Congenital malformations encompass a diverse group of disorders present at birth as result of genetic abnormalities, infection, errors of morphogenesis, or abnormalities in the intrauterine environment. Congenital disorders affecting the brain and spinal cord are often diagnosed before delivery with the use of prenatal ultrasonography and maternal serum screening. Over the past several decades there have been major advances in the understanding and management of these conditions. This article focuses on the most common spinal congenital malformations.
Congenital malformations encompass a diverse group of disorders present at birth, as result of genetic abnormalities, infection, errors of morphogenesis, or abnormalities in the intrauterine environment. Congenital disorders affecting the brain and spinal cord are now often diagnosed before delivery with the use of prenatal ultrasonography and maternal serum screening. Over the past several decades there have been major advances in the understanding and management of these conditions. This article focuses on the most common spinal congenital malformations, limiting the discussion to the neurosurgically relevant aspects of myelomeningocele, lipomyelomeningocele, and skeletal dysplasias, including achondroplasia, Goldenhar syndrome, Morquio syndrome, spondyloepiphyseal dysplasia (SED), osteogenesis imperfecta (OI), and Larsen syndrome.
Skeletal dysplasias are a heterogeneous group of more than 200 disorders in which there is abnormal formation, growth, or remodeling of cartilage and bone. This group of disorders affects 1 in 5000 live births, differing widely in natural history, inheritance, and etiology. Skeletal dysplasias may be classified as either osteochondral dysplasia (involving the whole skeleton) or dysostosis (involving a single group of bones). Craniocervical junction abnormalities, atlantoaxial subluxation, and kyphoscoliotic deformities are common spinal problems found in skeletal dysplasias. This discussion focuses on the key skeletal dysplasias and their neurosurgical implications in children.
Achondroplasia
Achondroplasia is the most common form of dwarfism and is the most common heritable skeletal dysplasia, characterized by a disproportionate shortening of the proximal limbs relative to the trunk. This is sometimes referred to as rhizomelic dwarfism, describing the small forearms and thighs in relation to the entire limb and trunk. It occurs in 1 of every 28,000 live births. Recognizable at birth, the characteristic morphology includes shortened limbs and long bones, macrocephaly, frontal bossing, genu varum abnormalities, and a low-set nasal bridge. Achondroplasia follows an autosomal dominant inheritance pattern, although 80% of cases arise as a result of spontaneous mutations in the fibroblast growth factor receptor 3 ( FGFR3 ) gene located on chromosome 4. This gene mutation results in a decrease in the rate of endochondral bone formation with normal rates of membranous bone formation, calcification, and remodeling.
Almost half of all children with achondroplasia have neurologic manifestations of their disease. The neurologic manifestations of achondroplasia include ventriculomegaly, compressive spinal syndromes, and developmental delay. Other than ventriculomegaly, foramen magnum stenosis resulting in cervicomedullary compression is the most frequent cause of neurosurgical consultation in infants. In older children and adults, multisegment spinal stenosis involving the subaxial cervical or thoracolumbar spine may also be present. Foramen magnum stenosis results from abnormal endochondral bone growth and fusion of posterior basal synchondroses. The bones of the skull base, as well as bones of the neural arches, normally enlarge by endochondral ossification. Because of defective endochondral bone formation at the cranial base and craniocervical junction, infants with achondroplasia may have a small foramen magnum, a short basicranium and clivus, a shallow posterior fossa with a horizontally oriented inferior occiput, an abnormal odontoid process, stenotic jugular foramina, and a narrow upper cervical canal. Furthermore, premature fusion and abnormal development of the 2 posterior synchondroses contribute to thickening of the rim of the foramen magnum, which may project into the brainstem causing compression and severe angulations of the medulla and rostral cervical spinal cord. The odontoid often projects superiorly and posteriorly into the small foramen magnum causing the anterior medulla to drape over the odontoid. These changes lead to damage of the corticospinal tract and chronic ischemia to the medulla.
