TERMINOLOGY
Abbreviations
- •
Internal jugular vein (IJV)
- •
External jugular vein (EJV)
- •
Retromandibular vein (RMV)
GROSS ANATOMY
Overview
- •
Major extracranial venous system composed of facial veins, neck veins, scalp, skull (diploic), and orbital veins
- •
Facial veins
- ○
Facial vein
- –
Begins at angle between eye, nose
- –
Descends across masseter, curves around mandible
- –
Joins IJV at hyoid level
- –
Tributaries from orbit (supraorbital, superior ophthalmic veins), lips, jaw, facial muscles
- –
- ○
Deep facial vein
- –
Receives tributaries from deep face, connects facial vein with pterygoid plexus
- –
- ○
Pterygoid plexus
- –
Network of vascular channels in masticator space between temporalis/lateral pterygoid muscles
- –
Connects cavernous sinuses and clival venous plexus to face/orbit tributaries
- –
Drains into maxillary vein
- –
- ○
RMV
- –
Formed from union of maxillary and superficial temporal veins
- –
Lies within parotid space
- –
Passes between external carotid artery (ECA) and CNVII to empty into IJV
- –
- ○
- •
Neck veins
- ○
EJV
- –
From union of retromandibular and posterior auricular veins
- –
Courses inferiorly on surface of sternocleidomastoid muscle
- –
Drains into subclavian vein in supraclavicular fossa
- –
Receives tributaries from scalp, ear, and face
- –
Size, extent highly variable
- –
- ○
IJV
- –
Caudal continuation of sigmoid sinus from jugular foramen at skull base
- –
Jugular bulb = dilatation at origin
- –
Courses inferiorly in carotid space posterolateral to internal/common carotid arteries underneath sternocleidomastoid muscle
- –
Unites with subclavian vein to form brachiocephalic vein
- –
Size highly variable; significant side-to-side asymmetry common; right usually larger than left
- –
- ○
Subclavian vein
- –
Proximal continuation of axillary vein in thoracic inlet
- –
EJV drains into subclavian vein
- –
Subclavian vein joins IJV to form brachiocephalic vein
- –
- ○
Vertebral venous plexus
- –
Suboccipital venous plexus
- –
Tributaries from basilar plexus, cervical musculature
- –
Interconnects with sigmoid sinuses, cervical epidural venous plexus
- –
Terminates in brachiocephalic vein
- –
- ○
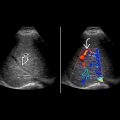
IMAGING ANATOMY
Overview
- •
Low pressure inside; easily compressible
- ○
Light probe pressure with good surface contact between transducer and skin to ensure optimal visualization
- ○
Valsalva maneuver helps to distend major neck veins
- ○
- •
IJV
- ○
Largest vein of neck
- ○
Deep cervical chain lymph nodes commonly found along its course
- ○
Beware of thrombosis in patients with previous central venous catheterization or adjacent tumors
- ○
Always check for compressibility and phasicity on respiration
- ○
Vascularity in IJV thrombosis usually seen with tumor thrombus rather than bland venous thrombus
- ○
- •
Subclavian vein
- ○
Accessible on US by inferior tilting of transducer in supraclavicular fossa
- ○
Venous valves present in most patients
- ○
Thrombosis/stenosis commonly seen in patients on chronic hemodialysis or with previous subclavian venous catheterization
- ○
- •
RMV
- ○
Serves as landmark on US to infer position of intraparotid portion of facial nerve
- ○
Anterior division of RMV sandwiched between submandibular gland anteriorly and parotid tail posteriorly
- –
Its displacement helps to determine origin of mass in posterior submandibular region
- –
- ○
ANATOMY IMAGING ISSUES
Imaging Pitfalls
- •
Neck veins often overlooked as most sonologists pay more attention to arteries than veins in neck
- •
Not all neck veins readily assessed by US
- ○
Only large and superficial veins clearly seen
- ○
- •
Asymmetric IJVs common; 1 IJV may be many times the size of contralateral IJV
- ○
IJV venous varix: Extreme dilatation of IJV upon Valsalva maneuver with clinically palpable neck lump
- ○
- •
Slow flow within IJV may appear as low-level, hyperechoic intraluminal “mass”
- ○
May mimic IJV thrombus
- ○
Moving nature of echoes on real-time US and sharp linear near-field interface help to distinguish artifacts from slow flow and IJV thrombus
- ○
CLINICAL IMPLICATIONS
Clinical Importance
- •
US safely guides needle for venous access
- •
Absence of respiratory phasicity is strong indicator of abnormality
GRAPHIC