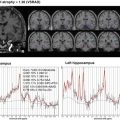
Fig. 12.1
A comparison of z-scores between AD and DLB using VSRAD
Among subcortical structures, atrophy of the substantia innominata (including the nucleus basalis of Meynert) [11] and dorsal midbrain [12] has been documented in DLB. Atrophy of these structures is supported by the pathological involvement of the areas. Atrophy of the substantia innominata is associated with cholinergic dysfunction in DLB. However, it remains unclear whether these subcortical structural changes are diagnostic markers for the identification of DLB and its differentiation from AD.
12.3 Perfusion SPECT
Perfusion SPECT studies are currently being employed in practice to differentiate between various types of dementia, as this method can reveal perfusion abnormalities that may be characteristic of different types of dementia [13]. Although the neuropathologic and neurochemical bases underlying occipital abnormalities in DLB are not yet clearly understood, functional brain imaging studies using SPECT and PET have revealed that reduced occipital metabolism and perfusion are characteristic features of DLB (Fig. 12.2). Several investigators have indicated the value of functional brain imaging studies in differentiating between DLB and AD, although there are some methodological differences, including patient selection (definite or probable cases), scanning methods (PET versus SPECT), and image analysis (conventional region of interest or statistical image analysis). In a multicenter study examining [18F]fluorodeoxyglucose (FDG) PET measures, the presence of hypometabolism in the occipital lobe discriminated DLB from AD with a sensitivity of 71% and a specificity of 95% [14]. On the other hand, the diagnostic accuracy of SPECT is relatively low, as shown by a sensitivity range of 65–85% and a specificity range of 85–87% [5]. We found that combined MMSE and perfusion SPECT studies achieved a high discrimination between DLB and AD with a sensitivity of 81% and a specificity of 85% [15].


Fig. 12.2
Z-score images of AD and DLB on perfusion SPECT (3D-SSP)
Lim et al. [16] confirmed that occipital hypometabolism and relative preservation of the posterior cingulate gyrus (cingulate island sign) differentiated DLB from AD in patients with a sensitivity of 77% and a specificity of 80%. In addition to occipital hypoperfusion, increased perfusion in the deep gray matter (striatum and thalamus) was shown to be a characteristic feature of DLB, possibly due to compensatory changes to decreased dopaminergic input to the basal ganglia [17] (Fig. 12.3). These additional alterations on functional brain imaging may enhance the diagnostic accuracy of DLB.


Fig. 12.3
Two-tail views of AD and DLB on perfusion SPECT
Psychotic symptom clusters in DLB appear to relate to spatially distinct perfusion deficits. Nagahama et al. [18] found that visual hallucinations concord with parietal and occipital association cortices perfusion deficits and delusional misidentifications to perfusion deficits of the limbic-paralimbic structures. Increased thalamic and decreased inferior occipital perfusion may be related to fluctuations in consciousness [19].
12.4 MIBG Myocardial Scintigraphy
MIBG myocardial scintigraphy is a useful, noninvasive technique for estimating local myocardial sympathetic nerve damage not only in primary heart disease but also in synucleinopathies, such as PD, DLB, and REM sleep behavior disorder (RBD) (Fig. 12.4). MIBG scintigraphy has been performed mainly on Japanese cohorts. A number of studies have shown reduced MIBG uptake (heart-to-mediastinum ratio) in DLB patients compared with AD and normal controls. A review from Sinha et al. [5] showed that MIBG myocardial scintigraphy yielded a high sensitivity (range, 83–100%) and a high specificity (range, 82–100%) for diagnosing DLB. MIBG scintigraphy was more sensitive in detecting DLB than occipital hypoperfusion on SPECT [20]. We investigated the role of MIBG scintigraphy in the differential diagnosis of dementia in 96 dementia patients in our Memory Clinic, including 32 with DLB, 9 with PDD, 40 with AD, and 24 with other types of dementia. The overall sensitivity to positively identify patients with Lewy body disease (including DLB and PDD) was 95%, and the specificity to differentiate them from patients with other types of dementia was 87% [21] (Fig. 12.5). There was no correlation between MIBG scintigraphy and disease severity or duration of DLB. Although it is important to note that reduced MIBG uptake has also been reported in patients with cardiac disorders, diabetes mellitus, and some medications, this technique is also a powerful tool in the differential diagnosis between DLB/PDD and other types of dementia.



Fig. 12.4
MIBG myocardial scintigraphy

Fig. 12.5
Diagnostic accuracy for DLB and PDD using MIBG myocardial scintigraphy
12.5 Dopamine Transporter (DAT) Imaging
Imaging with specific SPECT ligands for dopamine transporter (FP-CIT and beta-CIT) provides a marker for presynaptic nigrostriatal degeneration. DAT scan has been clinically available for patients with DLB and PD in Japan since 2014. DAT imaging is abnormal in PD and DLB, reflecting nigrostriatal degeneration, but not in AD, indicating a useful method in the differentiation between DLB and AD. In our preclinical study of DAT imaging, a 4.1 cutoff score of specific binding ratio yielded a sensitivity of 92% and a specificity of 84% for diagnosing probable DLB from AD (Fig. 12.6). A large multicenter study demonstrated a sensitivity and specificity of abnormal DAT scans in diagnosing probable DLB from AD of 78% and 90%, respectively [22]. DAT imaging results were in agreement with autopsy diagnosis in the vast majority of cases (7 of 8 DLB and 12 of 12 non-DLB) and were more precise than clinical diagnosis [23]. FP-CIT SPECT is also reliable in confirming cases of clinically possible DLB, supporting the inclusion of reduced DAT uptake as a suggestive feature of DLB in the International Consensus Criteria [24].


Fig. 12.6
DAT imaging
DAT imaging has demonstrated superior diagnostic accuracy for DLB compared with brain perfusion SPECT and FDG-PET. A recent clinical study has revealed that DAT imaging and MIBG scintigraphy showed similar diagnostic accuracy in differential diagnosis between DLB and other dementias [25]. However, DAT imaging fails to discriminate PD/DLB from other parkinsonian syndromes because reduced striatal dopamine uptake has been shown in progressive supranuclear palsy, multiple system atrophy, and corticobasal syndrome. The impact of concurrent vascular pathology in striatal DAT binding has not yet been determined. Despite the caveat and the limited diagnostic potential to differentiate between different synucleinopathies, the European Federation of Neurological Societies (EFNS) guidelines also recommend the use of DAT scan to differentiate between DLB and AD as the only imaging test to reach the level A category of evidence [26].
12.6 Structural and Functional Changes in Idiopathic RBD (iRBD)
RBD is a type of parasomnia characterized by a loss of normal skeletal muscle atonia during REM sleep and prominent motor activity while dreaming. RBD occurs either as an idiopathic disease or in association with neurodegenerative diseases, particularly alpha-synucleinopathies. Recent studies have demonstrated several neuropsychological impairments in iRBD patients, such as visuospatial construction dysfunction, executive dysfunction, memory disturbance, smell testing abnormalities, reduction of striatal presynaptic dopamine transporters, and reduced MIBG uptake. Since these findings are characteristic features of alpha-synucleinopathies, including PD and DLB, iRBD may be a prodromal stage of alpha-synucleinopathies.
There have been few studies examining structural and functional brain changes in iRBD patients. We investigated structural brain changes using voxel-based MRI morphometry in iRBD patients. Compared with the 18 age-matched controls, 20 iRBD patients had significant gray matter volume reduction in the anterior lobes of the right and left cerebellum, tegmental portion of the pons, and left parahippocampal gyrus [27]. Recently, Scherfler et al. [28] showed significant decreases in fractional anisotropy in the tegmentum of the midbrain and rostral pons and increases in mean diffusivity within the pontine reticular formation in iRBD patients. These studies provide in vivo evidence suggesting that structural lesions of the brain stem are responsible for the occurrence of iRBD. In our SPECT study, a decreased perfusion was shown in the parieto-occipital lobe (precuneus), limbic lobe, and cerebellar hemispheres in iRBD patients, as is commonly observed in patients with alpha-synucleinopathies, including DLB and PDD [29] (Fig. 12.7). In addition, a longitudinal study demonstrated more decreased perfusion in the parieto-occipital lobe in the second SPECT than in the first study in iRBD patients [30], although none of the patients showed any neurological deficits, including extrapyramidal and cerebellar signs, visual hallucinations, or neuropsychological impairments, during the study (Fig. 12.8). Therefore, iRBD may be a progressing neurodegenerative disorder, even though neurological and neuropsychiatric impairments have not been shown.