Multiple Myeloma
Todd M. Blodgett, MD
Alex Ryan, MD
Joanna Costello, MD
Key Facts
Terminology
Multiple myeloma (MM), monoclonal gammopathy of undetermined significance (MGUS)
Myeloma: Proliferation of clonal plasma cells and overproduction of monoclonal immunoglobulins
Imaging Findings
Increased activity in lytic lesion or extramedullary site on PET/CT
Multiple lytic or punched-out lesions are diagnostic of MM and are present in 75-90% of patients at diagnosis
Bone marrow and bone (97%)
PET/CT performs better than MR in the detection of focal lesions
Most studies have shown PET/CT reliable for bone lesions ≥ 1 cm using standard SUV cutoff of 2.5
PET provides accurate staging of untreated MM (solitary, multifocal)
Diffuse marrow uptake on PET usually indicates elevated plasma cell population
PET exceptionally useful in monitoring disease activity in patients with nonsecretory myeloma
Top Differential Diagnoses
Lytic Skeletal Metastases
Osteopenia, Osteoporosis
Other Bone + Soft Tissue Malignancy
Other Plasma Cell Neoplasms
Diagnostic Checklist
FDG PET/CT to stage and establish baseline for monitoring therapy (especially in nonsecretory myeloma)
TERMINOLOGY
Abbreviations and Synonyms
Multiple myeloma (MM), monoclonal gammopathy of undetermined significance (MGUS)
Definitions
Malignancy of antibody-forming plasma cells in bone marrow
Overproduction of monoclonal immunoglobulins
Causes a wide variety of manifestations
IMAGING FINDINGS
General Features
Best diagnostic clue
Multiple lytic or punched out lesions are diagnostic of MM
Present in 75-90% of patients at diagnosis
PET: Increased activity in lytic lesion or extramedullary site
Not all lesions are hypermetabolic
Location
97% of cases present in bone and bone marrow
Spine is the most common site of involvement of myeloma
Due to presence of red marrow in axial skeleton throughout life
Common extramedullary sites of occurrence: Paranasal sinuses, nasopharynx, tonsils
Less common: Lung, spleen, liver
Osteonecrosis of humeral and femoral heads reported in up to 10% of MM patients
Area of involvement is often asymptomatic
Risk factors include treatment with dexamethasone, male gender, younger age
Morphology
Increased complement of plasma cells in marrow and lytic bone lesions
Plasma cells > 10-15% of marrow cells
May present as solid mass (plasmacytoma) in bone or soft tissue
Imaging Recommendations
Best imaging tool
Prior to imaging, confirm disease via lab work and analysis of bone marrow aspiration
FDG PET useful for
Evaluation of disease activity
Detection of extraosseous disease involvement
Direction of local therapy (e.g., radiation)
Assessment of patients with nonsecretory myeloma
Evaluation of response to therapy
FDG PET/CT with contrast
Superior to MR in the detection of focal lesions
MR better for diagnosis of diffuse disease pattern
Limited window (spine and pelvis) reduces sensitivity
Generally reserved for evaluation of bone marrow in spine and pelvis
Improved ability to detect both focal and diffuse disease
Protocol advice
For detection of diffuse disease, obtain PET/CT from top of head to toes
For patients not affected by renal failure (which is common in MM), use oral and IV contrast-enhanced CT
Marrow stimulant drugs may mask underlying MM lesions
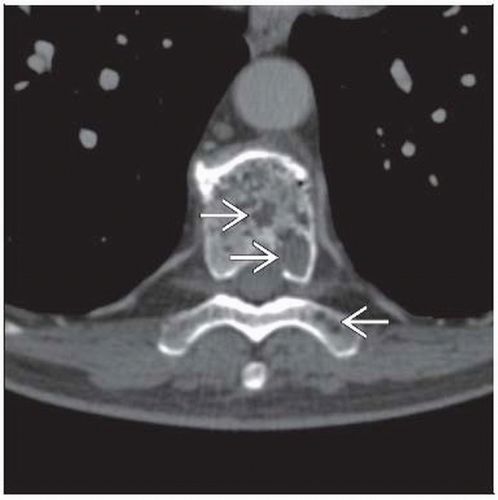
CT Findings
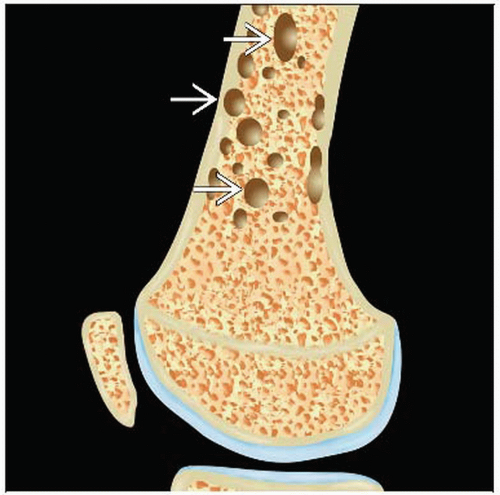
Plasma cell tumors in bone → ↑ osteoclasts and ↓ osteoblasts → “punched out” lesions in flat and long bones
NECT is indicated for evaluation of cortical destruction and intra-/extraosseous extent of tumor
Up to 30% demineralization required before lytic lesion may be detected
CT useful to guide percutaneous biopsies
Findings
Multiple well-defined, rounded, lytic, punched out lesions
Usual sites: Skull, spine, pelvis
Cortical and cancellous bone erosion
Endosteal scalloping (may be subtle)
Diffuse osteopenia, osteoporosis, osteolysis, with accentuated trabecular pattern
Minimal periosteal new bone formation
Lesions often become sclerotic after therapy
Spine
Vertebral collapse
Large endplate depressions
Sparing of posterior elements
Paraspinal/epidural soft tissue mass adjacent to bone destruction
Plasmacytoma
Solitary expansile lesions present in 10% of cases
May appear as bubbly expansion of single bone
Occasionally associated with soft tissue mass
Represents early stage of melanoma (progresses to multiple lesions)
Presents most commonly in ribs, pelvis, long bones
Discovery of second myeloma lesion upstages patient’s disease from I to III
Benign fracture suggested by
Retropulsed posterior fragment
Cortical fragments without destruction
Identifiable fragment lines within cancellous bone
Intravertebral vacuum phenomenon
Thin diffuse paraspinal soft tissue mass
Nuclear Medicine Findings
General
False positives seen with infection, inflammation, post-surgical changes, and hemangioma
Initial diagnosis
Most studies have shown PET/CT reliable for bone lesions of at least 1 cm using standard SUV cutoff of 2.5
Any lesions smaller than 5 mm with uptake should be considered positive, regardless of SUV
Stable MGUS may be diagnosed based on negative whole body PET in patients with monoclonal gammopathy
PET/CT can be useful for diagnosing infection, even with severe neutropenia/lymphopenia
Staging
FDG PET highly accurate for staging of untreated MM (solitary and multifocal)
Accurate staging is critical for treatment decisions and prognosis
FDG PET helps accurately delineate target volumes for radiotherapy planning
PET/CT leads to change in management in up to 70% of cases and upstaging of disease in up to 37.5%
Extramedullary plasmacytoma: FDG PET leads to management changes in more than 25% of patients
Due to presence of additional sites of disease in 33% of cases
Prognosis dismal for patients with extramedullary FDG-avid disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree