Introduction
Musculoskeletal ultrasound has become increasingly common over the last two decades. The possibility of a real-time, dynamic imaging modality that is both low cost and safe are among the key driving forces making this an important component of patient care for orthopedic presentations. Ultrasound-guided diagnostic and therapeutic procedures have become the cornerstone of many nonoperative sports medicine practices, as ultrasound guidance increases the efficacy and safety of many bedside procedures. Musculoskeletal ultrasound can be used to diagnose disorders of bone, joints, ligaments, tendons, muscles, nerves, and vascular structures.
Tendinopathy vs. Tenosynovitis
For decades, the condition now known as tendinopathy has been incorrectly called tendinitis or tenosynovitis . Tendinitis was often a “wastebasket” diagnosis, lumping together any injury to a tendon. Largely as a result of the work of Karim Khan, the two conditions have been identified separately as two distinct entities and are treated each in their own way. This distinction is critical to the musculoskeletal ultrasonographer, because each has its own image characteristics, which lead to a distinctly different treatment.
Tendinopathy describes noninflammatory degeneration of a tendon with structural changes more consistent with scar tissue rather than inflammation. At the cellular level, tendinopathy describes chronic, degenerative change to a tendon with eosinophilic infiltration, fibrillar degeneration, and loss of organization of the vascular structure with disorganized tendon structure. Tendinitis or tenosynovitis describes an acute inflammatory process with migration of white blood cells, edema surrounding the tendon, and mobilization of inflammatory mediators.
On musculoskeletal ultrasound imaging, a normal tendon appears as a well-organized linear structure, often described as fibrillar, with an even “copper wire” appearance or the appearance of neatly combed hair ( Fig. 28.1 ).

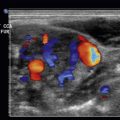
Tendinopathy takes on the appearance of broken lines, with an uneven, disorganized tendon matrix, often with thickening of the tendon structure showing a hyperechoic signal. On Doppler enhancement, the images will show patchy uptake of circulation, which does not appear with normal tendon ( Fig. 28.2 ).

Tenosynovitis shows a classical anechoic ring in the transverse image of the tendon, the “target sign” consistent with fluid, or edema. Longitudinal images show anechoic fluid surrounding the peroneus longus and peroneus brevis tendons ( Fig. 28.3 ).

Achilles Tendon Rupture
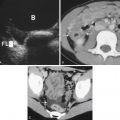
Achilles tendon rupture is one of the most common and disabling tendon ruptures, typically affecting women and men between the ages of 30 and 50. It occurs when an acute tensile overload is applied to a tendon that has been weakened by chronic, repetitive overuse microtrauma. Tendon weakening is visualized on musculoskeletal ultrasound as anechoic cystic formations embedded in the normal fibrillar tendon appearance on both longitudinal and transverse views ( Fig. 28.4 ). When the tendon has completely or partially ruptured, an anechoic gap is visualized in the longitudinal view that interrupts the fibrillar tendon ( Fig. 28.5 ). Image resolution of the Achilles tendon structure with static and dynamic images is superior to magnetic resonance imaging (MRI) in confirming this diagnosis and can be done in the examination room.


A dynamic Thompson test (squeezing the gastric-soleus muscle complex) will result in the loss of plantarflexion of the ankle on physical examination. This dynamic test can be replicated under real-time imaging of the Achilles tendon in longitudinal orientation, showing an increasing anechoic gap in the tendon structure with manual forced dorsiflexion. Dynamic testing of the Achilles tendon can decrease the false-negative rate of static imaging of a torn Achilles tendon.
Proximal Biceps Tendon Ruptures
Both acute tensile overload and repetitive microtrauma result in biceps tendon tears. The proximal biceps tendon is the more common location for a tear of the long head of the biceps (97%) compared with distal tears (3%).
Longitudinal views of the long head of the biceps just inferior to the bicipital groove on the anterior humerus can visualize the musculotendinous junction of the biceps muscle and tendon and show the characteristic anechoic gap with a tear ( Fig. 28.6 ). Dynamic testing of the long head of the biceps with internal and external rotation of the humerus often shows the absence of the long head of the biceps tendon within the bicipital groove, a characteristic finding with a complete tear.

Distal Biceps Tendon Ruptures
Tears of the distal long head of the biceps tendon are far less common than proximal tears but much more difficult to visualize. The Mayo Clinic “pronator window” approach by Jay Smith et al. is our favored diagnostic ultrasound imaging method, where visualization of the absent distal biceps tendon is performed while pronating and supinating the radius and ulna, showing the absence of the tendon. To perform this examination, place the high-frequency transducer on the medial aspect of the forearm over the pronator muscle and direct the ultrasound beams toward the distal biceps tendon and proximal radius. The transducer is oriented along the long axis of the biceps brachii tendon ( Fig. 28.7 ). As the patient is brought into supination, the insertion of the distal biceps brachii tendon is brought into view.