(1)
Princess Elizabeth Hospital Le Vauquiedor St. Martin’s Guernsey, Channel Islands, UK
(2)
Brighton and Sussex Medical School, Brighton, England UK
Abstract
In 1986, Rosen described an entity he termed a mucocoele-like lesion (MLL) in six women aged between 26 and 61 years. Only one patient was postmenopausal. These lesions consisted of duct–lobular units that were dilated and distended with mucin, which extravasated into the surrounding stroma, reminiscent of salivary gland lesions. In five patients the MLL presented as a symptomatic mass, and in another patient it was an incidental finding in association with intraductal carcinoma. From his observations, Professor Rosen concluded that MLLs should be included in the differential diagnosis of mucinous carcinoma and the lesions in young patients should be treated with caution, as mucinous carcinoma is rare in this age group. The pathogenesis of MLLs is unclear. Breast epithelium secretes acid and neutral mucins, which are present in both benign and malignant lesions (Spicer et al. 1962). MLL most likely arises due to accumulation of mucin in the ducts and lobular units with resultant dilatations and subsequent leakage of the mucin into the surrounding stroma. Mucocoele-like lesion and mucocoele-like tumour are used interchangeably in the publications.
Learning Points
MLLs are rare.
MLLs have a wide age range of presentation from mid-20s to 70s.
Most lesions are detected due to calcification on mammographic examination.
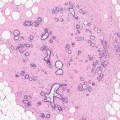
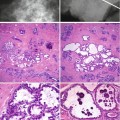
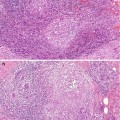
The hallmark of MLL is the presence of cystic ducts with associated mucin extravasation into the stroma.
MLLs can be associated with ADH, DCIS or mucinous carcinoma.
There are no pathognomonic radiological features of MLL.
All MLLs diagnosed on needle core biopsies require excision to exclude high-risk lesion.
The risk of MLL of progressing to malignancy is unknown
12.1 Background
In 1986, Rosen described an entity he termed a mucocoele-like lesion (MLL) in six women aged between 26 and 61 years. Only one patient was postmenopausal. These lesions consisted of duct–lobular units that were dilated and distended with mucin, which extravasated into the surrounding stroma, reminiscent of salivary gland lesions. In five patients the MLL presented as a symptomatic mass, and in another patient it was an incidental finding in association with intraductal carcinoma. From his observations, Professor Rosen concluded that MLLs should be included in the differential diagnosis of mucinous carcinoma and the lesions in young patients should be treated with caution, as mucinous carcinoma is rare in this age group. The pathogenesis of MLLs is unclear. Breast epithelium secretes acid and neutral mucins, which are present in both benign and malignant lesions (Spicer et al. 1962). MLL most likely arises due to accumulation of mucin in the ducts and lobular units with resultant dilatations and subsequent leakage of the mucin into the surrounding stroma. Mucocoele-like lesion and mucocoele-like tumour are used interchangeably in the publications.
12.2 Clinical Features of MLLs
In the original description by Professor Rosen (1986), MLLs presented symptomatically due to the presence of a palpable mass in young women. In the subsequent published studies, it appears that when MLLs presented symptomatically, the lesions arise in young women. In the older women, MLLs are detected mammographically through the screening programmes and in most cases due to the presence of microcalcification (Davies et al. 1995). When MLLs occur in young women, the lesions tend to be benign.
Cheng and colleagues (2004) reviewed the cytological features of 20 aspirates of mucinous lesions. The aspirates revealed 12 mucinous carcinomas, two MLLs with atypical ductal hyperplasia, three MLLs with ductal hyperplasia and three simple MLLs. The average age of the eight women with MLL was 26.3 years (range 20–32), and the women with mucinous carcinoma had an average age of 51.5 years (range 34–75 year). Although the paper does not indicate the clinical presentation, it is most likely that the women aged 20–32 years with MLL presented symptomatically. In a separate Chinese publication, Ding and Yang (2008) also reported benign MLLs in nine women aged between 23 and 43 years of age with a mean age of 34 years. All nine women presented with clinically palpable lumps.
12.3 Radiological Features of MLLs
Since the first edition of this book, more data have been published on MLLs, albeit most of them are based on retrospective review of archival material on the clinical presentation, radiological and pathological features of MLLs. Most of the reported series are on mammographically detected MLLs. As MLLs are rare, most published series consist of relatively few patients. The rarity of the MLL is illustrated in the study by Glazebrook and Reynolds (2003) who set out to evaluate the mammographic and sonographic features of MLLs. They reviewed breast lesions in their department coded as mucocoele or mucocoele-like tumour between 1992 and 2001. This small number of patients may be attributed to the lack of recognition of the lesion by the pathologists. They identified only five patients in over 10,000 specimens. The patients were a 29-year-old woman who presented with a mass and 41-, 48-, 51- and 73-year-old women whose lesions were mammographically detected. In this small number of patients, the mammographic appearances of the mucocoele-like tumours included a well-defined nodule, irregular nodule, well-defined nodule with calcification, cluster of indeterminate calcification and pleomorphic calcification. The sonographic features included well-defined hypoechoic mass with central septation, cluster of complex cysts with calcification and tubular hypoechoic structures with low-level internal echoes. Three women had benign MLLs on histology of the excision biopsy, and two women had MLLs with ADH. Although the number of patients is small, this study illustrated the heterogenous radiological features of MLLs.
In a separate study of 12 patients from a New Zealand Breast Screening Programme (Ramsaroop et al. 2005), the authors also reported that mammographic features of MLLs were non-predictive. The mammographic features consisted of calcification (10 patients) mass only (two patients) and calcification and a mass (one patient). The pathology was reported as benign MLLs in five patients, MLL with ADH in a single patient, MLLs with DCIS or LCIS in three patients and MLL with invasive ductal carcinoma in a single patient.
The mammographic features of MLL were further analysed by Carkaci and colleagues (2011) when they reviewed the radiological and pathological features of 44 patients to determine whether excision is always warranted on the diagnosis of MLLs on needle core biopsies. In this study the most common mammographic appearance was calcification which was reported in 61 % (27/44) patients; 18 % (8/44) patients had a mass only; 16 % (7/44) had masses with associated calcification; and 2 (5 %) patients had mammographically occult MLLs which were detected on ultrasonography performed for other reasons. The author further analysed the pattern of the calcification and noted that the calcification of MLLs associated with DCIS was clustered/grouped coarse and heterogenous (two patients). Similarly, calcifications in MLLs without atypia were clustered/grouped and heterogenous (10 patients). In contrast, the calcification in MLLs with atypia was clustered/grouped, fine and pleomorphic (six patients). Although the authors applied the BI-RADS lexicon in assessing the lesions, they did not indicate which categories the MLLs fell into. However, as the patients had needle core biopsies which prompted excision biopsies, therefore the mammographic abnormalities must have attained the threshold for biopsies, i.e. BI-RADS category 3 or above. In the same study by Carkaci and colleagues (2011), sonographic images were available in 17 patients and features included solid masses (seven patients), complex cysts (six patients) and negative ultrasound (four patients). Of the 13 patients with solid mass and complex cysts, four lesions had increased vascularity, another four lesions were avascular, eight lesions had posterior acoustic enhancement and four lesions had no posterior acoustic phenomenon. Although this study had more patients compared to other reported series, it just illustrates further that there are no radiological pathognomonic features of MLLs.
In an attempt to classify the MLLs according to BI-RAD5 criteria, Kim and colleagues (2011) retrospectively reviewed 72 MLLs in 68 women identified over a period of 10 years. They reported that calcification of indeterminate concern or higher probability of malignancy was more frequently present in MLLs with ADH or MLLs with malignancy than in pure MLLs (24/26 [92 %] vs. 17/27 [62.9 %]; p = 0.019). The calcification was more frequently clustered or segmental. At ultrasound 69 of the MLLs (95.8 %) were present as cystic masses. Cysts with thick septations, clustered cysts and complex masses were more frequently seen in MLLs associated with ADH or malignancy than in pure MLLs (26/29 [89.7 %] vs. 13/40 [32.5 %]; p = 0.001). Simple cysts, complicated cysts and cysts with thin septations were more frequently seen in pure MLLs than in MLL with ADH or malignancy (27/40 [67.5 %] vs. 3/29 [10.3 %]; p < 0.001). When the lesions were analysed according to the BI-RADS category, one lesion was classified as category 2; seven, category 3; 60, category 4; and four, category 5. The positive predictive value for BI-RADS category 4 was 13.3 % (CI, 6.9–24.2 %) and for BI-RADS category 5 was 50 % (CI, 15–85 %). All MLLs with malignancy were classified as category 4 or 5. The authors concluded that BI-RADS assessment can be applied in the management of MLLs.
12.4 Pathological Features of MLLs
When the MLLs were first reported by Professor Rosen in 1986, the lesions were benign and presented symptomatically. As the pathologists become aware of the lesion, the spectrum of the disease is much broader and includes mucin-filled ducts, mucinous ADH and mucinous DCIS to frankly malignant lesions (Hemele-Bena et al. 1996). However, the concept of a malignant MLL is difficult to reconcile with the established morphology of mucinous carcinoma which consists of lakes mucin freely dissecting through the stroma. Is a malignant MLL mucinous carcinoma? If so, this is in conflict with the original definition MLL by Rosen which was a benign lesion.
Based on the images illustrated in Rosen’s Breast Pathology (2009), a malignant MLL is classified as such if there is acellular extravasation of mucin into the stroma in association with DCIS and mucinous carcinoma.
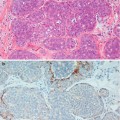
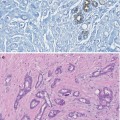
Cystically dilated mucin-filled ducts are usually identified as an incidental lesions in a specimen excised for other breast condition as illustrated in the fibroadenoma containing mucin-filled ducts (Fig. 8.13). However, mucin-filled ducts are more often than not present in association with the classical benign MLL or in association with mucinous carcinoma. Figure 12.1




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree