The breast undergoes significant anatomic and histologic changes after intervention. Posttreatment imaging findings have been thoroughly described for mammography and breast ultrasound, but only isolated descriptions of postsurgical breast changes seen on dynamic contrast enhanced (DCE) breast magnetic resonance imaging (MRI) are found in the literature. New or recurrent cancer can be difficult to detect in the postsurgical breast by physical examination, breast ultrasound, and mammography. DCE breast MRI has emerged as an important adjunct study in the evaluation of the breast in postsurgical patients. Therefore it is critical for radiologists to understand the common surgical procedures performed on the breast and to be able to recognize their expected appearance on DCE breast MRI.
Understanding which findings are usual in the postsurgical and postradiation setting is of utmost importance in distinguishing between suspicious findings and expected changes after intervention. In addition to high risk screening and evaluation of extent of disease, the American College of Radiology practice guidelines included additional evaluation of clinical or imaging findings. Many of the patients referred to DCE breast MRI have had previous breast interventions. Although DCE breast MRI postsurgical findings can have similar morphologic appearance to those seen with mammography and ultrasound, there are also postprocedural changes specific to breast MRI.
Drawing on our experience as well as a thorough literature review, we wrote this chapter to catalog the most common changes attributable to prior breast surgical intervention, including image-guided biopsy, lumpectomy, radiation, mastectomy, and reconstructive and cosmetic surgery as well as other regional surgical changes.
Our Experience
After obtaining Institutional Review Board approval, we reviewed 719 breast MRIs performed between July 1, 2008, and June 30, 2009. The cohort of patient underwent breast MRI at the University of California San Diego department of radiology, an academic center with a breast MRI volume of more than 700 patients annually. Of the 719 patients imaged, 881 breasts on 590 patients (82%) had undergone earlier surgical or image-guided procedures. We identified patients who had undergone prior core biopsy, excisional biopsy, lumpectomy, mastectomy, breast reconstruction, breast reduction, breast implants, and nodal dissection. Using these data, we identified the most common postoperative changes seen on DCE breast MRI. Breast MRI changes observed included susceptibility artifacts, skin thickening, architectural distortion, implant-related changes, postoperative fluid collection, skin enhancement, skin retraction, scar progression, edema, fat necrosis, nipple retraction, hematoma, hemosiderin deposition, and chest wall changes ( Table 10.1 ).
| Finding | Total | Percent |
|---|---|---|
| Susceptibility artifact | 321 | 36.44% |
| Skin thickening | 70 | 7.95% |
| Architectural distortion | 61 | 6.92% |
| Seroma | 61 | 6.92% |
| Implants | 39 | 4.43% |
| Edema | 13 | 1.48% |
| Chest wall changes | 12 | 1.36% |
| Fat necrosis | 12 | 1.36% |
| Hematoma | 11 | 1.25% |
| Skin retraction | 9 | 1.02% |
| Nipple retraction | 8 | 0.91% |
| Hemosiderin | 4 | 0.45% |
| Skin enhancement | 3 | 0.34% |
| Scar progression | 2 | 0.23% |
| “Benign postprocedural” | 405 | 45.97% |
Image-Guided Interventions
The paradigm of breast cancer diagnosis has changed from radical surgeries to minimally invasive procedures. In the United States, about 1.6 million biopsies of breast tissue are performed every year; of these 75% will be benign. Minimally invasive procedures for tissue diagnosis are performed using devices including spring-loaded and vacuum-assisted devices of varying gauges. Stereotactic, ultrasound, and MRI-guided large-core (>14-gauge) biopsies have reduced the number of surgical biopsies and are indicated for histologic tissue diagnosis of palpable findings and/or imaging abnormalities. Most image-guided core biopsies are performed parallel to the chest wall, to prevent intrathoracic injury. A tissue marker should be left in place to document the location of the procedure.
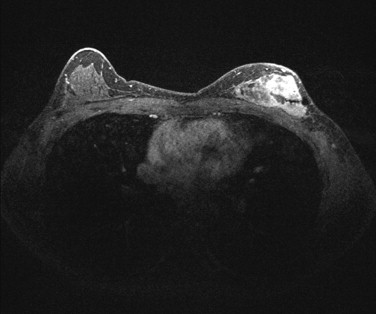
Although minimally invasive, these procedures disrupt the breast tissue, resulting in imaging findings easily identified on breast MRI. Depending on how recently the procedure was performed, the biopsy tract may be visualized by MRI. Figure 10.1 demonstrates a biopsy tract adjacent to an area of nonmasslike enhancement, diagnosed as invasive ductal carcinoma.
Tissue Markers
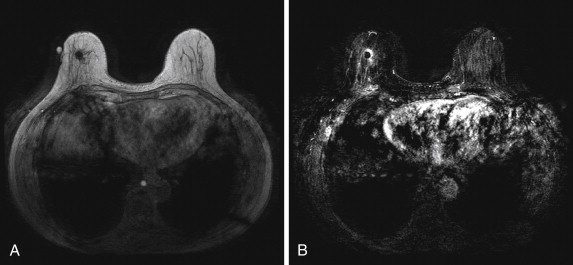
As mentioned, a tissue marker is routinely placed after core biopsy. Susceptibility artifacts of varying degrees may be noted and are typically more pronounced at higher field strengths (3 Tesla [T] vs. 1.5 T) and on T1-weighted sequences. Depending on the marker composition, identifying the marker may be challenging. Tissue markers are often best identified on the non–fat-saturated T1-weighted sequence, as seen in Figure 10.2 . Magnetic susceptibility is discussed further under the postsurgical findings of hemosiderin and metal.
Seroma/Hematoma
Seromas or hematomas are less common and usually less prominent by minimally invasive image-guided intervention than by surgical intervention. However, even large hematomas can be caused by image-guided interventions, as seen in Figure 10.3 . In this case, a delayed hematoma developed after stereotactic biopsy in a patient who was feeling well enough to exercise after the biopsy procedure. The stereotactic biopsy was positive for minimal ductal carcinoma in situ (DCIS). The hematoma, which had not been present immediately after stereotactic biopsy, was identified at the time of preoperative MRI to assess the extent of disease. Because seroma/hematoma findings are identical in both image-guided and surgical procedures, they are discussed further in the postlumpectomy findings in the next section.
Surgical Interventions
Lumpectomy
Lumpectomy is the most common form of breast cancer surgery and consists of removal of the tumor and immediate surrounding tissue. Randomized clinical trials have shown that breast conservation surgery with lumpectomy plus radiation therapy will yield the same disease-free and overall survival rates as mastectomy. However, after lumpectomy only, positive margins are present in the breast in 32% to 63% of patients and MRI is the primary imaging modality to evaluate for residual or recurrent tumor in the postoperative breast. Although it is not always possible to differentiate postsurgical changes from recurrent or residual tumor on MRI, it is crucial for the interpreting physician to be familiar with the imaging findings related to surgery, to distinguish them from tumor, and refrain from unnecessary intervention.
As with mammography, postsurgical changes identified at MRI are expected. These include enhancement of the postoperative seroma rim, architectural distortion, skin thickening, and retraction. Most of these changes diminish over time. In the case of positive surgical margins following breast conserving surgery, MRI can be beneficial in identifying clumped or masslike enhancement. This information can aid the surgeon in directing the region of reexcision.
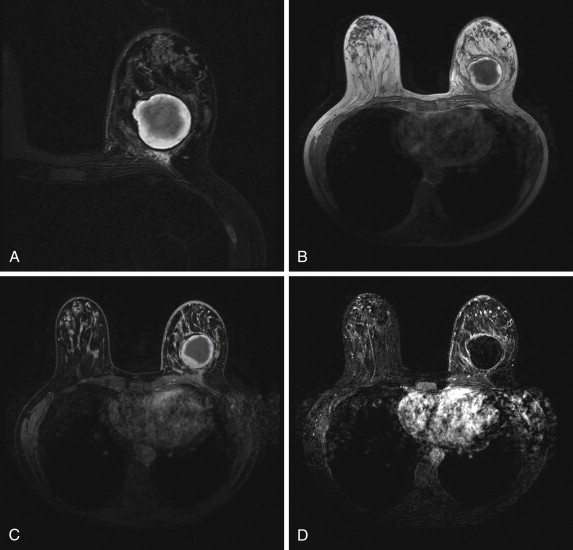
Fat Necrosis
Fat necrosis results from a vascular injury to fat cells within the breast and can be seen with any trauma to the breast, including invasive procedures such as needle or surgical biopsy, lumpectomy, mastectomy, reconstructive surgery, and radiation therapy to the breast. The imaging findings of fat necrosis have been well described in multiple modalities. Similar to other imaging modalities, the appearance on MRI can be variable, including oil cysts, architectural distortion, or a spiculated mass. Figure 10.4 demonstrates the classic appearance of fat necrosis by mammography and by DCE breast MRI. The most common MRI appearance is a round or oval mass with hyperintense T1-weighted signal that saturates on fat-saturated images and is compatible with a lipid cyst. Oil cysts may contain internal fat-fluid levels. Identifying central T1 hyperintensity on non–fat-saturated images helps confirm the diagnosis of fat necrosis. Fat necrosis will calcify over time, and therefore comparison with mammograms is often helpful in evaluating suspected fat necrosis and required for accurate interpretation of breast MRI. Overall, the MRI signal characteristics of fat necrosis typically follow that of fat elsewhere in the breast.

The enhancement pattern of fat necrosis is also widely variable. Kinetic assessment may demonstrate either benign or malignant type curves. The pattern of enhancement often correlates with the stage of fat necrosis evolution. The most malignant appearing enhancement occurs early after the inciting event and is secondary to acute inflammatory changes. As the inflammatory changes become chronic, granulation tissue develops, and the pattern of enhancement can change to reflect this evolution, with persistent or plateau delayed kinetics. However, fat necrosis is a great mimic of cancer, not only on MRI but also on all other imaging modalities. Therefore, if the lesion in question has suspicious morphologic or kinetic features, biopsy will be indicated. Two additional examples of fat necrosis are illustrated in the Reconstructive and Cosmetic Surgery section later.
Seroma/Hematoma
A hematoma is characterized by heterogeneous signal intensity and lack of contrast enhancement. However, hematomas can have rim enhancement secondary to surrounding inflammatory changes. The signal of blood varies depending on its age and the pulse sequence used for imaging ( Table 10.2 ). Chronic hematomas can demonstrate a low-signal intensity rim of hemosiderin on T1-weighted images.
| Stage | T1 Enhancement | T2 Enhancement |
|---|---|---|
| Hyperacute | Intermediate | Bright |
| Acute | Intermediate | Dark |
| Subacute: Early Late | Bright Bright | Dark Bright |
| Chronic | Dark | Dark |
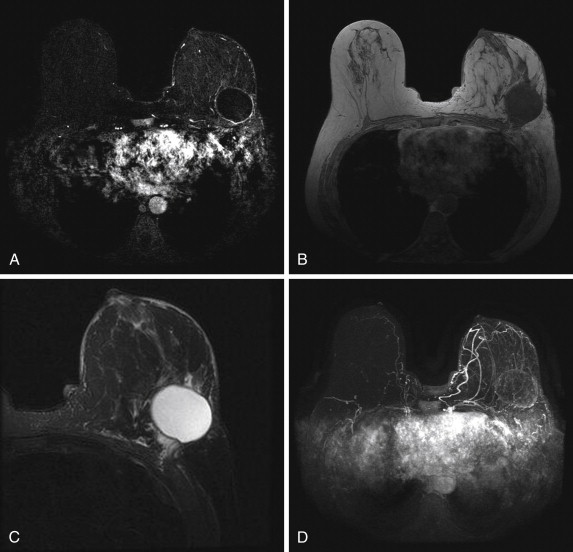
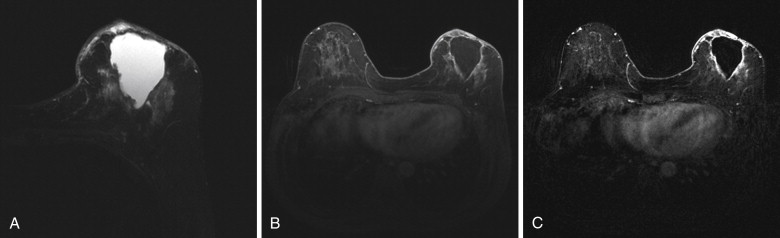
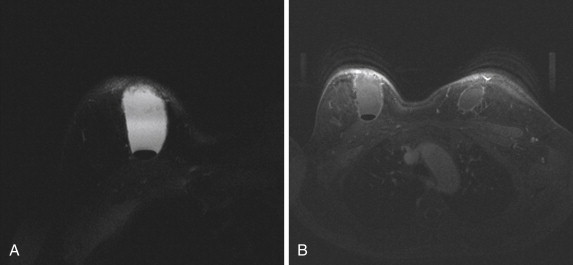
Seromas typically appear as fluid collections, with high signal intensity on T2-weighted sequences and low signal intensity on T1-weighted sequences and no internal enhancement ( Figure 10.5 ). Rarely, seromas can have rim enhancement, which is related to postprocedural inflammation, or focal or nodular enhancement that may represent residual disease, as is demonstrated in Figure 10.6 . Seromas usually resorb over time. However, the findings may also persist for months or even years. One study showed that 3.7% of women had a seroma persisting at 6 years or more after surgery. In the rare case in which DCE breast MRI is obtained in the immediate postsurgical period, air and fluid levels may be present in the dependent portions of the lumpectomy cavity. This is demonstrated in Figure 10.7 in a patient 2 days after surgery.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree