Mucinous Cystic Pancreatic Tumor
Brooke R. Jeffrey, MD
Michael P. Federle, MD, FACR
Key Facts
Terminology
Thick-walled, uni-/multilocular, low-grade malignant tumor composed of large, mucin-containing cysts
Imaging
Enhancing multiseptated mass in body or tail of pancreas
Enhancement of thin internal septa and cyst wall ± calcification
MRCP: Depicts displacement, narrowing, and prestenotic dilatation of pancreatic duct
Top Differential Diagnoses
Pancreatic pseudocyst
Pancreatic serous cystadenoma
Pancreatic IPMN
Cystic islet cell tumor
Pancreatic epithelial (true) cyst
Variant of ductal adenocarcinoma
Lymphangioma (mesenteric cyst)
Pathology
Considered pre- or frankly malignant
Clinical Issues
Asymptomatic, epigastric pain, palpable mass
Diagnosis: Endoscopic ultrasound with cyst aspiration/cytology
Surgical resection
Diagnostic Checklist
Multiloculated cystic mass with enhancing septa in pancreatic body or tail
Usually requires resection; may not warrant additional imaging
TERMINOLOGY
Synonyms
Mucinous macrocystic neoplasm, macrocystic adenoma, mucinous cystadenoma or cystadenocarcinoma
Definitions
Thick-walled, uni-/multilocular, low-grade malignant tumor composed of large, mucin-containing cysts
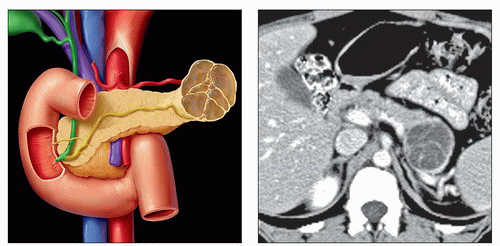
IMAGING
General Features
Best diagnostic clue
Enhancing multiseptated mass in body or tail of pancreas
Location
Tail of pancreas (more common)
Size
2-12 cm in diameter
Morphology
Classified under pancreatic mucinous tumors along with intraductal papillary mucinous neoplasm (IPMN) of pancreas
Mucin-producing tumors must be considered when cystic lesions of pancreas are found
Considered premalignant or frankly malignant
Radiographic Findings
ERCP
Displacement and narrowing of main pancreatic duct adjacent to tumor
CT Findings
NECT
Hypodense unilocular or multilocular cyst
Focal calcifications may be seen (16% of cases)
Location: Wall, septum, or periphery
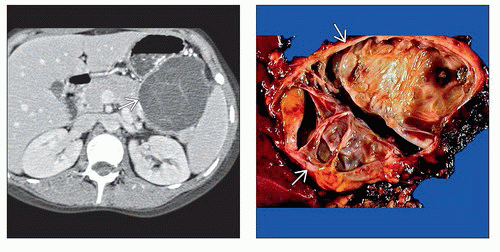
CECT
Multilocular cystic lesion
Enhancement of thin internal septa and cyst wall ± calcification
Unilocular cystic lesion
Enhancement of cyst wall
MR Findings
T1WI
Variable signal intensity based on cyst content
Fluid-like material: Hypointense
Proteinaceous or hemorrhagic: Hyperintense
Focal calcifications: Hypointense
T2WI
Cysts: Hyperintense
Internal septations: Hypointense
Focal calcifications: Hypointense
T1WI C+
Fat-suppression sequence
Enhancement of septations and cyst wall
MRCP
Depicts displacement, narrowing, and prestenotic dilatation of pancreatic duct
Ultrasonographic Findings
Grayscale ultrasound
Multiloculated cystic mass with echogenic internal septa
Less common: Unilocular anechoic mass
Imaging Recommendations
CECT or MR ± MRCP
DIFFERENTIAL DIAGNOSIS
Pancreatic Pseudocyst
Inflammatory changes in peripancreatic fat
Pancreatic calcifications and temporal evolution of lesion
Communicates with pancreatic duct (70% of cases)
Clinical history of pancreatitis or alcoholism
Lab data: Increased amylase (in cyst and serum)
Simulates unilocular mucinous cystic tumor
Pancreatic Serous Cystadenoma
Large, well-defined, encapsulated, sponge-like mass in pancreatic head
Innumerable small cysts separated by thin septa
Central scar with calcification
Calcification more common in serous than mucinous pancreatic neoplasms (38% vs. 16%)
Macrocystic variant of serous cystadenoma
Difficult to distinguish from mucinous tumor
Serous lesion usually has thinner wall
Pancreatic IPMN
Low-grade malignancy arises from
Main pancreatic duct (MPD)
Branch pancreatic duct (BPD)
Combined MPD and BPD
BPD or combined IPMN types may simulate mucinous cystic neoplasm due to presence of dilated cystic branch ducts in pancreatic tail
Cystic Islet Cell Tumor
Usually non-insulin-producing and nonfunctioning
Tumor: Cystic on NECT
Cyst wall shows enhancement; nonenhancing cyst contents
No pancreatic ductal dilatation
Angiography: Hypervascular primary and secondary
Pancreatic Epithelial (True) Cyst
Examples: von Hippel-Lindau disease and autosomal dominant polycystic kidney disease (ADPKD)
Rare; usually small and multiple nonenhancing cysts
No pancreatic ductal dilatation
Variant of Ductal Adenocarcinoma
Mucinous colloid adenocarcinoma or mucin-hypersecreting cancer
Pancreatic ductal obstruction and dilatation
Local invasion and regional metastases
Lymphangioma (Mesenteric Cyst)
Often extends from or into retroperitoneal soft tissues
Water density; imperceptible wall; thin septa
PATHOLOGY
General Features
Etiology
Uncertain
Embryology, anatomy
May be related to germ cell migration during 1st 8 weeks of gestation
Neoplasm with number of cysts 2-6 cm in diameter seen in 95% of cases
Stromal component is key for diagnosis of mucinous cystic neoplasm
Tumor shares both clinical and pathologic characteristics of biliary and ovarian tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree