Pulmonary
Gastrointestinal
Genitourinary
Miscellaneous
Atelectasis
Colitis
Urinary tract infection
Malignancy
Pneumonia
Obstruction
Pyelonephritis
Drug reaction
Empyema
Perforated viscus
Renal abscess
Deep vein thrombosis
Pulmonary embolism
Peritonitis
Cystitis
Sinusitis
Cholecystitis
Urethritis
Dural sinus thrombosis
Cholangitis
Prostatitis
Osteomyelitis
Pancreatitis
Gynecological
Discitis
Abscess
Catheter related bloodstream infection
Wound infection
Imaging Techniques
The choice and sequence of initial imaging techniques to investigate suspected abdominal sepsis must largely be tempered by a focused differential diagnosis surmised by a careful history, physical examination, and analysis of the initial laboratory data. Guided by the patient-specific differential diagnosis, an imaging modality is then selected. Four of the five classic “Ws” of post-surgical pyrexia may help guide decision-making:
Wind – Atelectasis (Chest Radiograph)
Wound – Wound infection or post-operative collection (Focused Ultrasound or Contrast enhanced CT)
Water – Urinary tract infection (Urinalysis +/− Renal Ultrasound, followed by CT if still concerned about renal abscess or collection)
Walking – Deep Venous Thrombosis (Lower Extremity Ultrasound)
What Did We Do – Drugs, heating blankets etc. (no imaging available apart from clinician’s eyes and vigilance).
In this day and age much emphasis has been placed on the early utilization of the various cross-sectional imaging modalities (US, CT, MRI). However, the plain film remains a useful initial diagnostic imaging modality. Particularly in intubated and ventilated ICU patients, sepsis of pulmonary origin is high on the list of potential differential diagnoses (see Chap. 24).
Ultrasound is easily performed at the bedside, provides a good overview of common pathologies and can guide the need for further imaging. It is also useful for picking up some of the less common sources of sepsis (Fig. 29.1). Computerized Tomography (CT) remains the preferred imaging modality for intra-abdominal infections in many ICU settings across the world. Various complementary applications can often be employed with the obtained data set, such as 3D volume-rendered reconstructions of various anatomic structures. As the data set is obtained quickly, often in a matter of seconds, it suffers less from motion artifacts commonly seen in MRI or Nuclear Radiology studies. CT can also be utilized for image-guided procedures in addition to diagnostic indications.
Fig. 29.1
Transvaginal grayscale ultrasound image in a 44 year old with fevers demonstrates a large tubular loculated echogenic collection in the right adnexa (blue arrow), which represents a pyosalpinx or a tubo-ovarian abscess. Normally, the fallopian tube is not a well-imaged structure, unless filled with fluid (Hydrosalpinx) or pus (Pyosalpinx) as in this case
Scintigraphic studies are used in extremely rare circumstances in ICU patients. They have a role in cases where other modalities have failed to yield a diagnosis, mainly when looking for an infective focus (Fig. 29.2a, b). These studies are cumbersome and slow and they require the patient to be returned to the Nuclear Medicine Suite on more than one occasion (e.g., delayed Gallium Scan Images at 4 and 24 h to confirm absence of infectious source).
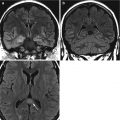
Fig. 29.2
Osteomyelitis/discitis in an iv drug abuser with fevers and leukocytosis of unknown source. The Gallium-67 scan (a) shows the radiotracer accumulating in the T12-L1 region (blue circle). The T1-weighted post-contrast MRI image (b) demonstrates a robust enhancement of the vertebral bodies, disc, and paravertebral soft tissues (blue arrow) consistent with osteomyelitis and discitis
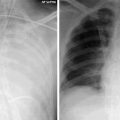
Urinary Tract Infections
They are thought to be the most common overall source of ICU fever and are often catheter-related. It is possible that the incidence of catheter-related urinary tract infections has been overestimated because many studies do not distinguish between asymptomatic bacteriuria and a genuine urinary tract infection. If unrecognized they may progress to pyelonephritis but urosepsis is the ultimate endpoint that needs to be prevented. The diagnosis is typically made clinically in conjunction with laboratory. The role of imaging is typically to exclude more advanced infections of the urinary tract or their complications, such as advanced cystitis, pyonephrosis and both emphysematous and non-emphysematous pyelonephritis. Ultrasound provides the first line test, followed by CT (Fig. 29.3).