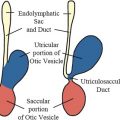
Although foramen magnum stenosis is found in as many as 70% of achondroplasia patients, only between 10% and 35% of patients exhibit symptoms of cervicomedullary compression. Cervicomedullary compression secondary to foramen magnum stenosis can present with dysfunction of the lower brainstem, high cervical spinal cord, and associated nerve roots in children with achondroplasia. Symptoms of cervicomedullary compression may include poor head control, excessive hypotonia, apnea, feeding difficulties, developmental delay, hydrocephalus, myelopathy, respiratory disorders, and sudden death due to respiratory arrest. Less lethal respiratory disturbances in children with achondroplasia include central and obstructive sleep apnea. Central sleep apnea in these children is thought to result from damage to the ventral medullary respiratory control centers from foramen magnum stenosis. Foramen magnum stenosis may also compress lower motor neurons leading to paralysis of the diaphragm and accessory muscles of respiration. Apnea due to foramen magnum stenosis may improve dramatically after surgical decompression. Hydrocephalus in children with achondroplasia is theorized to result from a combination of crowding of the foramen magnum, resulting in obstruction of cerebrospinal fluid (CSF) outflow, and jugular foramen stenosis, resulting in elevated venous sinus pressures. In many instances, the ventriculomegaly found in children with achondroplasia arrests without treatment. Shunt placement can be considered for those who have failed conservative treatment. Even without hydrocephalus, macrocephaly is extremely common in achondroplasia and relative head size should be assessed compared with disease-specific normative data.
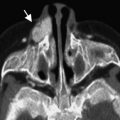
The decision to recommend surgical decompression of foramen magnum and cervical stenosis in achondroplasia patients should be based on both clinical signs and symptoms and imaging data. The clinical signs and symptoms of most concern include lower cranial nerve palsies, apnea, hyperreflexia, clonus, and weakness. Concerning findings on magnetic resonance (MR) imaging include intramedullary T2-weighted changes, absence of CSF signal at the foramen magnum, and the presence of a syrinx. One prospective study of children with achondroplasia concluded that the signs and symptoms that best predicted the need for surgical decompression included central hypopnea, foramen magnum measurements below the mean for children with achondroplasia, lower-extremity hyperreflexia, and clonus. Foramen magnum decompression via a suboccipital craniectomy with removal of the posterior arch of the atlas is performed in cases of proved symptomatic cervicomedullary compression. Even in apparently asymptomatic children, the presence of significant stenosis and T2 signal change in the spinal cord is strongly suggestive of the need for decompression or stabilization. The use of an intraoperative ultrasound to assess for adequate CSF pulsations around the brainstem may assist in determining the degree to which the dura mater should be opened. Marked improvement in neurologic function is often noted in symptomatic children after foramen magnum decompression. Bagley and colleagues reported their single-institution series of 43 children with achondroplasia who underwent foramen magnum decompression. All patients in their series had complete or partial improvement in preoperative symptoms after surgery, in particular respiratory symptoms. Postoperative complications include re-stenosis at the level of the foramen magnum, particularly if the procedure is performed in infancy. If the procedure is performed with a durotomy, additional potential complications include CSF leaks and pseudomeningocele formation.
Subaxial spinal stenosis in children with achondroplasia results from premature fusion of the ossification centers of the vertebral bodies and posterior neural arches. The vertebrae develop a characteristic morphology, including short and thick lamina, vertebral bodies with reduced height, and small neural foramina with a narrowed interpedicular distance. Clinically the most commonly involved areas in order are thoracolumbar, pure lumbar, and cervical. A history of prior need for foramen magnum decompression has been associated with an increased likelihood of symptomatic spinal stenosis before adolescence. Typically, however, stenosis becomes symptomatic in adolescence. Signs and symptoms depend on the level of spinal cord involvement and include ataxia, frequent falls, spasticity, bowel or bladder dysfunction, radiculopathy, temporary deterioration of spinal cord function after minor trauma, paraparesis, or quadriparesis. Surgical treatment usually involves posterior decompression with consideration given to spinal cord fusion if multiple-level laminectomies are required or preoperative spinal instability is present.
Goldenhar syndrome
Goldenhar syndrome, also known as oculoauriculovertebral dysplasia, is a clinically heterogeneous disorder occurring in 1 of every 3000 to 5000 live births in North America. It is characterized by hemifacial microsomia, epibulbar dermoid appendages, and spinal defects. As many as 40% of patients with Goldenhar syndrome may have Klippel-Feil–type fusion anomalies of the spine. Additionally, craniofacial, gastrointestinal, cardiac, renal, and ophthalmic anomalies may be seen. Most cases occur sporadically due to a terminal deletion in the short arm of chromosome 5 and trisomy 7 and 9 mosaicism. This is thought to lead to a disruption in development of the first and second branchial arches as well as in the intervening first pharyngeal pouch and branchial cleft within the first 6 weeks of intrauterine life.
The spinal anomalies associated with Goldenhar syndrome include vertebral hypoplasia, segmentation failure, and failure of vertebral formation. Segmentation defects are more common in the cervical spine, whereas vertebral formation failure more often occurs in the thoracolumbar spine. Unbalanced hemivertebrae and segmentation defects may result in scoliosis or thoracolumbar kyphosis, often requiring surgical treatment. Gibson and colleagues identified vertebral anomalies in 60% of children with Goldenhar syndrome. Among the spinal anomalies identified were block vertebrae (most often involving fusion of C3 and C4), unilateral hemivertebrae in the thoracolumbar spine, spina bifida occulta, butterfly vertebrae, and sacral agenesis. In that series, all patients with scoliosis had an unbalanced hemivertebra. Although several patients required surgical correction of their scoliosis, none of the children in that single-institution series demonstrated any neurologic dysfunction.
Anomalies of the upper cervical spine, including platybasia, occipitalization of the atlas, and odontoid hypoplasia with atlantoaxial instability, have been identified in association with Goldenhar syndrome. One group reported a 12% incidence of platybasia and occipitalization of the atlas. In a series of 8 children with Goldenhar syndrome reported by Healy and colleagues, 3 patients had atlantoaxial subluxation with upward migration of the odontoid process. Two of the patients in that series had atlantoaxial subluxation greater than 7 mm and required occipitocervical fusion. Although atlantoaxial instability may remain clinically silent in children who have not yet reached skeletal maturity, some surgeons advocate treatment in any child with greater than 6 mm of subluxation to reduce the possibility of catastrophic spinal cord impingement. In cases of subluxation less than 6 mm, serial cervical flexion-extension films should be obtained at regular intervals. In addition, due to the high frequency of upper cervical instability, preoperative flexion-extension imaging should be considered in all children with Goldenhar syndrome before undergoing elective endotracheal intubation.
Goldenhar syndrome
Goldenhar syndrome, also known as oculoauriculovertebral dysplasia, is a clinically heterogeneous disorder occurring in 1 of every 3000 to 5000 live births in North America. It is characterized by hemifacial microsomia, epibulbar dermoid appendages, and spinal defects. As many as 40% of patients with Goldenhar syndrome may have Klippel-Feil–type fusion anomalies of the spine. Additionally, craniofacial, gastrointestinal, cardiac, renal, and ophthalmic anomalies may be seen. Most cases occur sporadically due to a terminal deletion in the short arm of chromosome 5 and trisomy 7 and 9 mosaicism. This is thought to lead to a disruption in development of the first and second branchial arches as well as in the intervening first pharyngeal pouch and branchial cleft within the first 6 weeks of intrauterine life.
The spinal anomalies associated with Goldenhar syndrome include vertebral hypoplasia, segmentation failure, and failure of vertebral formation. Segmentation defects are more common in the cervical spine, whereas vertebral formation failure more often occurs in the thoracolumbar spine. Unbalanced hemivertebrae and segmentation defects may result in scoliosis or thoracolumbar kyphosis, often requiring surgical treatment. Gibson and colleagues identified vertebral anomalies in 60% of children with Goldenhar syndrome. Among the spinal anomalies identified were block vertebrae (most often involving fusion of C3 and C4), unilateral hemivertebrae in the thoracolumbar spine, spina bifida occulta, butterfly vertebrae, and sacral agenesis. In that series, all patients with scoliosis had an unbalanced hemivertebra. Although several patients required surgical correction of their scoliosis, none of the children in that single-institution series demonstrated any neurologic dysfunction.
Anomalies of the upper cervical spine, including platybasia, occipitalization of the atlas, and odontoid hypoplasia with atlantoaxial instability, have been identified in association with Goldenhar syndrome. One group reported a 12% incidence of platybasia and occipitalization of the atlas. In a series of 8 children with Goldenhar syndrome reported by Healy and colleagues, 3 patients had atlantoaxial subluxation with upward migration of the odontoid process. Two of the patients in that series had atlantoaxial subluxation greater than 7 mm and required occipitocervical fusion. Although atlantoaxial instability may remain clinically silent in children who have not yet reached skeletal maturity, some surgeons advocate treatment in any child with greater than 6 mm of subluxation to reduce the possibility of catastrophic spinal cord impingement. In cases of subluxation less than 6 mm, serial cervical flexion-extension films should be obtained at regular intervals. In addition, due to the high frequency of upper cervical instability, preoperative flexion-extension imaging should be considered in all children with Goldenhar syndrome before undergoing elective endotracheal intubation.
Spondyloepiphyseal dysplasia
SED encompasses several disorders characterized by flattened vertebral bodies and abnormal epiphyses. Typically, children with SED have short-trunk dwarfism with shortened proximal and middle limbs but relatively normal-sized hands and feet. Epiphyseal abnormalities frequently result in precocious osteoarthritis by the third to fourth decade of life. There are 2 major types of SED: SED congenita and SED tarda. SED congenita is the more severe form of the disorder with recognizable features present at birth. It is commonly associated with delayed ossification of vertebral bodies, coxa vara abnormalities of the hips, and retinal detachment. Wynne-Davies and Hall further classified SED congenita into mild or severe clinical subtypes, with the severe subtype marked by extremely short stature and severe coxa vara.
SED congenita is inherited in an autosomal dominant fashion, with most cases resulting from sporadic mutations in the collagen, type II, alpha 1 chain ( COL2A1 ) gene on chromosome 12. An X-linked recessive form of SED tarda has also been described with similar clinical manifestations. Such mutations result in defective type II collagen, which is the major matrix protein in the nucleus pulposus, epiphyseal cartilage, and vitreous of the eye.
The signs and symptoms of myelopathy due to SED may develop gradually, manifesting as delayed motor development, slowly progressive weakness, spasticity, or sleep apnea. Atlantoaxial instability associated with odontoid hypoplasia or ligamentous laxity is the most common spinal manifestation of SED congenita in children. The incidence of cervical myelopathy due to atlantoaxial subluxation may be as high as 35% in children with SED congenita. In a study of risk factors for myelopathy in patients with SED congenita, Nakamura and colleagues found that atlantoaxial subluxation (defined as an atlantodental interval [ADI] of 5 mm or more in children) was present in most cases with myelopathy. Studies also suggest that atlantoaxial subluxation with increasing ADIs progress with age. The sagittal axis diameter, measured between the posterior edge of the anterior arch of the atlas and the anterior edge of the posterior arch of the atlas, is small in most patients with SED congenita. Those patients in whom sagittal cervical canal diameter at the level of the atlas is 10 mm or less are at increased risk of spinal cord compression, as are patients with the severe subtype of SED congenita. Os odontoideum is frequently present in children with SED and is also associated with a narrowed sagittal axis diameter. In patients with a small sagittal axis diameter and atlantoaxial subluxation, reduction of the subluxation does not ensure an adequate sagittal canal diameter, even in extension. In SED patients, stenosis at the C1 level may be multifactorial such that even with reduction of widened ADI, the canal diameter may still be unacceptably narrow from superimposed C1 stenosis. In these patients, removal of the posterior arch of the atlas in addition to a posterior occipitocervical fusion is recommended to reduce subluxation and to adequately decompress the spinal canal. Preoperative reduction and immobilization in a halo vest may be helpful. Depending on the extent of compression on preoperative imaging, additional procedures, such as a C2 laminoplasty and foramen magnum decompression, may also be required. Perioperative airway management must be tailored to prevent spinal cord injury during induction of anesthesia.
Morquio syndrome
Morquio syndrome or mucopolysaccharidosis type IV (MPS IV) is an autosomal recessive lysosomal storage disease characterized by the inability to metabolize keratan sulfate, a glycosaminoglycan found predominantly in cartilage and in the cornea. There are 2 subtypes of MPS IV: MPS IV type A, which results from a deficiency in N -acetyl-galactosamine-6-sulfatase, and MPS IV type B, which results from a deficiency in β-galactosidase. The clinical manifestations typically become apparent between ages 1 and 3 with marked abnormalities in the skeletal system. Individuals with MPS IV have short-trunk dwarfism with skeletal features that may include barrel chest with pectus carinatum, odontoid hypoplasia, thoracolumbar kyphosis, scoliosis, genus valgus, platyspondyly, flaring of the ribs, and joint hypermobility. Corneal clouding is also common in patients with MPS IV. In contrast to patients with other mucopolysaccharidoses, patients with MPS IV have normal intelligence. Although skeletal abnormalities are present and radiologically evident within the first year of life, patients with MPS IV appear healthy at birth and often have normal growth and development for the first 2 years of life. Clinical and phenotypical abnormalities progress rapidly between 2 and 6 years of age. MPS IV occurs in 1 in 40,000 live births, and although patients may survive to adulthood, many patients die in early adulthood, from either cardiopulmonary disease or neurologic complications of their disorder.
