This article provides an overview of the national initiatives developed for monitoring and reporting quality performance measures. Included is a review of the Physician Quality Reporting System, the Hospital Outpatient Quality Data Reporting Program, and the Hospital Outpatient Prospective Payment System, with specific emphasis on how these programs affect radiology practice. A practical review of these programs allows radiologists to gain further understanding of the economic and political influences on the daily practice of radiology today. The background and relevant features of each program are presented in this article.
- •
The Physician Quality Reporting System is an incentive payment program for eligible physicians who satisfactorily report data on quality measures.
- •
The Hospital Outpatient Quality Data Reporting Program is a pay-for-quality data reporting program for outpatient hospital services.
- •
The Hospital Outpatient Prospective Payment System is used by the Centers for Medicare and Medicaid Services to reimburse for hospital outpatient services.
Introduction
This article provides an overview of national initiatives developed for monitoring and reporting quality performance measures. Included are a review of the Physician Quality Reporting System (PQRS), the Hospital Outpatient Quality Data Reporting Program (HOP QDRP), and the Hospital Outpatient Prospective Payment System (HOPPS), with specific emphasis on how these programs affect radiology practice. These programs are operated by federal agencies to measure and monitor the quality of healthcare practices at the individual physician and hospital levels, and for the implementation and regulation of an effective system of reimbursement. These programs are under the jurisdiction of the Centers for Medicare and Medicaid Services (CMS), previously known as the Health Care Financing Administration, which is a federal agency within the US Department of Health and Human Services that administers the Medicare program and works in partnership with states to administer Medicaid and the State Children’s Health Insurance Program. A practical review of these programs allows radiologists to gain further understanding of the economic and political influences on the daily practice of radiology today. The background and relevant features of each program are presented in this review.
Physician quality reporting program
Overview
This section provides a brief review of the PQRS, highlighting the program’s legislative history, eligibility requirements, and incentive payment plan. The PQRS program began in 2007 to provide an incentive payment to eligible physicians who satisfactorily report data on quality measures for covered Physician Fee Schedule (PFS) services furnished to Medicare Part B Fee-for-Service beneficiaries. Specifically, the PQRS measures applicable to the practice of neuroradiology are discussed. Several steps are suggested for individual physicians or group practices to start participation in the program. Resources are also provided for further information on the program requirements and the individual PQRS measures.
History and Background
The PQRS program is a relatively new program but has experienced a gradual process of transition since its inception. In 2006, the Tax Relief and Health Care Act established this program as an initiative to provide a 1.5% incentive payment with a cap for eligible physicians who satisfactorily reported data on quality measures for covered services furnished to Medicare. In 2007 the Medicare, Medicaid, and State Children’s Health Insurance Program Extension Act authorized continuation of the PQRS program for 2008 and 2009, which also provided a 1.5% incentive payment in 2008 and removed the cap established by the Tax Relief and Health Care Act. In 2008, the Medicare Improvements for Patients and Providers Act established the PQRS as a permanent federal program. It also increased the incentive payment to 2% of the total allowed charges for PFS-covered professional services in 2008 and 2009.
The Affordable Care Act, signed into law by President Obama in 2010, made several changes to the PQRS program. These changes included a gradual decrease in the incentive payment, requiring that quality measures eventually be met to receive the maximum Medicare payment for services. In 2011, the program decreased the incentive payment to 1% of the total allowed charges for PFS-covered professional services. The incentive will be further decreased to 0.5% in 2012 through 2014 and will eventually become a penalty starting in 2015 if not met. The expected starting penalty is a 1.5% reduction in the total allowed charges for PFS-covered professional services. In 2016, there will be further reduction to 2% in payment for services if the reporting measures are not met.
Quality Performance Measures
The PQRS program consists of more than 200 quality measures for Medicare patients including various aspects of care, such as prevention, chronic and acute care management, procedure-related care, resource use, and care coordination. Fifteen of these quality measures are applicable to diagnostic radiology, interventional radiology, or nuclear medicine as shown in Table 1 .
| Category | Measure No | Title |
|---|---|---|
| Stroke and stroke rehabilitation | 10 | CT or MR imaging reports |
| Perioperative care | 20 | Timing of antibiotic prophylaxis, ordering physician |
| Perioperative care | 21 | Selection of prophylactic antibiotic, first or second-generation cephalosporin |
| Perioperative care | 22 | Discontinuation of prophylactic antibiotics (noncardiac procedures) |
| Perioperative care | 23 | Venous thromboembolism prophylaxis (when indicated in all patients) |
| Prevention of catheter-related bloodstream infections | 76 | Central venous catheter insertion protocol |
| Health information technology | 124 | Adoption/use of electronic health records |
| Medication reconciliation | 130 | Documentation of current medications in the medical record |
| Radiology | 145 | Exposure time reported for procedures using fluoroscopy |
| Radiology | 146 | Inappropriate use of “probably benign” assessment category in mammography screening |
| Nuclear medicine | 147 | Correlation with existing imaging studies for all patients undergoing bone scintigraphy |
| Preventive care and screening | 173 | Unhealthy alcohol use, screening |
| Radiology | 195 | Stenosis measurement in carotid imaging reports |
| Radiology | 225 | Reminder system for mammograms |
| Preventive care and screening | 226 | Tobacco use: screening and cessation intervention |
The following three measures are applicable to most neuroradiologists in practice :
- 1.
Measure 10—Stroke and Stroke Rehabilitation: CT or MR Imaging Reports refers to the percentage of finalized reports for CT or MR imaging studies within 24 hours of arrival to the hospital for patients aged 18 years and older with either a diagnosis of ischemic stroke or transient ischemic attack or intracranial hemorrhage or at least one documented symptom consistent with ischemic stroke or transient ischemic attack or intracranial hemorrhage that include documentation of the presence or absence of each of the following: (1) hemorrhage, (2) mass lesion, and (3) acute infarction.
- 2.
Measure 195—Stenosis Measurement in Carotid Imaging Reports refers to the percentage of final reports for all patients, regardless of age, for carotid imaging studies (including neck MR angiography, neck CT angiography, carotid duplex sonography, and carotid angiography) performed that include direct or indirect reference to measurements of the distal internal carotid artery diameter as the denominator for the stenosis measurement.
- 3.
Measure 145—Radiology Exposure Time Reported for Procedures Using Fluoroscopy refers to the percentage of final reports for procedures using fluoroscopy that include documentation of the radiation exposure or exposure time.
Program Requirements
The PQRS is a voluntary incentive program. Submission of quality data codes through claims or a qualified registry indicates the intent to participate. In claims-based individual reporting, each eligible physician must report a minimum of three measures if applicable to his or her practice. There must be 50% compliance in a minimum of three measures to qualify for the incentive payment. However, if an eligible physician has less than three measures applicable to their practice, they are still able to participate in the program reporting on only their applicable measures. If fewer than three measures are reported, CMS may apply a measure-applicability validation process to determine eligibility for the incentive payment.
CMS uses two methods for assessing conformity to the requirements, referred to as “reporting compliance” and “quality compliance.” Reporting compliance reflects the percentage of eligible cases that have a PQRS code assigned. The incentive plan is based on obtaining reporting compliance. The physician performance data are published on-line as a list of the eligible professionals who satisfactorily report PQRS measures since 2009. Quality compliance refers to the percentage of reported cases that have completed the quality measure. Currently, quality compliance data are collected and monitored by CMS. Compliance is measured as a ratio: “denominator” refers to all eligible cases for a particular measure in your practice, and “numerator” refers to successful reporting of the measure.
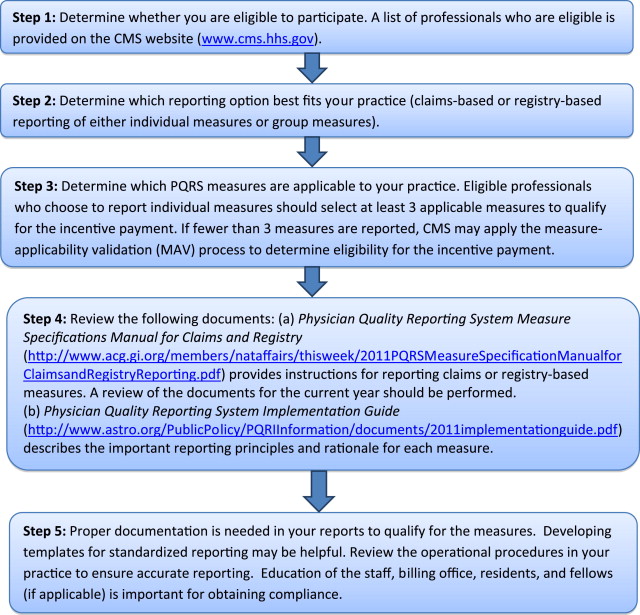
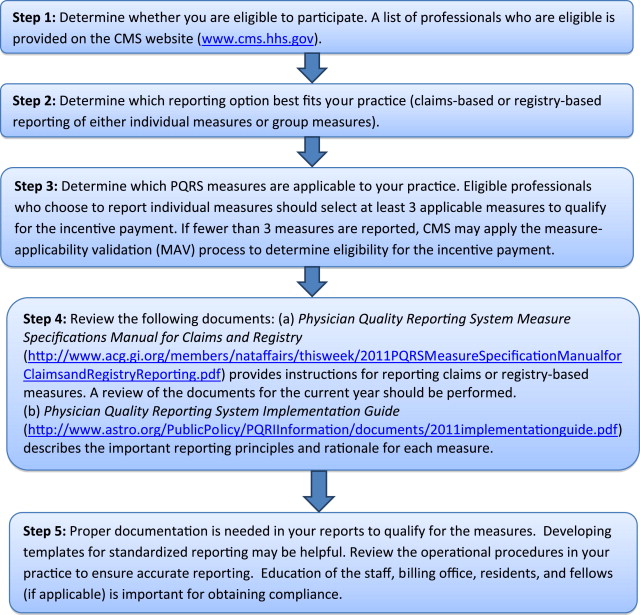
The beginning of this year’s cycle is January 1, 2012. However, you can start participating in the program during the mid-year cycle. Fig. 1 demonstrates five main steps to getting started.
Resources
More information and details can be found at the Centers for Medicare and Medicaid. A brief synopsis of the PQRS program can be found in the American Journal of Neuroradiology .
Physician quality reporting program
Overview
This section provides a brief review of the PQRS, highlighting the program’s legislative history, eligibility requirements, and incentive payment plan. The PQRS program began in 2007 to provide an incentive payment to eligible physicians who satisfactorily report data on quality measures for covered Physician Fee Schedule (PFS) services furnished to Medicare Part B Fee-for-Service beneficiaries. Specifically, the PQRS measures applicable to the practice of neuroradiology are discussed. Several steps are suggested for individual physicians or group practices to start participation in the program. Resources are also provided for further information on the program requirements and the individual PQRS measures.
History and Background
The PQRS program is a relatively new program but has experienced a gradual process of transition since its inception. In 2006, the Tax Relief and Health Care Act established this program as an initiative to provide a 1.5% incentive payment with a cap for eligible physicians who satisfactorily reported data on quality measures for covered services furnished to Medicare. In 2007 the Medicare, Medicaid, and State Children’s Health Insurance Program Extension Act authorized continuation of the PQRS program for 2008 and 2009, which also provided a 1.5% incentive payment in 2008 and removed the cap established by the Tax Relief and Health Care Act. In 2008, the Medicare Improvements for Patients and Providers Act established the PQRS as a permanent federal program. It also increased the incentive payment to 2% of the total allowed charges for PFS-covered professional services in 2008 and 2009.
The Affordable Care Act, signed into law by President Obama in 2010, made several changes to the PQRS program. These changes included a gradual decrease in the incentive payment, requiring that quality measures eventually be met to receive the maximum Medicare payment for services. In 2011, the program decreased the incentive payment to 1% of the total allowed charges for PFS-covered professional services. The incentive will be further decreased to 0.5% in 2012 through 2014 and will eventually become a penalty starting in 2015 if not met. The expected starting penalty is a 1.5% reduction in the total allowed charges for PFS-covered professional services. In 2016, there will be further reduction to 2% in payment for services if the reporting measures are not met.
Quality Performance Measures
The PQRS program consists of more than 200 quality measures for Medicare patients including various aspects of care, such as prevention, chronic and acute care management, procedure-related care, resource use, and care coordination. Fifteen of these quality measures are applicable to diagnostic radiology, interventional radiology, or nuclear medicine as shown in Table 1 .
| Category | Measure No | Title |
|---|---|---|
| Stroke and stroke rehabilitation | 10 | CT or MR imaging reports |
| Perioperative care | 20 | Timing of antibiotic prophylaxis, ordering physician |
| Perioperative care | 21 | Selection of prophylactic antibiotic, first or second-generation cephalosporin |
| Perioperative care | 22 | Discontinuation of prophylactic antibiotics (noncardiac procedures) |
| Perioperative care | 23 | Venous thromboembolism prophylaxis (when indicated in all patients) |
| Prevention of catheter-related bloodstream infections | 76 | Central venous catheter insertion protocol |
| Health information technology | 124 | Adoption/use of electronic health records |
| Medication reconciliation | 130 | Documentation of current medications in the medical record |
| Radiology | 145 | Exposure time reported for procedures using fluoroscopy |
| Radiology | 146 | Inappropriate use of “probably benign” assessment category in mammography screening |
| Nuclear medicine | 147 | Correlation with existing imaging studies for all patients undergoing bone scintigraphy |
| Preventive care and screening | 173 | Unhealthy alcohol use, screening |
| Radiology | 195 | Stenosis measurement in carotid imaging reports |
| Radiology | 225 | Reminder system for mammograms |
| Preventive care and screening | 226 | Tobacco use: screening and cessation intervention |
The following three measures are applicable to most neuroradiologists in practice :
- 1.
Measure 10—Stroke and Stroke Rehabilitation: CT or MR Imaging Reports refers to the percentage of finalized reports for CT or MR imaging studies within 24 hours of arrival to the hospital for patients aged 18 years and older with either a diagnosis of ischemic stroke or transient ischemic attack or intracranial hemorrhage or at least one documented symptom consistent with ischemic stroke or transient ischemic attack or intracranial hemorrhage that include documentation of the presence or absence of each of the following: (1) hemorrhage, (2) mass lesion, and (3) acute infarction.
- 2.
Measure 195—Stenosis Measurement in Carotid Imaging Reports refers to the percentage of final reports for all patients, regardless of age, for carotid imaging studies (including neck MR angiography, neck CT angiography, carotid duplex sonography, and carotid angiography) performed that include direct or indirect reference to measurements of the distal internal carotid artery diameter as the denominator for the stenosis measurement.
- 3.
Measure 145—Radiology Exposure Time Reported for Procedures Using Fluoroscopy refers to the percentage of final reports for procedures using fluoroscopy that include documentation of the radiation exposure or exposure time.
Program Requirements
The PQRS is a voluntary incentive program. Submission of quality data codes through claims or a qualified registry indicates the intent to participate. In claims-based individual reporting, each eligible physician must report a minimum of three measures if applicable to his or her practice. There must be 50% compliance in a minimum of three measures to qualify for the incentive payment. However, if an eligible physician has less than three measures applicable to their practice, they are still able to participate in the program reporting on only their applicable measures. If fewer than three measures are reported, CMS may apply a measure-applicability validation process to determine eligibility for the incentive payment.
CMS uses two methods for assessing conformity to the requirements, referred to as “reporting compliance” and “quality compliance.” Reporting compliance reflects the percentage of eligible cases that have a PQRS code assigned. The incentive plan is based on obtaining reporting compliance. The physician performance data are published on-line as a list of the eligible professionals who satisfactorily report PQRS measures since 2009. Quality compliance refers to the percentage of reported cases that have completed the quality measure. Currently, quality compliance data are collected and monitored by CMS. Compliance is measured as a ratio: “denominator” refers to all eligible cases for a particular measure in your practice, and “numerator” refers to successful reporting of the measure.
The beginning of this year’s cycle is January 1, 2012. However, you can start participating in the program during the mid-year cycle. Fig. 1 demonstrates five main steps to getting started.