NASOPHARYNX: INTRODUCTION
TECHNICAL ASPECTS
Techniques and Relevant Aspects
General Examination Technique
Patients should be positioned so that the hard palate is perpendicular to the tabletop—a position that usually assures the infraorbital meatal line will also be perpendicular to the tabletop. This will mean that the proper anatomic relationship of the pharynx to the skull base will be maintained in this plane of data acquisition. When using multidetector computed tomography (MDCT), the data acquisition will then be done with zero gantry tilt. This may cause problems at the junction of the nasopharynx and oropharynx when dental fillings are present. If the images are severely degraded by artifacts arising from dental appliances, the gantry may be angled and second series of computed tomography (CT) images may be obtained or a complementary magnetic resonance (MR) study can be done. Such gantry angling is typically necessary for oropharyngeal lesions but is not usually necessary for those arising in the nasopharynx or adjacent deep spaces.
Nasopharyngeal CT and magnetic resonance imaging (MRI) always include axial and coronal views as a routine with relatively selected use of sagittal sections. On CT studies, axial volume CT data sets should be obtained with 0.5- to 1.0-mm sections that will provide for reconstructions and/or multiplanar reformations (MPRs) of sufficient resolution to provide definitive bone detail of the skull base. Reconstruction of the images at 1- to 3-mm slice thickness (SLT) is suitable for evaluating the soft tissue extent of cancers since reconstructing at that larger range of SLT will improve low-contrast resolution to some extent, as discussed in Chapters 1 and 2. The axial and coronal images are the mainstay for evaluating pathologic relationships at the most critical anatomic sites. MDCT (especially $16 slices) makes it easy to obtain a volume data set routinely reconstructed as axial images viewed at appropriate window settings with MPR tools in any plane required.
Additional coronal reconstructions with a bone algorithm may be part of cancer protocols (Appendix A) since bone invasion is an important factor in medical decision making in the vast majority of nasopharyngeal malignancies. Subtle but significant bone changes can be missed when viewing bone windows on images only reconstructed with a soft tissue algorithm (Figs. 21.41–21.43). Additional thinner reconstructions with bone windows may be necessary from saved raw data whenever bone is threatened and definitive information is not available on images of lesser spatial resolution or bone detail.
Iodinated contrast is used on almost all nasopharyngeal CT studies. If iodinated contrast cannot be used, then MRI should be done instead unless only bone information is the issue of interest. It is very important not to begin scanning too early in the contrast injection. Peak enhancement of most cancers, as well as other pathology not of blood vessel origin, relative to normal tissue may be missed if scanning begins to early. Specific CT protocols are presented in Appendix A.
MRI should be done with 3- to 4-mm sections and a field of view of about 12 to 16 cm depending on the size of the patient. All three orthogonal planes are obtained, but axial and coronal sections usually provide all of the critical information. T1- and T2-weighted images should be obtained. Fat suppression may be used but may be unpredictably degraded by susceptibility artifacts in critical areas, such as the skull base adjacent to a well-aerated sphenoid sinus. Such artifacts can obscure important details relative to a paracavernous course of cranial nerves III through VI as discussed in Chapters 1 and 3 (Figs. 1.3 and 1.4). T1-weighted non–fat-suppressed images before and after contrast and T2-weighted images are a choice that will avoid such artifacts, although this approach lengthens the examination. Intravenous contrast is used in most cases. MR protocols are presented in Appendix B.
MRI is done in the axial plane, always parallel to the hard palate of the infraorbital-meatal line. Coronal acquisitions are done routinely since the relationship between the pathology and the central skull base is almost always in question. Sagittal images are routinely useful to show spread of pathology relative to the clivus and body of the sphenoid.
Pros and Cons
CT and MRI are used for the majority of imaging of the nasopharynx. Dental-related artifacts can seriously degrade both CT and MR images through the mid oral cavity; this problem is generally worse on CT. The artifacts are accentuated on MRI when fat suppression is used (Fig. 1.4 and Chapter 1). These problems usually do not significantly impact medical decision making or treatment planning in nasopharyngeal-origin pathology. MRI sections above the hard palate are not frequently significantly degraded by jaw and other motion.
Ultrasound has no role in nasopharyngeal pathology.
Angiography is used occasionally in both diagnosis and treatment settings. Catheter angiography is necessary if angioarchitecture and temporal flow dynamics of a lesion, such as might be used to identify a juvenile angiofibroma, or an active leak are in question. Those indications will continue to decrease with the dispersion of MDCT 320 or a similar detector size. If not, CT and/or MR angiography will usually suffice. Angiography is almost always used following imaging studies, although it is occasionally the primary examination (e.g., intractable bleeding) or a prelude to endovascular procedures.
Radionuclide studies, particularly single photon emission computed tomography (SPECT) gallium and bone scanning, are useful in highly selected cases of infectious disease. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) is used selectively in cancer patients. It should not be used routinely. Specific radionuclide technique depends on the indications, and this is discussed elsewhere in Chapter 5.
Specific Areas of Interest
Developmental Abnormalities
These anomalies are studied with a combination of CT and MRI. CT is used when bone detail is critical to diagnosis and three-dimensional planning or craniofacial reconstruction. MR is used to look for an intracranial connection of the nasopharyngeal process and associated brain and other intracranial congenital anomalies.
Potentially cystic congenital lesions with a complex relationship to the nasopharynx and related deep facial spaces are very effectively imaged with MRI, especially in children where one would like to limit exposure to ionizing radiation (Figs. 8.23, 8.24, 10.12, and 142.1).
If MRI, CT, or the clinical evaluation suggests a venolymphatic or other vascular malformation, then angiography is occasionally done to confirm this impression and/or is used to direct endovascular or percutaneous ablative therapy. Such treatment may be definitive or an adjunct to surgical removal.
Inflammatory Disease
Complex inflammatory disease of the nasopharynx, such as that associated with skull base osteomyelitis, and diseases such as Wegener granulomatosis are studied with contrast-enhanced computed tomography (CECT) and MRI. Radionuclide bone gallium scanning is used occasionally as a supplemental diagnostic study as well as to monitor the progress of antimicrobial therapy (Figs. 13.5, 13.12, 16.1, 16.2, and 142.2).
Staging of Known Nasopharyngeal Cancer and Evaluation of Masses of Uncertain Etiology
Both CT and MR can be used to demonstrate the presence, possible nature, and extent of a mucosal or submucosal nasopharyngeal mass lesion. Parapharyngeal and other deep facial masses that may affect the nasopharynx were introduced in Chapter 142 and discussed in detail throughout Section VI. In some cases, both an MRI and CT study are necessary for these indications. A variety of sometimes unusual lesions, either benign or malignant, can be encountered in this clinical context. As the initial biopsy results may be inconclusive or negative, MR can be particularly useful to further characterize the lesion. In most patients, MR is the best starting point for suspected or documented nasopharyngeal cancer. MRI detects subtle soft tissue infiltration better than CT, making it the first choice for detection of early or submucosal cancers (Fig. 1.5) or infiltrating benign processes such as Wegener granulomatosis (Fig. 21.2). MR is also better than CT for evaluation of infiltration of the marrow spaces of the skull base, as discussed in Chapters 1 through 3 and 14 (Figs. 14.5 and 21.8).
Both MR and CT can supply information needed by the clinician for optimal treatment planning. The studies are complementary. CT studies are easier to execute and more reproducible than MRI because of the short data acquisition time that may result in less image motion degradation. This is much less a problem than at anatomic sites below the hard palate. MDCT systems also now offer high-quality multiplanar imaging, with the image quality often equivalent in diagnostic information to multiplanar MR images, especially when the CT superiority in rendering cortical bone detail is included in the comparison. The evaluation of cortical bone on CT is superior to that of MRI, and this can be a critical factor. CT detects calcifications better than MRI, but this is only infrequently significant in nasopharyngeal diseases. These factors are discussed in Chapters 1 through 3, 14, and 21. CT is better and easier to perform and interpret than MRI with regard to the extent of metastatic adenopathy, but this is a less critical factor than for other upper aerodigestive tract head and neck region primary sites (Chapter 188).
FDG-PET should play a selective role, but not a primary role, in nasopharyngeal cancers. It is most useful in looking for recurrence after treatment. It should not be used as a routine staging procedure since it is unlikely to alter management or affect outcome.
Velopharyngeal Function and Sleep Apnea Airway Evaluations
Fluoroscopic monitored studies during speech formation are done to document velopalatal coordination during speech. These are nowadays more typically performed by physicians specializing in communicative disorders than by diagnostic radiologists.
Static volumetric or dynamic MRI techniques might be used to assess the behavior of the airway at risk in patients with sleep apnea.
Controversies
In general, MRI is the preferred starting point for evaluating nasopharyngeal and parapharyngeal masses, but CT may be preferred as the initial study in some practices. This is more a matter of preference than controversy.
The standard or “routine” use of FDG-PET in the initial evaluation in head and neck cancer remains unsubstantiated. FDG-PET should be used with discernment in the nasopharynx with regard to its likelihood of contributing, in any individual case, to medical decision making that might measurably improve outcomes.
NORMAL ANATOMY
General Description
The nasopharynx is a muscular tube that connects the nasal cavity to the oropharynx, maintaining that part of the airway relatively rigidly open (Fig. 184.1A,B). This muscular and membranous tube attaches to the central skull base so that the floor of the sphenoid sinus and upper clivus form the nasopharyngeal roof. The nasopharyngeal mucosa and lymphoid tissue, referred to as the pharyngeal tonsils or adenoids, lie within the thick pharyngobasilar fascia and the pharyngeal and palatal musculature (Figs. 184.1D and 184.2–184.7) posteriorly and laterally. The soft tissue parapharyngeal space (PS) lies outside the pharyngobasilar fascia and musculature as described in Chapter 142 (Figs. 142.3–142.6). The pharyngobasilar fascia is largely responsible for holding the airway rigidly open for breathing, except during swallowing (Figs. 142.4A,B and 184.1D). The medial pterygoid plates are the anterior and lateral skeletal boundaries of the nasopharynx (Figs. 44.11 and 184.7 and Chapter 44). The lower clivus formed by the basiocciput and the upper cervical spine and related prevertebral musculature are its posterior deep musculoskeletal wall. The intervening soft tissue spaces along this posterior boundary are the retropharyngeal space (RS) and prevertebral space (PVS). The specific appearance of the airway contours varies considerably depending on the level of the section and the age of the patient.1
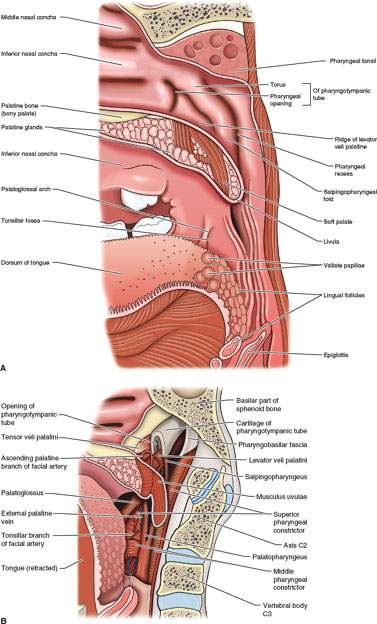
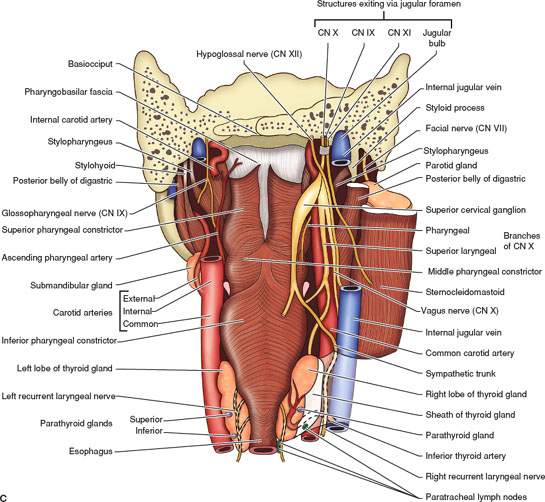
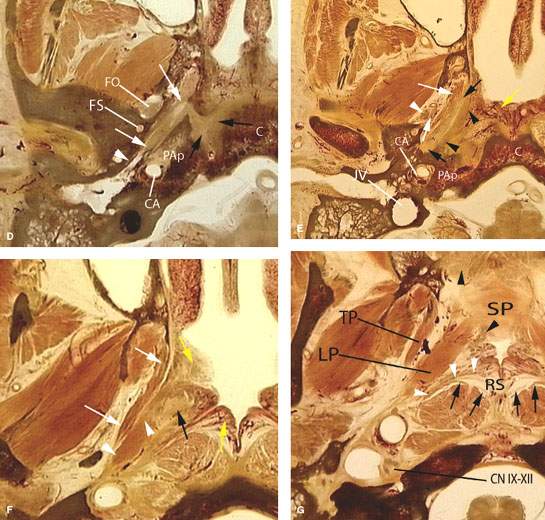
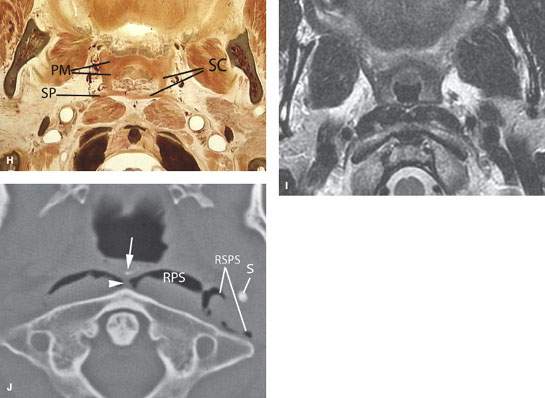
FIGURE 184.1. A series of anatomic diagrams and whole organ sections and a magnetic resonance (MR) image to demonstrate important anatomic relationships of the nasopharynx to the remainder of the pharynx and surrounding structures. A: Anatomic diagram showing the mucosal landmarks of the nasopharynx and their continuity with that of the oropharynx. B: Anatomic diagram showing the deeper muscle groups and eustachian tube that give rise to the mucosal landmarks in A. C: Anatomic diagram showing the three parts of the pharynx. The muscular tube suspends from the skull base with differentiating anatomic features based on the function of each portion of the pharynx. The tube is opened anteriorly to the nasal cavity and oral cavity. These openings define the major functions of the nasopharynx relative to the oropharynx. D: Whole organ section showing the relationship of the cartilage portion of the eustachian tube (ET) to important surrounding structures at the skull base. The cartilage portion of the ET is shown by the white arrows extending along the roof of the nasopharynx between the petrous apex (PAp) and the floor of the middle cranial fossa containing the foramen ovale (FO) and foramen spinosum (FS). The ET cartilage portion connects to the bony portion of the hypotympanum (white arrowhead). There is cartilage in the gap between the clivus (C) and petrous apex (black arrows); this is the so-called foramen lacerum. However, it is not a foramen at all. The carotid artery (CA) enters its vertical segment of the carotid canal in the petrous apex to turn forward above the foramen lacerum before entering the cavernous sinus. Note that the clivus and petrous apex contains a mixture of hematopoietic and fatty marrow. E: Whole organ section lightly inferior to that in (D). The course of the ET (black arrows) lies just lateral to the pharyngobasilar fascia (black arrowheads) as the ET cartilage attaches to the skull base. The origins of the tensor muscle of the soft palate (white arrows) separate the parapharyngeal space (PS) from the constituents of the nasopharynx. The third division of the trigeminal nerve lying just lateral to that musculature attachment at the skull base (white arrowheads) is in the masticator space. The lower clivus (C) is formed from the basiocciput, and the carotid canal lies at the junction of the petrous apex (PAp) and mastoid portions of the temporal bone. (CA, carotid artery; JV, jugular vein.) The somewhat vascularized lymphoid tissue of the nasopharynx, commonly called the adenoids, lines the mucosal surface of the nasopharynx (yellow arrow). F: A whole organ section made through the mid to lower third of the nasopharynx. The bulbous cartilaginous end of the ET (black arrow) produces a prominent bulge called the torus tubarius. The levator muscle of the soft palate arises largely from the ET (white arrowheads). The tensor muscle of the soft palate (white arrows) separates the nasopharynx from the masticator space. Lymphoid tissue that is partially vascularized and partially not vascularized (yellow arrows) lines the lumen of the nasopharynx. G: Whole organ section through the lower third of the nasopharynx just above its junction with the oropharynx. The lower fibers of the pharyngobasilar fascia (white arrowheads) separate the mucosa and submucosa of the nasopharynx from the retropharyngeal space (RS). The prevertebral fascia (black arrows) borders the posterior aspect of the RS. The tensor (TP) and levator (LP) muscles of the palate begin to merge with the soft palate (SP). The soft palate contains minor salivary gland tissue (black arrowheads). The carotid sheath is very well formed at this level, and cranial nerves IX through XII are plainly visible between the carotid artery and jugular vein (CNs IX–XII). H: The functional junction of the nasopharynx and oropharynx is formed by the Passavant muscle. The ridge produced by this functional zone of the superior constrictor converges with the palatal musculature to seal the nasopharyngeal airway during swallowing, protecting the airway from aspiration of swallowed contents. The pharyngeal musculature at this level includes the superior constrictor (SC) and stylopharyngeus (SP). The palatal musculature is made up of the confluence of the tensor and levator palatal muscles (PM). From the arrangement of these muscles, it seems simple to understand how when contracted they seal the nasopharynx during swallowing and when appropriate during speech formation. I: T2-weighted MR image to correlate with the anatomy shown in (G) at the junction of the nasopharynx and oropharynx. J: Computed tomography of the nasopharynx in a trauma patient with air in the RS, showing its relationship to the retrostyloid PS. The raphe (arrowhead) creates no real boundary in the space. The calcific densities (arrow) are common normal variations in lymphoid tissue. (S, styloid process.) (A, B from Cummings CW, Fredrickson JM, Harker LA, et al. Otolaryngology: Head and neck surgery. St. Louis, Mo: Mosby; 1986.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








