(1)
Radiology – Neuroradiology Section, S. Paolo Hospital, Bari, Italy
MRI is considered a fundamental technique in the diagnosis of spondyloarthritis (SpA) and in particular constitutes the gold standard technique to visualize early changes of the disease [1–10]. However, MRI findings of spondyloarthritis are typical but not specific, and similar changes may be seen in degenerative or other spinal disorders as well [1–3]. It is therefore of particular importance for radiologists and neuroradiologists to know MRI findings of these inflammatory lesions. Moreover, an efficient spinal imaging protocol is needed to correctly interpret MRI findings.
Typical lesions in spondyloarthritis comprise:
Spondylitis (Romanus lesion)
Discitis
Spondylodiscitis (Andersson lesion)
Osteoarthritis of the facet joints, costovertebral, and costotransverse joints
Osteoarthritis of the sacroiliac joints (sacroiliitis)
Enthesitis
It is helpful to know that inflammatory spinal lesions rarely occur in isolation but are frequently associated among them and in particular with sacroiliitis.
2.1 Vertebral Bodies
The earliest changes of spondylitis were described by Romanus and Yden on conventional radiographs [11]. These changes consist of blurring and erosions involving the anterior and posterior edges of the vertebral endplates and are also known as Romanus lesions. Later, sclerosis occurs in these areas, which is referred to as shiny corners.
MRI allows for the detection of these lesions at the beginning of their course. The early changes of the vertebral bodies are constituted by edema – osteitis in correspondence of the subchondral bone marrow. These changes are depicted on MRI as reduced signal on T1-weighted images and increased signal on T2-weighted/STIR images.
When these changes are localized to the anterior vertebral edges, the condition is called anterior spondylitis; when the changes involve only the posterior vertebral edges, we speak about posterior spondylitis; the combined form is named as marginal spondylitis.
In the further course of the disease, the epiphyseal rings may become hyperintense on T1-weighted images. Such hyperintensity indicates a circumscribed area of postinflammatory fatty degeneration of the bone marrow. This is the stage at which the changes first appear on conventional radiographs as shiny corners [4, 5].
Similar to conventional radiography, MRI depicts syndesmophytes as bone bridges of the anterior vertebral edges, which may be of lower or higher signal intensity on T2-weighted images depending on the floridity of the disease [4].
2.2 Intervertebral Discs
Inflammatory lesions of the intervertebral disc or discovertebral complex are known as discitis or spondylodiscitis, i.e., Andersson lesion, from the author who first described them [12].
Active spondylodiscitic lesions are characterized by hyperintense discovertebral changes on T2-weighted images and hypointense changes on T1-weighted images, indicating an edematous pattern of disc and/or subchondral bone marrow of adjacent vertebral bodies. Contrast enhancement of the same lesions is the indicator of inflammatory activity (i.e., osteitis and discitis).
In the further course of the disease, typical findings are constituted by erosions, fatty degeneration of the subchondral bone marrow, sclerosis, and transdiscal ankylosis.
As in anterior spondylitis (Romanus lesion), MRI is superior to conventional radiography in detecting Andersson lesions, since the edematous changes in early disease are not radiographically visualized [4, 5]. Radiography may show erosions of the vertebral endplates in the late course of the disease.
In literature, it is also described as a noninflammatory type of Andersson lesion, corresponding to an insufficiency fracture of the ankylosed spine, which may occur at the level of a disc (transdiscal) or a vertebral body (transvertebral) [13]. Such fractures may occur spontaneously or after minor trauma, frequently in association with osteoporosis.
2.3 Facet Joints, Costovertebral Joints, and Costotransverse Joints
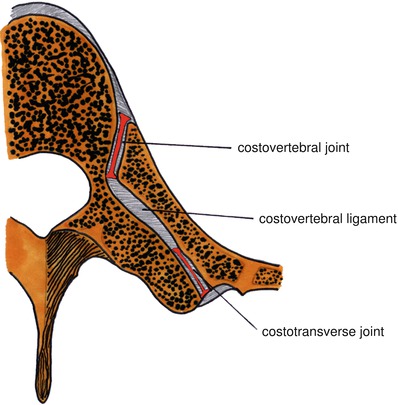
Facet joints (or zygapophyseal joints), costovertebral joints, and costotransverse joints (Fig. 2.1) represent another target for spondyloarthritis. They are all synovial joints.
MRI findings of arthritis involving the abovementioned joints are similar, including joint effusion, synovitis, erosions of the articular surfaces, and bone marrow edema. In the further course of the disease, affected joints may undergo ankylosis.
MRI clearly depicts these lesions, but it is necessary to examine carefully the sagittal images and obtain additional images on the axial plane.