(1)
Radiology – Neuroradiology Section, S. Paolo Hospital, Bari, Italy
Degenerative spinal pathology is one of the most common causes of pain in society. Degenerative disease of the spinal column is highly prevalent in the general population, and its incidence increases with age.
Pain is the main symptom among those individuals most commonly associated with this pathologic condition; others are neurologic disorders (i.e. sensory, motor, neurovegetative dysfunctions).
Different factors, both individually and concomitantly, can result in degenerative processes of the spine, such as mechanical (e.g. postural anomalies, heavy weight-bearing, sports), anatomic (e.g. malformations, dysplasias) and metabolic factors (e.g. diabetes).
The lumbar spine is most frequently involved; up to 70–80 % of people have low back pain during their lifetime [1].
It is understood that only a certain number of patients with back pain will be found to have a disc herniation, spinal stenosis or well-known causes of pain; in the other cases it may be difficult to discover the source of pain. It is equally well understood that the syndrome may arise from the posterior elements/perispinal tissues of the lumbar spine, which are richly innervated [2–4].
The diagnostic techniques of computed tomography (CT) and magnetic resonance imaging (MRI) have made an important contribution to the study of degenerative diseases of the spinal column. In particular, MRI provides a very sensitive method for examining degenerative phenomena of the spine, even in the initial stages of the disease lifetime [1–3, 5–9].
However, traditional MRI of patients with low back pain does not always enable clear identification of pain aetiology. In our experience, T2-weighted sequences with fat saturation and, when indicated, T1-weighted sequences with fat saturation after intravenous administration of contrast medium provide a more sensitive picture of the degenerative changes of the spinal column and occasionally disclose pathologic conditions unsuspected during a “standard” MRI examination [1–3, 5].
All the patients in this series were examined with a 1.5 T MR system (Siemens Symphony TIM) by using the following basic study protocol:
TSE/SE T1-weighted images on the sagittal plane (and axial plane on the lumbosacral spine)
TSE T2-weighted images with fat saturation on the sagittal plane
TSE T2-weighted images with fat saturation on the axial plane (eventually to be conducted on the pathologic area, for a better spatial characterization of the oedematous lesion)
GE T2*-weighted images on the axial plane on the cervical spine
TSE/SE T1-weighted images with FS on the sagittal and axial planes following administration of contrast medium (eventually to be conducted to identify the active-inflammatory stage of the disease)
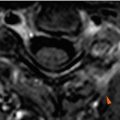
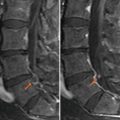
An efficient spinal imaging protocol must comprise T2-weighted sequences with fat suppression, in particular with fat saturation technique or STIR sequences, in order to clearly visualize hyperintensity corresponding to oedematous lesions, otherwise not easily identifiable with “standard” imaging sequences without fat suppression (Fig. 2.1).


Fig. 2.1
(a, b) “Standard” sagittal TSE T2-weighted image without fat saturation (a) and sagittal TSE T2-weighted image with fat saturation (b). Hyperintense areas in fat suppressed T2-weighted image in the L3-L4-L5 vertebral bodies, indicating oedema of the bone marrow (b, asterisks). Note that the sequence without fat saturation does not detect the same lesions in the same way (a). Note also hyperintense lesions of the interspinous ligaments in T2-weighted images with fat saturation (b, arrowheads). The same lesions cannot be defined in T2-weighted image without fat saturation (a)
In the same way, administration of contrast medium must be followed by T1 sequences with fat saturation, in order to clearly identify the active inflammation.
The indication for contrast medium administration was based on evidence of osteo-articular or muscular-ligamentous oedema in T2-weighted images with fat saturation. In some selected cases, we administered contrast medium although the basic scan failed to disclose oedematous lesions on T2-weighted images (e.g. in cases of clinical-radiological discrepancy).
In this series we administered intravenous paramagnetic contrast medium (Dotarem – Guerbet – 0.5 mmol/ml, 0.2 ml/kg dose).
The fat saturation technique consists in a spectral saturation of the fat, by adding a selective radiofrequency (RF) impulse on the fat frequency. To determine the fat frequency, the machine checks for the presence of approximately a 130-Hz peak, as compared with the resonance frequency of water, at which point it emits the RF impulse. The effect of the impulse is to excite the fat over 180°, whereby it will be unable to return the signal. Such a technique enables the saturation of the fat signal on almost all of the available sequences, from spin-echo to gradient-echo, using any type of MRI sequence (T1, T2, T2*).
We have to remember that fat signal can be suppressed also by using STIR sequences, but, in our experience, this technique has a long acquisition time, whereas FS technique substantially does not change the relative acquisition time.
Today, the correct diagnosis is important in effecting improved aeration outcomes: it will be reflected in an elevated benefit/cost ratio with regard to MRI and will enable more accurate therapy of the specific source of painful symptoms (e.g. microinvasive percutaneous treatment).
In this text-atlas we deal with the following degenerative spinal changes, with particular attention on corresponding inflammatory aspects: disc degeneration, disc herniation, facet joint pathology (e.g. osteoarthritis, joint effusion, synovitis, and synovial cysts), spondylolysis, canal stenosis, spinal/perispinal ligamentous degenerative-inflammatory changes and perispinal muscular changes. Moreover, we show some unusual clinical cases.
2.1 Disc Degeneration
Discs are commonly the primary element of the spine that manifest degenerative alterations. As with every occurrence of arthrosis, such degenerative phenomena are largely due to genetics, long-term heavy weight-bearing and other complex factors.
From the morphological standpoint, disc degeneration results in loss of height, radial bulging, fissuring of the annulus fibrosus and disc herniation; moreover, degenerative disc alterations are typically accompanied by morpho-structural changes of the adjacent vertebral bodies (e.g. spondylosis and osteochondrosis).
These degenerative phenomena, and associated inflammatory component, are clinically important as they are associated with nonirradiating (discogenic) pain, caused by stimulation of the nerve terminals innervating the disc-vertebral body complex [4, 5] (Fig. 2.2).
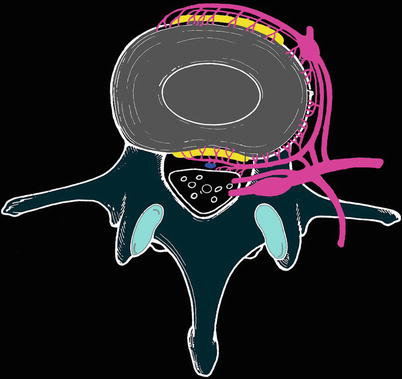
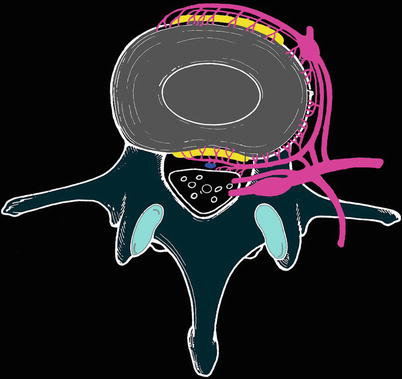
Fig. 2.2
Schematic figure depicting the rich innervation of the disc-vertebral body complex (modified from Jinkins)
MRI clearly depicts such degenerative phenomena to a superior degree than other imaging modalities. Among other findings, the degenerated disc demonstrates a reduction in signal intensity on T2-weighted images (principally due to dehydration processes and variations in proteoglycan composition) and a decrease in height; in the more advanced stages of degeneration, the disc collapses and may undergo cystic changes, gaseous degeneration and calcification.
Discal degenerative processes are usually accompanied by bone marrow changes in the supravertebral and subjacent vertebral bodies, which are currently classified as the following [10]:
Type I – fibrovascular replacement of the bone marrow
Type II – proliferation of the fatty marrow
Type III – osteosclerosis
In our experience, type I alterations are more evident on T2-weighted images with fat saturation, since the suppression of the fat signal enhances the fibrovascular transforming phenomena and underlying bone marrow oedema. In addition, the use of T1-weighted sequences with fat saturation after administration of contrast medium frequently shows enhancement of this same bone marrow in parallel with the bone oedema (this event is normally marked in “traditional” T1-weighted sequences after contrast medium administration).
2.2 Disc Herniation
Disc herniation is one of the most common diseases, with very high social costs; it is the first cause for absenteeism from work and the main cause for surgery on the spine [11].
Herniated disc arises from the rupture of the annulus fibrosus and subsequent leakage of nucleus pulposus beyond the margins of the same annulus.
The aetiology of disc herniation includes degenerative disc disease, repeated trauma and genetic factors [9].
Symptoms of disc herniation originate from compression of nerve roots and/or spinal cord, depending on the level and position of the hernia.
In particular, radicular pain is caused by mechanical compression, inflammatory effects, vascular and biochemical modifications caused by the contact between the disc and nerve root [11].
Patients affected by herniated disc many times begin a diagnostic and therapeutic route involving neurosurgeons, orthopaedics, neurologists and physiatrists.
Diagnosis involves the collection of anamnestic data, physical examination, diagnostic imaging (MRI, CT) and electromyography.
MRI represents the gold standard diagnostic technique, exquisitely delineating disc herniation and the relationship to adjacent soft tissues.
It is important to describe the precise location of the herniated disc. The relationship of the disc material to surrounding structures should also be mentioned in describing a disc herniation.
The hallmark of a herniated disc is a focal contour abnormality along the disc margin, with a soft tissue mass displacing the epidural fat, thecal sac or nerve root. The herniated disc is usually contiguous with the corresponding disc by a narrow waist, which is the site of a radial tear in the annulus [9]. In some cases, a free disc fragment can develop, that is, no longer in continuity with the parent disc and can migrate inferior or superior to the parent disc level.
Unusual MR findings include atypical signal intensity or uncommon location. Some herniated discs present different signal intensity with respect to the disc parent, showing high signal intensity on T1- or T2-weighted images.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree