NASOLACRIMAL APPARATUS: DEVELOPMENTAL CONDITIONS
KEY POINTS
- Imaging is not required in the vast majority of patients with a developmental condition of the nasolacrimal apparatus.
- Computed tomography, magnetic resonance imaging, and ultrasound can be used to definitively confirm these conditions.
- Computed tomography may be used in confusing cases to sort out bony anatomy.
Developmental abnormalities of the orbit and nasolacrimal apparatus may be isolated findings. Nasolacrimal apparatus anomalies are not often associated with other findings involving the eye or orbit and not usually part of syndromes and other more generalized genetic errors. The orbital anomalies related to eye development are discussed in Chapter 46. Those associated with craniofacial anomalies are discussed in Chapter 79.
Any orbital mass or disease process may be approached by first establishing whether it is preseptal (Chapters 70 and 71) or postseptal (Chapters 57–60, 62, and 64). Nasolacrimal apparatus problems are generally preseptal in their manifestations. Most of these, such as absence of the valves of Hasner and those of the puncta and canaliculi, do not come to imaging, even dacryocystography. This chapter essentially discusses dacryostenosis, which is a common abnormality that only occasionally comes to imaging, and even more unusual entities that may present in infants as an inferior medial orbital mass or airway obstruction.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The lacrimal system develops from the first pharyngeal arch. The external and middle ear structures also arise from the first and second pharyngeal arches and from the related pharyngeal cleft and pouch.1,2 Disorders of canalization of the nasolacrimal duct system cause congenital dacryostenosis.
Applied Anatomy
The relevant anatomy of the nasolacrimal drainage system is discussed in detail in Chapter 44.
IMAGING APPROACH
Techniques and Relevant Aspects
The orbit is studied with computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Studies for anomalies of the nasolacrimal system are done without contrast except if a complicating infection may be present.
Pros and Cons
Ultrasound simply confirms the diagnosis and may identify this condition in utero.
Dacryocystography is not necessary.
CT may also be done without contrast to confirm an origin of a nasal aperture region mass or nasolacrimal sac distension due to dacryostenosis or atresia in unusual or confusing cases.
DEVELOPMENTAL CONDITIONS
Dacryostenosis/ Atresia and Other Rare Occurrences
Etiology
Dacryostenosis/Atresia is a spontaneous and very common anomaly. It is only rarely syndromic or associated with other conditions, although it might be present in patients with midface anomalies and clefts (Figs. 67.1 and 67.2). Other developmental conditions requiring imaging are rare (Figs. 67.3 and 67.4).
Prevalence and Epidemiology
Nasolacrimal obstruction occurs in 2% to 4% of newborns. The vast majority of these cases are resolved with duct probing. Very few come to imaging.1,2
Clinical Presentation
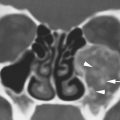
Nasolacrimal obstruction presents with tearing, nasolacrimal sac distension, and very rarely nasal aperture airway symptoms (Figs. 67.1–67.3).
Pathophysiology and Patterns of Disease
The end of the nasolacrimal duct beneath the inferior turbinate fails to completely canalize. This can result in essentially a “mucocele” or “amniocele” (in utero) of the sac and duct. High-grade obstruction can lead to marked enlargement of the canal that, if bilateral, can actually occlude the nasal aperture (Fig. 67.2). This may be associated with nasolabial cysts.
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
CT and magnetic resonance imaging will show a dilated lacrimal sac and possibly bony stenosis or atresia of the terminal end of the nasolacrimal canal (Figs. 67.1 and 67.2). These structures will be fluid filled. The bony canal may be enlarged, sometimes markedly so.
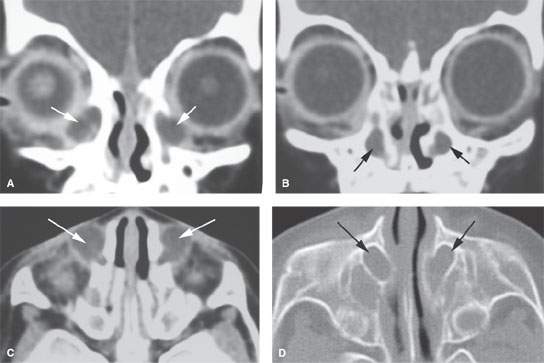
FIGURE 67.1. Computed tomography of a newborn presenting with bilateral palpable masses in the inferior medial aspect of the orbit and some upper airway noisiness. A: Coronal section shows bilateral distention of the lacrimal sacs (arrows). B: A coronal section slightly more posterior than (A) shows dilatation of the nasolacrimal ducts and canals (arrows). C: Axial section demonstrates the enlarged lacrimal sacs (arrows). D: Bone windows show the chronically enlarged nasolacrimal canals (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree