adjacent to fat
Employing fat-suppression techniques (chemical selective or STIR) on long-TR sequences increases lesion conspicuity
Axial & coronal T1WI C+ FS sequences are superior to CT for defining soft tissue extent, perineural tumor, & dural/intracranial invasion
Fat-suppression increases conspicuity of enhancing lesions adjacent to otherwise hyperintense fat
Fat-suppressed T2 and post-contrast T1 best for identifying nodal necrosis and extranodal spread
Number of signal averages, field of view (FOV), matrix size, & interslice distance adjusted to provide maximum detail and pixel width ≤ 1 mm
IMAGING PROTOCOLS
Neck
Coverage: Skull base to at least supraclavicular fossa
Sequences: 3 sequences, each at least 1 plane
Axial & coronal T1WI
Axial & coronal T2WI FS or STIR
Axial & coronal T1WI C+ FS
± sagittal plane sequence
May be useful for nasopharynx (NP), oral cavity (OC), base of tongue (BOT), palate, & airway lesions
Parameters
FOV: 20-22 cm
Slice thickness: 4 mm; interslice gap: 0.5-1 mm
Matrix: 192 × 256
Surface coils improve image quality
Saturation pulses reduce vascular flow artifacts
Sinonasal
Coverage: Axials (anterior cranial fossa through maxillary alveolus); coronals (nasal vestibule through cavernous sinuses)
Sequences
Axial & coronal T1WI
Axial & coronal T2WI FS or STIR
Axial & coronal T1WI C+ FS
Sagittal sequence optional
Parameters
FOV: 16-18 cm
Slice thickness: 3 mm; interslice gap: 0.5 mm
Surface coil utilized (head coil)
Salivary Glands
Coverage: Top of petrous ridge through mandible
Include course of CN7 for parotid mass evaluation
Sequences & parameters
Similar to sinonasal protocol
Diffusion images may aid in distinguishing benign & malignant lesions
Surface coil utilized (head coil)
Special Techniques
Gauze padding: Oral cavity
Improves visualization of small oral vestibule tumors obscured by apposition of buccal and gingival mucosa
2 × 2 inch rolled gauze inserted into oral vestibule has similar MR appearance to air
Analogous to “puffed cheek” CT technique
Neck padding/“water bags”
Loss of fat suppression often occurs in lower neck/thoracic inlet due to variable width/thickness in extracranial head & neck
Saline bags can reduce bulk susceptibility artifact and improve fat suppression
CLINICAL INDICATIONS & UTILITY
Roles
Multiple roles in H&N cancer patient
Much is due to better delineation of invasion of deep tissues and involvement of critical structures
Preepiglottic fat infiltration
Prevertebral fascia invasion
Laryngeal cartilage penetration
Marrow infiltration
Perineural tumor spread
Orbital fat invasion
Dural and brain invasion
Tracheal & esophageal involvement
Arterial encasement
Brachial plexus involvement
Mediastinal infiltration
Staging
As above, deep extent of tumor best delineated
Tumor volume measurements correlate with local control & outcome for supraglottic, glottic, & pyriform sinus SCCa & NPC
Treatment planning
MR important for determining resectability of primary lesion
Delineation of true extent of tumor important for planning intensity-modulated radiotherapy (IMRT)
Treatment response & surveillance
Baseline imaging after therapy used to assess for residual and as roadmap for future studies
Recurrences occur most often in 1st 2 years after treatment
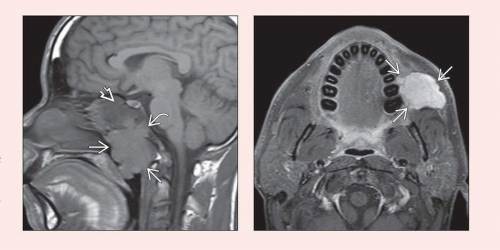
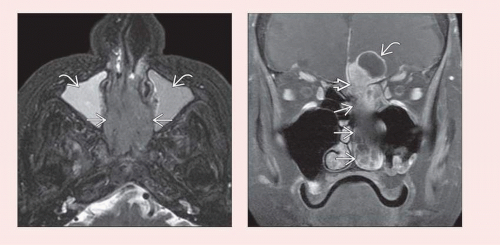
Nasopharynx
MR is superior to CT for detecting small NPC missed on endoscopy, determining deep extension (parapharyngeal space), skull base invasion, & intracranial spread
Skull base invasion may be direct, via PNT, or perivascular
Direct extension through pharyngobasilar fascia or sinus of Morgagni around eustachian tube & levator palatini muscle
Direct marrow infiltration of sphenoid bone, clivus, petrous apex, temporal squamosa
PNT through foramen ovale, hypoglossal canal, &/or to pterygopalatine fossa (PPF)
Perivascular spread along internal carotid artery (ICA) at foramen lacerum then into cavernous sinus
Nonenhanced T1WI best for evaluating skull base and parapharyngeal extension
Tumor replaces normal high signal fat
T1WI C+ FS recommended for detection of PNT
Important to evaluate entire anterograde and retrograde extent of involved cranial nerve
Oral Cavity & Oropharynx
Mucosal extent of oral cavity tumor often best determined on clinical exam
Dental amalgam & dense mandibular bone do not cause prominent artifacts
Small tongue base and palatine tonsil tumors may be invisible on clinical exam
These are frequently more readily detected with MR than CT
Tumor margins & thickness seen well with T2WI
Margin delineation improved with T1WI C+ FS
Tumor > 2 cm with aggressive margins & sublingual space extension likely involves neurovascular bundle
If lesion involves sublingual space, assess for contralateral extension under frenulum & posterior spread to submandibular space
Tumor thickness is prognostic factor for oral tongue SCCa
≤ 3 mm thickness has lower local recurrence rate & excellent disease-free survival
≥ 9 mm thickness has 24% probability of local recurrence & 66% 5-year disease-free survival
Increased incidence of nodal involvement if tumor thickness > 9 mm
Marrow invasion of mandible shows ↓ T1 signal, ↑ T2 or STIR signal, & enhancement on T1WI C+ FS
Reported accuracy for MR detection of mandibular invasion is ˜ 93%
MR may overestimate the degree of marrow invasion
False-positive findings due to presence of inflammation or hemorrhage
Preservation of high T1 signal in retropharyngeal fat reliably predicts absence of prevertebral fascia invasion for posterior pharyngeal wall lesions
Larynx & Hypopharynx
Advantages of soft tissue differentiation of MR often outweighed by motion artifacts in larynx & hypopharynx
Cartilage invasion notoriously missed by CT
On MR, look for loss of normal cartilage fatty signal; cartilage signal follows that of tumor
↓ T1 signal, intermediate T2 signal, contrast enhancement of cartilage marrow space
MR specificity for cartilage invasion: Thyroid (56%), cricoid (87%), arytenoid (95%)
Reactive inflammation, edema, & fibrosis may result in false-positive diagnosis of cartilage invasion
MR better for accurately predicting invasion of cervical esophagus
Wall thickening, effacement of surrounding fat plane, ↑ T2 signal in wall
These findings combined are ˜ 100% sensitive for esophageal involvement
Circumferential mass > 270° is ˜ 100% specific
Sinonasal
MR superior for differentiating neoplasm from mucosal thickening & obstructed secretions
Better for identifying characteristic features of sinonasal malignancies
Superior for identifying SCCa arising in inverted papilloma
Areas of necrosis or loss of convoluted/cerebriform architecture suspicious for carcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree