More than 2 million women in the United States have undergone breast implantation since the 1960s, either for cosmetic augmentation or breast reconstruction. During this time, both the silicone controversy and the known complications of breast augmentation have necessitated an accurate imaging modality to evaluate breast implants. Magnetic resonance imaging (MRI) has become the accepted standard for the evaluation of implant integrity. In this chapter, we will discuss the history of breast augmentation and the types of implants that can be encountered in daily practice. The advantages of MRI over both mammography and sonography in evaluating implant rupture will also be addressed.
History of Breast Implantation
The first breast augmentation procedure was performed in 1895 by Czerny. The breast was reconstructed with autologous fat implantation, after the excision of a large fibroadenoma. Throughout the remainder of the 1800s, a variety of materials were injected into the breast, including mineral oil, fat and Vaseline. In the early 1900s, paraffin injections were performed for breast reconstruction. However, this practice was discontinued by the early 1920s secondary to both local and lethal complications, including breast lumps, skin necrosis, lung emboli, and brain emboli. Other materials, such as glass balls and ivory, have been inserted into the breast for reconstruction.
Silicone was developed in the 1930s. The material was soon considered ideal for breast augmentation for two reasons. Silicone could be easily manufactured in a variety of sizes and shapes, and silicone was the first material to have a “normal” feel once inserted into the breast. The injection of liquid silicone into the breast was first performed in Japan, reportedly in the late 1940s. In the United States in the 1950s and 1960s, liquid silicone was directly injected into the breast parenchyma for augmentation. The main problem encountered by use of free silicone was the tendency of the silicone to migrate a far distance from the site of the injection. “Adulterated” silicones were then created to keep the silicone from migrating away from the injection site. These adulterated silicone substances contained fibrosing agents such as vegetable oil or fatty acids. The free injections of adulterated silicones resulted in a silicone-induced mastopathy in many women. The mastopathy included lymphadenopathy, granulomatous masses, fibrosis, skin retraction, nipple inversion, and infections. The practice of direct silicone injections was prohibited by the U.S. Food and Drug Administration (FDA) in the 1970s.
The first silicone gel-filled implant was inserted into the breast by Dr. Thomas Cronin at Baylor University in 1962. The creation of the silicone gel prosthesis revolutionized plastic surgery of the breast. The first silicone implants were produced commercially by Dow Corning Corp. starting in October 1963. The early silicone implants were made of a silicone polymer capsule and a liquid silicone gel. These early-generation implants were prone to rupture, predominantly as a result of the thinner shells and less-viscous silicone gel used at the time. Since the 1980s, silicone implants have contained a more viscous or adhesive gel, which is designed not to leak, even if the outer shell is breached.
The use of silicone breast implants has been a controversial and debated topic since the beginning of their use in the 1960s. Most of the controversy has centered on the suggested association of silicone implants with connective tissue disorders and malignant diseases of the breast. As a response to the concern over silicone breast implants and their association with systemic disease, the FDA imposed a moratorium on silicone gel implants in 1992.
In 1999, a formal report was published by the Institute of Medicine: “Safety of Silicone Breast Implants.” The report concluded that the local complications of silicone implant rupture were frequent. However, these complications were difficult to diagnose because of the large variety of implant types and styles available on the market. The report also came to two separate conclusions, assuring patients of the safety of silicone implants. First, the report asserted that there was no increase in either primary or recurrent breast cancer in women with silicone implants. Second, it asserted that there was no higher risk of malignancy, connective tissue disorders, or neurologic diseases in women with implants than in women without implants. In a slow response to this report, the FDA re-approved silicone gel implants in 2006, with some mild limitations. Silicone devices are permitted for all women undergoing breast reconstruction following breast cancer, trauma to the breast, or developmental disorders involving the chest wall. However, silicone implants are not available for women younger than age 22 years for purely cosmetic use.
The FDA also made recommendations to guide imaging practices. The FDA suggests a baseline breast MRI to evaluate for implant integrity 3 years after the placement of silicone implants and then every 2 years thereafter, to evaluate for rupture in asymptomatic women.
Implant Basics
A wide variety of implants are available to the American consumer, including silicone and saline implants and numerous varieties that contain a combination of both materials. To better evaluate for the complication of rupture, familiarity with the types of implants is necessary for the interpreting radiologist. The types of implants, the location of implants, and the known complications of implant rupture are discussed later. For a thorough review of breast implants, Middleton and McNamara created a comprehensive breast implant classification scheme, based on historical and MRI considerations.
A saline implant is constructed with an elastomer shell filled with saline. The implant can contain a variable amount of saline, which can be adjusted via a fill valve. Often, the valves used to adjust saline volume are mammographically visible and frequently palpable on physical examination ( Figure 11.1 ). A saline implant rupture is a clinical diagnosis, with rapid implant decompression when the elastomer shell develops a tear ( Figure 11.2 ). Hence there are few indications for MRI evaluation of a patient with saline implants. If the patient has a history of a prior silicone implant or free silicone injections, MRI may be useful to determine if any free silicone remains. If MRI is performed, it is important to note that the presence of fluid outside the shell is not specific for rupture in patients with saline implants. Normal migration of saline or reactive serous fluid can develop around the saline implant.


A variety of silicone implants can be encountered with MRI scans, including single-lumen, double-lumen, and reverse double-lumen implants. The standard single-lumen silicone implant has an outer silicone elastomer shell and contains homogeneous high signal intensity silicone on T2 images ( Figure 11.3 ). A typical double-lumen implant contains two elastomer shells, with silicone in the inner gel space and saline in the outer lumen. The amount of saline in the outer lumen can either be a fixed amount or variable, depending on the manufacturer. Double-lumen implants were created to reduce silicone gel bleeding and associated capsular contracture ( Figure 11.4 ).


A reverse double-lumen implant contains a variable amount of saline in the inner lumen and a fixed amount of silicone in the outer lumen. The reverse double lumen implant is frequently seen in the setting of breast reconstruction. The benefit of this implant is a more natural feel because the silicone component is located on the outside. In the Middleton and McNamara series, only 11% of the implants were of the standard double-lumen variety and fewer than 1% were reverse double-lumen implants.
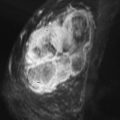
Because of the bicompartmental nature of dual-lumen implants, failure of the inner elastomer shell can have a unique outcome not visualized with single-lumen silicone implants. Failure of the inner shell leads to intermixing of the saline and silicone, a type of intracapsular rupture easily identified with MRI. Failure of the inner elastomer shell has been termed an internal rupture . The mixture of the silicone and saline contents has also been described as the salad oil sign on breast MRI because of the appearance of large globules of silicone intermixed with saline ( Figures 11.5 and 11.6 ).


Silicone implants can have a smooth or textured surface to the elastomer shell. The textured surface was developed to decrease the rate of capsular contracture. Some implants also have a coating of polyurethane (PTU) over the surface of the silicone envelope. This PTU layer serves a similar purpose as a textured implant, decreasing the rate of capsular contracture. Both the textured and PTU-covered implants commonly have a small to moderate amount of serous reactive fluid surrounding the implants. If pronounced, the reactive fluid surrounding a single-lumen device can mimic an intact double-lumen implant. The presence of this extracapsular fluid on MR imaging has been described as a picture frame appearance.
Additional, rarer types of implant devices are occasionally seen with implant-integrity breast MRI. These types of implants account for fewer than 1% of breast implants. A silicone gel/gel double-lumen implant has been commercially available since the 1980s. The inner lumen is usually overfilled with silicone gel and therefore holds a more spherical shape. The outer lumen is usually underfilled to achieve a more reasonable cosmetic outcome. Triple-lumen implants are also available, containing an overfilled silicone gel inner layer, an underfilled silicone gel middle layer, and an outer layer of saline ( Figure 11.7 ). Soft pectus implants are made of a solid silicone elastomer and are dark on all MRI sequences. These pectus implants were developed to cosmetically correct either an acquired or congenital absence of the pectoralis muscle. Finally, “stacked” implants have been used for the purpose of breast reconstruction. This technique utilizes more than one implant per breast.

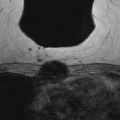
Breast implants are placed in either a subglandular or subpectoral location. The subglandular location places the implant between the patient’s fibroglandular breast tissue and the pectoralis major muscle. With both mammography and breast MRI, the pectoralis muscle is seen diving behind the implant when the implant is placed in a subglandular location ( Figure 11.8 ). The subpectoral location places the implant between the pectoralis major and minor muscles ( Figure 11.9 ). The choice of a subpectoral versus subglandular location greatly varies from patient to patient, and the decision is often based on the surgeon’s preference. The surgical insertion of a subpectoral implant is technically more difficult. However, a subpectoral implant allows for better visualization of native breast tissue on mammography, has a lower incidence of capsular contracture, and has been associated with reduced surgical scarring.


Implants can be placed by an inframammary, periareolar, or axillary approach. The inframammary approach provides the easiest surgical access but does result in a scar along the inframammary fold. The periareolar semicircular incision causes the least amount of scarring, but there is a risk of decreased nipple sensation. The axillary approach causes minimal scarring but is technically more difficult.
The risk of rupture of a silicone-containing implant is directly related to the age of the implant and placement of the implant behind the pectoralis muscle. The majority of ruptures have no known traumatic origin, and implant rupture increases in incidence with time. The exact incidence of breast implant rupture is unknown. Silicone implant ruptures have been linked to breast pain, paresthesias, asymmetric swelling, and breast contracture. In symptomatic women, with either breast pain or contracture, the incidence of rupture is 15% to 33%. In most cases, however, implant rupture goes unnoticed by the patient, with no changes to the shape or feeling of the breast. The frequency of rupture in asymptomatic women has been reported up to 6%.
Magnetic Resonance Imaging of the Implanted Breast
Breast MRI is the modality of choice for the evaluation of silicone implant rupture. MRI conveys the highest sensitivity and specificity for silicone implant rupture. In 2005, Holmich and coworkers calculated an accuracy of 92%, a sensitivity of 89%, and a specificity of 97% for implant rupture detection in a population of 118 implants, after comparing with findings at explantation. Silicone has a unique magnetic resonance frequency that allows for silicone-selective sequences to be performed. It is this selective frequency that accounts for the high accuracy and specificity seen with implant-integrity breast MRI. According to Monticciolo and colleagues, the creation of silicone-selective pulse sequences has contributed to the use of MR for detection of implant rupture and subsequent silicone leakage.
Breast MRI also has additional advantages over both mammography and sonography, including the ability to image with multiplanar capability and the lack of ionizing radiation conveyed to the patient. In the setting of an extracapsular rupture, MRI gives a detailed account of silicone migration and the relationship to vital structures, including axillary lymph nodes and the brachial plexus. However, breast MRI has several limitations. MRI is an expensive imaging modality, with a cost several times greater than either mammography or ultrasound. Also, the use of MRI is not available for patients with pacemakers, certain aneurysm clips, foreign bodies in sensitive locations, and for patients limited by claustrophobia or body habitus.
Adequate MRI of the breast requires both specific sequences and dedicated breast imaging equipment to evaluate for implant rupture. A 1.5 Tesla (T) magnet strength or greater is preferred, which allows for detection of more subtle signs of intracapsular or extracapsular rupture. Also, the use of a standard body coil does not provide adequate resolution in breast imaging. A dedicated magnetic resonance breast coil is needed for implant-integrity breast imaging. The use of a dedicated breast surface coil improves the accuracy of breast MRI in diagnosing implant rupture. For diagnosing extracapsular rupture, T2-weighted images with both chemical fat suppression and water suppression should be obtained. This sequence allows for the greatest contrast difference between silicone and the surrounding breast tissue. Extracapsular rupture is not well depicted on fast spin echo T1-weighted images.
MRI of the breast can also be used as a problem-solving tool in patients who plan to undergo revision implant surgery. Often, patients who need a revision of their silicone implants have no specific information about their current implant size, making surgical planning difficult. Clinical estimates of implant volumes can be widely inaccurate, especially if the implants have ruptured or are severely contracted. A calculation of silicone breast implant volume can be performed using breast MRI and a commercially available computer-aided detection (CAD) system with sufficiently accurate results. Calculating accurate implant volume may have a clinical benefit in planning implant revision surgery.
MRI of the breast is also considered the modality of choice for detecting breast cancer in patients who have undergone free silicone injections. In the 1960s and 1970s, free silicone injections were less costly than implants and therefore appealed to women who were unaware of the risks and complications. The injected free silicone is randomly distributed in the breast and limits both the mammographic and sonographic evaluation for breast cancer ( Figure 11.10 ). In the setting of silicone-induced mastopathy, fibrous silicone breast masses are difficult to distinguish from a breast carcinoma. Therefore a combined breast MRI technique using both contrast-enhanced sequences and the T2-weighted sequence with fat and water suppression can be helpful in identifying malignancy in patients with free silicone injections ( Figure 11.11 ).