As in SED congenita, a common and serious condition associated with MPS IV is atlantoaxial subluxation with spinal cord compression. Odontoid dysplasia—which can include hypoplasia, aplasia, or os odontoideum—is often present in MPS IV, as is ligament laxity. Both are contributing factors for atlantoaxial subluxation in these patients. In Stevens and colleagues’ series of patients with MPS IV and radiographic atlantoaxial subluxation, odontoid hypoplasia was present in every case. As in patients with SED, primary C1 sinal stenosis can coexist with odontoid and ligamentous abnormalities.
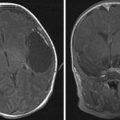
Atlantoaxial subluxation has been identified in up to 42% to 90% of cases of MPS IV. Not all patients with atlantoaxial subluxation have spinal cord compression or require surgery. Symptomatic patients or patients with a 50% reduction in spinal cord diameter, however, should be considered for posterior occipitocervical fusion. The preferred time period for an elective operation is between 3 and 8 years of age, when skeletal anomalies are well developed. Preoperative MR imaging is useful to assess extradural soft tissue elements and the degree of cord compression at the craniocervical junction. In patients who have undergone occipitocervical fusion, postoperative studies of the extradural compressive agents suggest a regression of the extradural soft tissue and ossification of previously unossified cartilage.
Osteogenesis imperfecta
OI is an autosomal dominant congenital disorder characterized by osteopenia, fragile bones susceptible to fracture, variable degrees of short stature, and progressive skeletal deformities. This disease results from mutations in 1 of 2 genes that code for the collagen, type I, alpha chains, COLA1A1 and COL1A2 , localized to chromosomes 17 and 7, respectively. Type I collagen fibers are found in bone, organ capsules, fascia, cornea, sclera, tendon, meninges, and dermis. There are several classification schemes for subtypes of OI; the most common of these categorizes OI into 4 subtypes. Type I is a mild form with no long bone deformities and a normal life expectancy; type II is lethal in the perinatal period with in utero fractures; type III is the most severe form in children who survive the perinatal period; and type IV is associated with moderate bone deformities and variable short stature with a near-normal life expectancy.
Kyphosis and scoliosis are the most common spine manifestations of OI in children. The incidence of scoliosis in OI is reported to be age dependent but as high as 80% in some series. Benson and colleagues found that the incidence of scoliosis is 26% in children younger than 6 years of age and that the incidence of scoliosis rises significantly in children 6 years of age and older. There is a predictable, early progression of scoliotic curves in children with OI. The scoliotic curve in OI usually progresses despite bracing. Brace therapy in severe forms of OI is usually not indicated because of poor therapeutic results and a high complication rate. Furthermore, the ribs of affected patients with OI type III and type IV are too fragile to transmit corrective forces to the spine with bracing, and bracing often causes further deformities of the rib cage that can, in turn, compromise pulmonary function. Early spinal fusion in children with curves less than 40° has been advocated by some to halt or slow progression of spinal deformity and cardiopulmonary dysfunction. Kyphosis, like scoliosis, is often associated with more severe forms of OI.
Patients with OI are at risk for compression fractures and vertebral body collapse. The vertebrae assume a biconcave shape, and microfractures adjacent to vertebral growth plates can interfere with growth and cause deformity. Ishikawa and colleagues found that severe scoliosis (>50°) was likely to develop in prepubescent children with 6 or more biconcave vertebrae. Cyclic intravenous bisphosphonate pamidronate therapy given monthly was found to have beneficial effects on vertebral morphometry in children and adolescents with severe forms of OI. With treatment, there is increased cortical long bone thickness and bone mineral density in the lumbar vertebral bodies, decreased fracture rates, and improved mobility. Moreover, the effect is greatest in vertebral bodies that are more compressed. Early treatment is advocated in children, and pretreatment may improve surgical outcomes for scoliosis.
A rare but potentially serious condition associated with OI is basilar impression due to repetitive microfractures of the base of the skull adjacent to the foramen magnum. Janus and colleagues report a series of 130 children with OI who were found to have basilar impression. None of these children displayed neurologic symptoms. The condition may progress slowly, and it is rare for children with OI to require surgical treatment. Surgery is indicated, however, if there is symptomatic compromise of the spinal cord. If there is significant anterior compression present, an anterior transoral approach for ventral clival-odontoid anterior atlas arch resection followed by posterior stabilization may be required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree