Fig. 1
Typical pathological changes in muscular tissue of the thigh shown in standard proton (1H) MRI. a edema like changes, b lipoamatous degeneration, c atrophy, d hypertrophy (images courtesy of Prof. Dr. M.-A. Weber, Heidelberg)
This chapter will describe the development of WB MRI, discuss advantages and disadvantages of this modality, give examples for dedicated neuromuscular WB MRI protocols and show potential clinical applications of WB MRI to evaluate skeletal muscle disease.
3 Development of WB MRI
Between 1997 and 2001, the first studies about WB MRI were published (Barkhausen et al. 2001; Daldrup-Link et al. 2001; Eustace et al. 1997, 1999; Horvath et al. 1999; Johnson et al. 1997; Steinborn et al. 1999). However, these early protocols were not introduced into routine clinical care because imaging quality was reduced in comparison to dedicated examinations and examination times were too long. Furthermore, the coils had to be repeatedly rearranged and the patient had to be repositioned for several times during one examination.
Important improvements were the introduction of a rolling table platform mounted on top of the MRI table (Lauenstein et al. 2002; Zenge et al. 2005) and the implementation of parallel imaging techniques (Larkman and Nunes 2007). Parallel imaging has the advantage of a shorter acquisition time for the same spatial resolution or a higher spatial resolution within a given time in comparison to conventional techniques (Griswold et al. 2002; Sodickson and Manning 1997).
Whole-body imaging protocols employing these new MR techniques were mainly described for whole-body cancer screening and staging and for whole-body cardiovascular examinations (Steinborn et al. 1999; Schmidt et al. 2006, 2007; Kramer et al. 2005; Weckbach and Schoenberg 2009). Possible applications for musculoskeletal WB MRI beyond the evaluation of bone marrow and metastases are inflammatory arthritis and multifocal rheumatoid diseases (Weckbach 2009, 2012), or lipodystrophies (Hegele et al. 2007) (Fig. 2).


Fig. 2
Whole-body MR image of Type 2 familial partial lipodystrophy (FPLD, type Dunnigan). The coronal T1-weighted sequences (1.5T) composed of the whole-body showed rarefication of subcutaneous fat tissue of the upper and lower extremities and more fat tissue within the abdomen when compared to a control subject (images courtesy of Prof. Dr. M.-A. Weber, Heidelberg)
In comparison to oncology and cardiovascular applications, there are still only few publications about comprehensive WB MRI protocols for evaluation of the skeletal muscles (Schramm et al. 2008; Kesper et al. 2009; Kornblum et al. 2006; Quijano-Roy et al. 2012), even though this is a promising field for WB MRI in our opinion.
4 Conventional Muscle Imaging with MRI
Imaging in muscle disease has been and still is in many cases focused on the evaluation of particular muscle groups, especially the pelvic girdle and the thighs. Many myopathies predominantly affect the pelvic girdle and the thighs (Fischer et al. 2005). As many patients with muscular disease are pediatric, short protocols sometimes only containing axial T1w sequences have been proposed (Mercuri et al. 2002).
5 Why WB MRI for the Evaluation of Muscle Diseases?
As many myopathies involve various muscle groups in different body areas, the full extent of the disease may not be detected with dedicated muscle MRI. In one of our WB MRI studies including 18 patients with different degenerative and inflammatory myopathies we found an involvement of the erector spinae muscles in 61.1 % (Schramm et al. 2008). Affection of the erector spinae muscles seems also to be common in patients with myotonic dystrophy type 1 and 2 as described by Kornblum et al. in their WB MRI study (Kornblum et al. 2006). It has been shown in WB MRI studies that involvement of other muscle groups like in the shoulder girdle or the upper arms seem to be a common finding in many myopathies, too (Schramm et al. 2008; Shelly et al. 2010).
Muscle MRI and especially WB MRI can detect subclinical involvement of muscle groups, this may be helpful for early diagnosis and differential diagnosis (Sookhoo et al. 2007). In comparison to clinical examination and dedicated muscle MRI, WB MRI could be of additional diagnostic value by depicting the extent of disease and identifying possible patterns of involvement for distinct myopathies (Olive et al. 2007; Ozsarlak et al. 2004).
The fundamentals of the diagnosis of a myopathy remain muscle biopsy with histological examination and genetic analysis. WB MRI has the potential to characterize distinct subtypes of myopathies and enable a more focused genetic testing (Fischer et al. 2005; Carlier et al. 2011). Muscle biopsy has a high rate of false-negative results (10–25 %). WB MRI can decrease this high rate by providing a WB overview of possible biopsy sites (Sookhoo et al. 2007). WB MRI a suitable modality for follow-up examinations (e.g., progress, prognosis, therapy monitoring) as it is noninvasive in contrast to electromyography or biopsy.
6 MR Sequences for Muscle MRI
T1-weighted images provide a high signal-to-noise ratio and excellent anatomic detail, while also allowing characterization of hemorrhagic lesions (e.g., hematoma, hemorrhagic neoplasm) or abnormal fat deposition (e.g., muscle atrophy, lipoma) (Napier et al. 2006). Any protocol designed to highlight muscle disease must take advantage of T2 lengthening; most disease processes cause an increase in the water content of muscle resulting in prolongation of the T2 relaxation time and hence signal hyperintensity (Rybak and Torriani 2003). Fat-suppressed T2-weighted and short tau inversion recovery (STIR) fast spin echo sequences are more sensitive to the presence of muscle edema and hemorrhage than longer time to echo (TE) sequences that are not fat suppressed (May et al. 2000) (Fig. 3). Intravenous contrast material is not generally necessary in the evaluation of muscle disease as areas affected by inflammation are well demonstrated on fat-suppressed T2-weighted and STIR imaging. Occasionally, fat-suppressed T1-weighted imaging post gadolinium administration can be helpful in difficult cases (e.g., when evaluating for a cystic versus a solid mass) (Schmidt et al. 2007). In addition to producing signal abnormality, conditions affecting the musculature commonly cause changes in muscle size and shape and this is best appreciated by comparison with the contralateral, unaffected side.
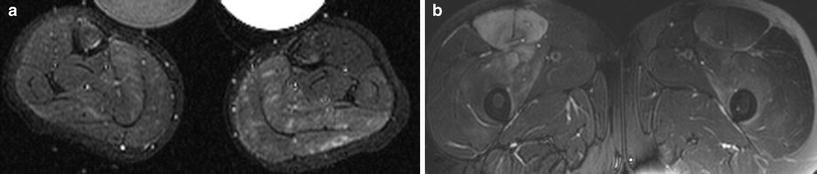
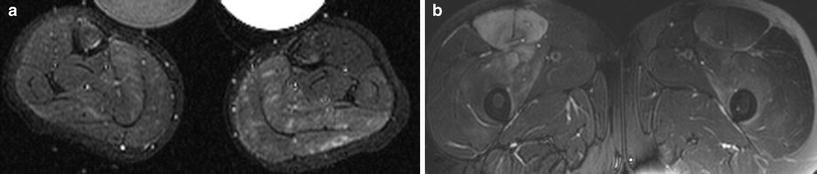
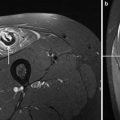
Fig. 3
a Axial STIR images of both lower legs in a 7-year-old boy with Duchene muscle dystrophy and edema like changes most pronounced in the left triceps surae muscle. b Axial fat-saturated T2-weighted MR image of both thighs in a 25-year-old rugby player with rhabdomyolysis most pronounced within the right quadriceps muscle after intensive resistance training that focuses on strengthening the quadriceps muscles. The patient presented with acute muscle tenderness (images courtesy of Prof. Dr. M.-A. Weber, Heidelberg)
7 Normal Skeletal Muscle MR Appearances
Muscle fibers form the basic functional unit of skeletal muscle. Muscle fibers are grouped into fascicles, and the fascicles are grouped into muscles. At MR imaging, skeletal muscle has an intermediate to long T1 and short T2 relaxation time and so it has signal intensity higher than water and lower than fat on T1-weighted imaging and much lower than water and fat on T2-weighted imaging (Reimers et al. 1994; Fleckenstein and Reimers 1996). Normal muscle fascicles are separated from one another by fat-containing septa, thus, normal skeletal muscle has a feathery or marbled appearance on non-fat suppressed images (Costa et al. 2012).
8 Comprehensive Neuromuscular WB MRI Protocol
The statement “one fits all” is not true for WB MRI protocols. A WB protocol should be tailored to a specific clinical question. For example, WB MRI protocols designed to evaluate cardiovascular or oncological diseases differ from each other considerably.
In this chapter, we provide an example of a comprehensive neuromuscular WB MRI protocol as it is used at the Ludwig-Maximilians-University Hospital in Munich/Germany (Schramm et al. 2008).
