9 Neurogenic and Metabolic Bone Diseases
Neurogenic Osteoarthropathy
Definition
 Severe destructive atrophic/hypertrophic arthropathy
Severe destructive atrophic/hypertrophic arthropathy
Pathology
 Increased osteoclastic resorption due to increased blood flow to the subchondral region, caused by neurogenic dysfunction
Increased osteoclastic resorption due to increased blood flow to the subchondral region, caused by neurogenic dysfunction
Causes
 Frequent:
Frequent:
– Syringomyelia
 Rare:
Rare:
– Spinal trauma
– Diabetes mellitus
– Tabes dorsalis
– Amyloidosis
– Disseminated encephalitis
– Myelomeningocele
– Alcoholism
– Intra-articular corticosteroid injection
Clinical Findings
 Depends on underlying condition
Depends on underlying condition
 Joint swelling (with or without pain)
Joint swelling (with or without pain)
 Joint hypermobility (instability)
Joint hypermobility (instability)
Diagnostic Evaluation
 (→ Method of choice)(Fig. 9.1)
(→ Method of choice)(Fig. 9.1)
Recommended views
 Anteroposterior (AP)
Anteroposterior (AP)
 Axial
Axial
Findings
 Increased sclerosis
Increased sclerosis
 Effusion
Effusion
 Fragmentation
Fragmentation
 Joint destruction
Joint destruction
 Dislocation/subluxation
Dislocation/subluxation
 No juxta-articular osteoporosis
No juxta-articular osteoporosis
 (→ Supplementary method)
(→ Supplementary method)
Indications
 In the early stage, detection of effusion (not diagnostic)
In the early stage, detection of effusion (not diagnostic)
 (→ Supplementary method)
(→ Supplementary method)
 Evaluation of underlying disease (e.g., syringomyelia, myelomeningocele)
Evaluation of underlying disease (e.g., syringomyelia, myelomeningocele)
 Differential diagnosis:
Differential diagnosis:
– Atrophic type: septic joint
– Hypertrophic type: massive osteoarthritis
Goals of Imaging
 Seventy of joint destruction
Seventy of joint destruction
 Differentiation from other diseases (causes)
Differentiation from other diseases (causes)
 Extra-articular manifestations?
Extra-articular manifestations?
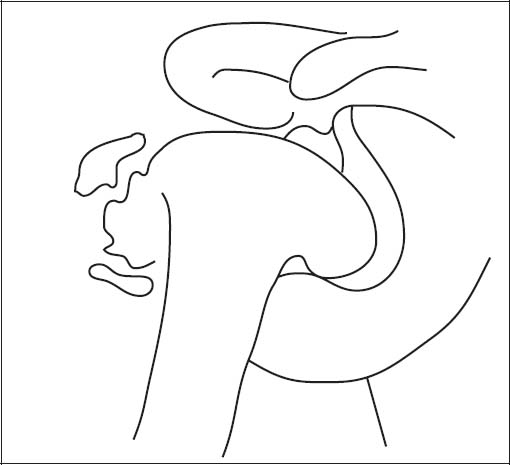
Fig. 9.1  Neurogenic osteoarthropathy (Charcot joint)
Neurogenic osteoarthropathy (Charcot joint)
Massive deformity of the joint-forming bones with numerous osteochondral fragments (advanced stage of the disease).
Therapeutic Principles
 Therapy of underlying condition
Therapy of underlying condition
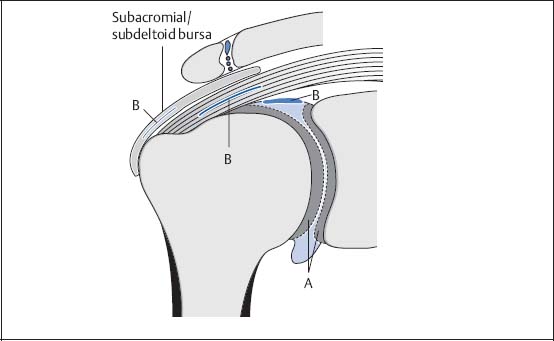
Fig. 9.2  CPPD crystal arthropathy
CPPD crystal arthropathy
A | Chondrocalcinosis with punctate superficial calcifications of the articular cartilage and small calcifications in the disk of the AC joint. |
B | Delicate stripe-like calcifications in the joint capsule and/or supraspinatus tendon and/or subacromial/subdeltoid bursa. |

Fig. 9.3  CPPD crystal arthropathy, conventional radiograph
CPPD crystal arthropathy, conventional radiograph
A Delicate linear calcification at the insertion of the supraspinatus tendon.
Calcium Pyrophosphate Dihydrate Crystal Arthropathy
Definition
 A joint disease caused by calcium pyrophosphate dihydrate (CPPD) crystal deposition, usually multiarticular and symmetrical
A joint disease caused by calcium pyrophosphate dihydrate (CPPD) crystal deposition, usually multiarticular and symmetrical
 Occurs in middle and old age, no gender preference
Occurs in middle and old age, no gender preference
Pathology
 Numerous, also larger cystic lesions
Numerous, also larger cystic lesions
 Severe progressive bone destruction
Severe progressive bone destruction
 No erosions
No erosions
 CPPD deposition in:
CPPD deposition in:
– Cartilage (chondrocalcinosis)
– Synovia and synovial fluid
– Joint capsule
– Tendons, primarily the supraspinatus tendon
– Subacromial/subdeltoid bursa
– Ligaments
Clinical Findings
 Ranging from asymptomatic to symptoms of acute arthritis or chronic progressive arthritis with acute pain attacks
Ranging from asymptomatic to symptoms of acute arthritis or chronic progressive arthritis with acute pain attacks
Diagnostic Evaluation
 (→ Method of choice)
(→ Method of choice)
Recommended views
 AP
AP
 Axial
Axial
 High-resolution film
High-resolution film
 Punctate calcifications in hyaline cartilage and/or in the disk of the acromioclavicular (AC) joint in chondrocalcinosis
Punctate calcifications in hyaline cartilage and/or in the disk of the acromioclavicular (AC) joint in chondrocalcinosis
 Linear calcifications in joint capsule, supraspinatus tendon, and subacromial bursa
Linear calcifications in joint capsule, supraspinatus tendon, and subacromial bursa
 In pyrophosphate arthropathy, numerous, also larger cysts to severe destructive arthropathy, with or without chondrocalcinosis and soft-tissue calcifications
In pyrophosphate arthropathy, numerous, also larger cysts to severe destructive arthropathy, with or without chondrocalcinosis and soft-tissue calcifications
 (→ Supplementary method)
(→ Supplementary method)
Findings
 Localization of calcifications in the supraspinatus tendon or bursa
Localization of calcifications in the supraspinatus tendon or bursa
 Determination of tendon degeneration or tear
Determination of tendon degeneration or tear
 Bursal fluid
Bursal fluid
 (→ Supplementary method) (Fig. 9.4a, b)
(→ Supplementary method) (Fig. 9.4a, b)
Indications
 Documenting the extent of the synovitis and the therapeutic response
Documenting the extent of the synovitis and the therapeutic response
 Visualization of the extent of cartilage and bone destruction
Visualization of the extent of cartilage and bone destruction
Recommended sections
 Paracoronal
Paracoronal
 Parasagittal
Parasagittal
 Axial
Axial
Recommended sequences
 T1-weighted spin-echo (SE)
T1-weighted spin-echo (SE)
 Short time inversion recovery (STIR)
Short time inversion recovery (STIR)
 Intravenous injection of Gd-DTPA
Intravenous injection of Gd-DTPA
Findings
 Synovial thickening with strong enhancement on T1 weighting after administration of Gd-DTPA
Synovial thickening with strong enhancement on T1 weighting after administration of Gd-DTPA
 Hyperintense effusion in bursa and joint on STIR sequence
Hyperintense effusion in bursa and joint on STIR sequence
 Calcifications signal void on all sequences
Calcifications signal void on all sequences
 Degenerative changes in the supraspinatus tendon hyperintense on all sequences
Degenerative changes in the supraspinatus tendon hyperintense on all sequences
 Defects in hyaline articular cartilage
Defects in hyaline articular cartilage
 Subchondral cysts hypointense on T1 weighting and hyperintense on STIR sequence
Subchondral cysts hypointense on T1 weighting and hyperintense on STIR sequence
Goals of Imaging
 Localization of calcifications
Localization of calcifications
 Detection of cystic and destructive bone changes
Detection of cystic and destructive bone changes
Therapeutic Principles
Conservative
 Nonsteroidal anti-inflammatory drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs)
 Colchicine
Colchicine
 Intra-articular corticosteroids
Intra-articular corticosteroids
Surgical
 Arthroplasty in severe destructive arthropathy
Arthroplasty in severe destructive arthropathy

Fig. 9.4 a  CPPD crystal arthropathy, paracoronal section, T1-weighted SE sequence
CPPD crystal arthropathy, paracoronal section, T1-weighted SE sequence
A | Supraspinatus tendon showing altered signal with hyperintense areas and thickening at the insertion. |
B | On the bursa-facing surface of the supraspinatus tendon, a small signal-void area consistent with a calcification. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


