Ductal carcinoma in situ (DCIS) now makes up 20% to 30% of newly diagnosed breast cancers, an increase in detection that is largely attributed to the advent of screening mammography. Before the advent of screening mammography, DCIS made up about 5% of breast cancers. DCIS is defined as intraductal malignancy that does not extend beyond the basement membrane, and therefore—at least theoretically—has no propensity to metastasize. It is not considered an immediate, life-threatening disease. However, it can progress to invasive disease and can also harbor invasive disease that may not be evident with clinical evaluation or conventional imaging. Thus accurate detection and characterization of DCIS may ultimately have a significant impact on breast cancer survival. Magnetic resonance imaging (MRI) is a highly sensitive imaging tool for detecting invasive breast carcinoma, and it is also very effective for identifying DCIS.
Pathology and Natural History of Ductal Carcinoma in Situ
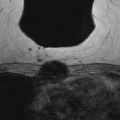
DCIS is a biologically diverse disease. Traditionally, DCIS classification was based on architectural features and divided into two categories based on the presence or absence of comedo necrosis ( Figure 5.1 ).Those without comedo necrosis were further categorized as cribriform, solid, papillary, or micropapillary. However, this categorization is relatively subjective, leading to pathologic inconsistencies and is also not predictive of the potential for recurrence or progression to invasive disease.
Classification based on tumor grade and the presence or absence of necrosis is more predictive of a potential for tumors to recur. Multiple classification schemes based on nuclear grade and the presence or absence of necrosis have been proposed, but investigators have not arrived at a single, universally accepted classification scheme.
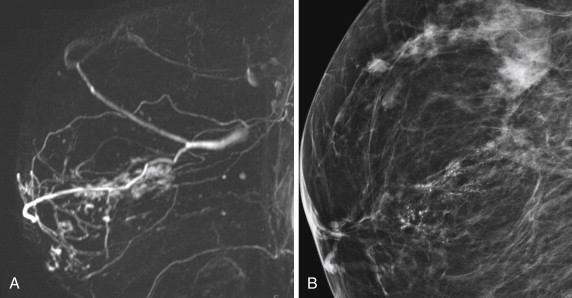
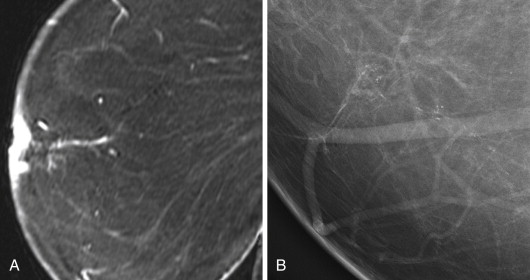
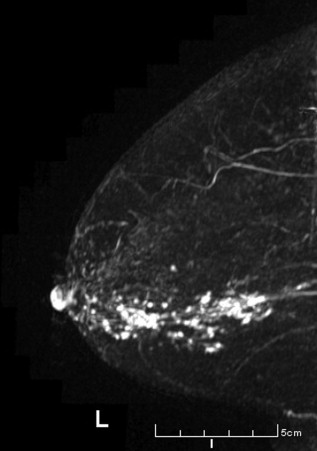
High-grade and non–high-grade DCIS behave differently and have different imaging features on mammography. Most (90%) of DCIS detected with mammography is seen as microcalcifications, but the entire lesion may not calcify. Low-grade DCIS is typically associated with amorphous calcifications, whereas high-grade DCIS is more typically associated with pleomorphic and fine linear branching calcifications ( Figures 5.2 and 5.3 ). However, the mammographic features overlap substantially, and the grade of DCIS cannot reliably be determined by its mammographic features. High-grade lesions are more consistently associated with calcifications; low-grade lesions are more likely to be mammographically occult and more likely to be underestimated in extent by image readers. The degree of underestimation has been shown to be less with higher-grade comedo-type DCIS than for lower-grade micropapillary/cribriform type. A masslike appearance is also possible and may be directly caused by tumor or may be caused by periductal fibrosis or elastosis.
Only 30% to 40% of invasive cancer contains calcifications. Because DCIS is a probable precursor to invasive ductal carcinoma, it has been postulated that the majority of DCIS is not calcified and not detected by mammography.
DCIS grading is similar to that for invasive cancer with low, high, and intermediate grades. Low-grade lesions contain monotonous-appearing cells with small nuclei, minimal nuclear pleomorphism, and infrequent mitoses. Cell polarity with respect to the basement membrane is well preserved. High-grade lesions consist of cells with large pleomorphic nuclei and frequent mitoses, and comedo necrosis is frequently present. Intermediate-grade lesions do not have features of either low- or high-grade lesions ( Figure 5.4 ). Lesions that are heterogeneous in grade are assigned the highest grade present.
Limited information exists about the natural history of DCIS because most is excised. Studies looking at patients with untreated DCIS (probably initially diagnosed as benign with the diagnosis then changed to DCIS after pathologic reevaluation) show a 30% to 50% rate of progression to invasive cancer. Progression to invasive cancer can occur with all nuclear grades, but low-grade lesions seem to progress more slowly than high-grade lesions. As yet, a reliable method has not been found for differentiating lesions that will become invasive from those that will not. However, molecular and genetic evidence exists that high-grade DCIS probably progresses to high-grade invasive cancer and low-grade DCIS probably progresses to low-grade invasive cancer.
DCIS has an excellent prognosis, with 10-year mortality after excision or mastectomy of 2%. Treatment is mastectomy or lumpectomy, generally with radiation. Adjunctive pharmacotherapy can also be used. In the NSABP B-24 trial of lumpectomy followed by breast irradiation with or without tamoxifen, the drug decreased the local recurrence rate for DCIS (8% with tamoxifen vs. 11.1% without). Controversy exists over the need for sentinel node biopsy because, by definition, DCIS is not invasive and so would not be expected to cause nodal metastases; however, axillary nodal metastases are found in 5% to 15% of patients with DCIS. Presumably, metastases developed after the pathologist missed the foci of invasion.
When DCIS recurs, it recurs as invasive cancer in 50% of cases. The reported range for progression to invasive cancer is 14% to 75%. Factors that increase the likelihood of recurrence include young patient age, presence of risk factors for breast cancer, high tumor grade, presence of necrosis, and large lesion size. Evidence is inconsistent that patients with human epidermal growth factor receptor 2 (HER2)-positive tumors and estrogen receptor (ER)-negative tumors have a poorer prognosis.
The most important risk factor for DCIS recurrence is the presence of positive surgical margins after resection. However, universal agreement has not been reached on adequate margin width. Margin widths of 1 to 3 mm have been variably reported as adequate, with the lowest risk of recurrence with a margin width of 10 mm.
MRI Morphologic Features
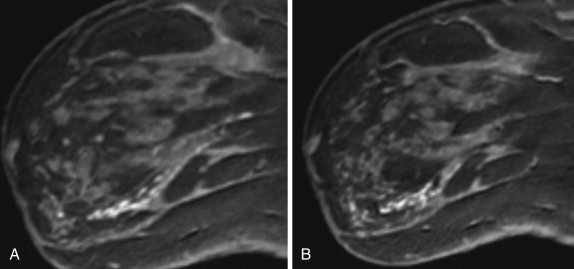
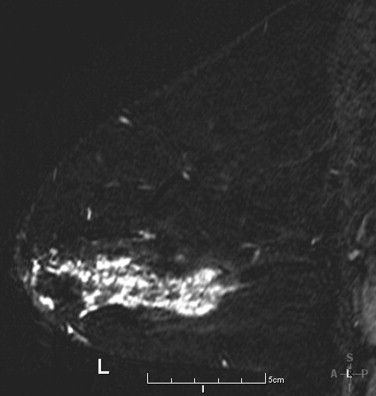
The most common morphologic feature of DCIS on MRI imaging is non–mass-like enhancement (NME), shown in Figure 5.5 . NME is described in the American College of Radiology Breast Imaging Reporting and Data System (BI-RADS) lexicon as enhancement that is not a mass but still is discrete from normal surrounding breast tissue. It is characterized by its distribution and pattern of internal enhancement. In the literature, NME is the reported lesion type in 40% to 82% of DCIS cases, with most studies showing NME in more than half of all DCIS cases. The reported frequencies of distribution types are somewhat variable. This can be attributed to the relatively subjective nature of application of the BI-RADS lexicon descriptors. For example, the same lesion could be described as either a focal area or segmental enhancement by different observers. Although any distribution pattern can be seen, segmental enhancement is the most common. The most commonly reported pattern of internal enhancement for NME lesions is clumped enhancement ( Figure 5.6 ). Clumped enhancement can be described as closely associated, rounded areas of enhancement reminiscent of cobblestones. DCIS appears as a mass in 14% to 60% of cases. Mass margins are most commonly described as irregular.
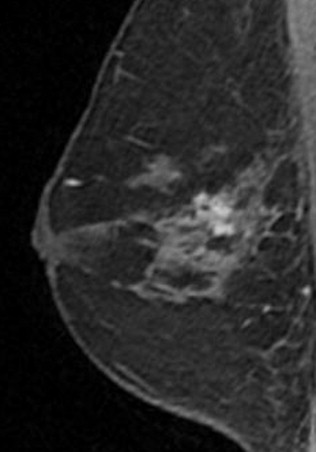
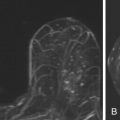
Clustered Ring Enhancement
Clustered ring enhancement ( Figure 5.7 ) has recently been described as an internal enhancement pattern associated with NME that appears to have a strong correlation with DCIS. Clustered ring enhancement was first described by Tozaki in 2006 and consists of conglomerate, small, round, hypointense structures surrounded by enhancement. Histologically, this pattern has been shown to correlate with crowded, DCIS-filled ducts, with the enhancement postulated to correspond to the periductal stroma and duct wall. The reported positive predictive value for malignancy with this finding ranges from 67% to 96%. In one study, 28 of 51 malignancies (55%) with clustered ring enhancement were DCIS. In 16 of 23 invasive cancers with clustered ring enhancement, associated DCIS made up 50% or more of the tumor. In another study, clustered ring enhancement was seen in 74% of malignancies presenting as segmental enhancement (positive predictive value, 83%). No clustered ring enhancement was found in six of seven tubular or lobular cancers in the study. However, seven of eight high-risk lesions (atypical ductal hyperplasia and multiple micropapillomas) also showed clustered ring enhancement. The authors postulate that this may be secondary to the lesion’s intraductal nature.
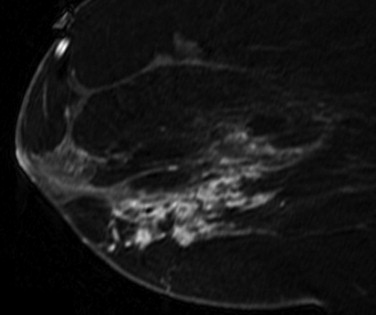
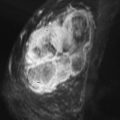
Kinetic Features
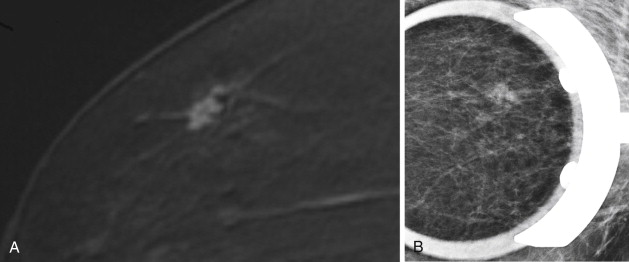
In terms of kinetic characteristics, DCIS frequently shows features similar to invasive cancer but may have a greater propensity toward slower enhancement and persistent and plateau curves than invasive cancer ( Figure 5.8 ).Van Goethem and coworkers compared 49 cases of pure DCIS with 213 cases of enhancing invasive carcinoma. DCIS showed washout kinetics slightly less frequently than invasive cancer: 53.8% for pure DCIS versus 65.3% for enhancing invasive carcinoma; 60.9% of DCIS cases reached peak enhancement after 3 minutes, whereas most invasive masses showed peak enhancement between 1 and 3 minutes. The only statistically significant kinetic parameter differentiating between DCIS and invasive cancer was signal intensity increase of more than 100%, which was seen in 76.9% of DCIS and 91.1% of invasive cancer. Other studies have demonstrated similar results: 50% to 78% of DCIS cases showed suspicious kinetics with rapid initial uptake of contrast and delayed phase washout- or plateau-curves. Another study showed a similar distribution of delayed phase curves (57.5% showing washout or plateau curves), but only 25% showed strong initial phase uptake. These results imply that a meaningful proportion of DCIS lesions will show kinetic features not typical of malignancy.