WB MRI is performed on a 1.5 T whole-body scanner (Magnetom Avanto, Siemens Medical Solutions, Erlangen, Germany). Multiple phased-array surface coils with up to 76 receiver coil elements and 32 receiver channels for simultaneous signal reception are used (Fig. 4). Parallel imaging techniques are utilized, and imaging is possible without patient repositioning by automated table motion (Schmidt et al. 2007). The maximum range of volume to be examined in the z-axis is 205 cm. Patients are examined from head to toe in supine position with the arms beside the body. The protocol contains T1 turbo spin echo (TSE) sequences for delineation of anatomy and to detect fatty infiltration and atrophy of skeletal muscles as well as STIR sequences for sensitive detection of muscle edema. The proposed WB protocol includes coronal T1w and STIR sequences at five body levels (head/neck, thorax/shoulders, abdomen, pelvis, thighs, lower legs) and axial T1w sequences of the upper arms, the thighs, and the lower legs. Half-Fourier acquired single-shot turbo-spin-echo (HASTE) sequences of the thorax and abdomen in axial and coronal orientation to detect organ pathologies are optional. No contrast material is administered. Sagittal sequences of the spine are dispensable for muscular WB MRI protocols. Further details concerning the protocol are provided in Table 1. Relevant pathology can be demonstrated to clinicians with composed T1w and STIR whole-body images after postprocessing. Total acquisition time for this comprehensive WB MRI protocol was 41:26 min (including 1:35 min localization time). Patient preparation and coil positioning requires approximately 5–7 min.


Fig. 4
For a whole-body MRI examination the entire body of the patient is covered by several coils (Magnetom Verio, Siemens Medical Solutions, Germany) (image courtesy of Prof. Dr. M.-A. Weber, Heidelberg)
Table 1
Example of a neuromuscular whole-body 1.5 Tesla MRI protocol (adapted from reference 23)
Sequence | TA (min) | Slice thickness (mm) | Slices | PAT | TR (ms) | TE (ms) | Voxel size (mm) | FOV (mm) | Matrix |
|---|---|---|---|---|---|---|---|---|---|
T2 stir cor head/neck | 01:55 | 5 | 38 | 3 | 6380 | 92 | 1.8 × 1.3 × 5 | 480 | 269 × 384 |
T1 cor head/neck | 03:41 | 5 | 38 | 3 | 797 | 12 | 1.8 × 1.1 × 5 | 480 | 358 × 448 |
T2 stir cor Th + Abd mbh | 02:02 | 5 | 42 | 3 | 3380 | 101 | 1.8 × 1.3 × 5 | 480 | 269 × 384 |
Haste tra mbh Tha | 00:44 | 6 | 40 | 2 | 1100 | 45 | 1.2 × 1.2 × 6 | 380 | 240 × 320 |
Haste tra mbh Abda | 00:44 | 6 | 40 | 2 | 1100 | 45 | 1.2 × 1.2 × 6 | 380 | 240 × 320 |
T2 ha cor mbh p3 Th + Abda | 00:38 | 5 | 42 | 3 | 900 | 73 | 1.9 × 1.5 × 5.0 | 480 | 256 × 320 |
T1 cor Th + Abd + mbh | 01:38 | 5 | 40 | 3 | 400 | 8.2 | 1.3 × 1.1 × 5 | 480 | 358 × 448 |
T1 tse cor upper arm | 03:58 | 4 | 24 | 3 | 588 | 12 | 0.8 × .8 × 4.0 | 360 | 448 × 448 |
T1 tse tra upper arm | 02:08 | 5 | 32 | 2 | 600 | 18 | 0.8 × 0.7 × 5 | 280 | 281 × 384 |
T2 stir cor pelvis | 02:02 | 5 | 38 | 3 | 6090 | 84 | 1.8 × 1.3 × 5 | 480 | 269 × 384 |
T1 cor pelvis | 03:41 | 5 | 38 | 3 | 797 | 12 | 1.3 × 1.1 × 5 | 480 | 358 × 448 |
T2 stir cor thigh | 02:02 | 5 | 38 | 3 | 6090 | 84 | 1.8 × 1.3 × 5 | 480 | 260 × 384 |
T1 cor thigh | 03:41 | 5 | 38 | 3 | 797 | 12 | 1.3 × 1.1 × 5 | 480 | 358 × 448 |
T1 tse tra thigh | 02:51 | 6 | 34 | 2 | 637 | 20 | 1.1 × 0.9 × 6 | 400 | 240 × 448 |
T2 stir cor lower leg | 02:45 | 5 | 38 | 2 | 5900 | 84 | 1.8 × 1.3 × 5 | 480 | 269 × 384 |
T1 cor lower leg | 03:29 | 5 | 38 | 2 | 767 | 11 | 1.3 × 1.1 × 5 | 480 | 358 × 448 |
T1 tse tra lower leg | 01:52 | 6 | 34 | 2 | 637 | 20 | 1.1 × 0.9 × 6 | 400 | 230 × 448 |
To save time the following variant of a neuromuscular WB MRI protocol is also possible (as performed on a 3T scanner (Magnetom Verio, Siemens Medical Solutions, Erlangen, Germany) in the University Hospital of Heidelberg/Germany): Routinely, the patients are examined from head to toe with coronal STIR sequences and T1 TSE sequences. Only regions that appear pathological on the coronal slices are examined with additional STIR and T1 TSE sequences in axial orientation. This approach requests a radiologist who quickly reviews the coronal sequences during the examination and tells the technologists which optional axial sequences are needed in every single case.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree