Fig. 7.1
Calyceal diverticula. (a) Ultrasound of the kidney demonstrates anechoic lesions (arrows) suggesting cortical cysts. (b) MR pyelographic phase examination confirms the diagnosis of calyceal diverticula (arrows). (c) Calyceal diverticulum containing a calculus (arrow), excised by partial nephrectomy
When echogenic material or posterior wall calcification is identified within a renal cystic lesion, the patient should be scanned in both the supine and prone position to determine whether mobile calculi are present within a calyceal diverticulum.
The demonstration of gravitational change of echogenic content in a cystic lesion located close to renal sinus is diagnostic for calyceal diverticulum on ultrasound.
Computed Tomography
Coronal and sagittal reformatted images can delineate the location of the calyceal diverticulum and its relationship to the collecting system.
Delayed images demonstrate opacification of the entire lesion with a similar density to that of the collecting system, confirming the presence of a calyceal diverticulum (see Fig. 3.8b, c).
Magnetic Resonance Imaging
MRI may be used in circumstances in which the ionizing radiation dose necessitated by CT is undesirable, particularly in pediatric patients, young females, and pregnant patients.
Multi-planar MRI can delineate calyceal diverticula and their infundibulum.
Contrast-enhanced MRI demonstrates contrast filling of cysts on pyelographic phase and confirms the diagnosis of calyceal diverticula (Fig. 7.1b).
Differential Diagnosis
Differential diagnosis includes simple renal cyst, pseudodiverticulum, cortical abscess, and tuberculosis.
Renal cortical and parapelvic cysts mimic calyceal diverticulum, but do not show contrast filling on delayed images.
Pearls and Pitfalls
The demonstration of gravitational change of echogenic content in a cystic lesion located close to the renal sinus is diagnostic for calyceal diverticulum on ultrasound.
Delayed images demonstrate opacification of the entire lesion with a similar density to that of the collecting system, confirming the presence of a calyceal diverticulum.
Most of them are asymptomatic and may contain milk of calcium or renal stone (Fig. 7.1c).
Megacalycosis
General Information
Megacalycosis is accepted as a non-obstructive upper urinary tract lesion in which the calyces are dilated, malformed, and often increased in number.
It is characterized by hypoplasia of the medullary pyramids and calyceal dilatation in the absence of obstruction.
There are an increased number of calyces (12–20 calyces).
Megacalycosis usually occurs unilaterally.
May be associated with congenital megaureter.
Imaging
Intravenous Pyelography
The pyramids have a semilunar configuration, instead of the normal triangular or cone shape.
The tip of each papilla is flat.
The calyces have a rounded appearance.
The corresponding pelvis is normal or only slightly dilated.
IVP may exclude obstruction of collecting system.
Ultrasound
Ultrasound demonstrates dilated calyces with absence of enlargement of the renal pelvis (Fig. 7.2a).
Fig. 7.2
Megacalycosis. (a) Longitudinal sonographic images of the right and left kidney show cystic dilatation of all calyces which are not associated with visible pelvic dilatation. (b) Heavily T2-weighted MR image demonstrates bilateral megacalycosis. (c) MIP reconstructions of dynamic contrast-enhanced images of early (left) and late (right) excretory phases demonstrate contrast filling of calyces and ureters without anatomical obstruction
Computed Tomography
Increased kidney size
Decreased thickness of the renal parenchyma
Ectatic and polygonal calyces
Magnetic Resonance Imaging
T2-weighted images demonstrate dilated calyces with hyperintense signal intensity.
MR urography may exclude anatomical or functional site of obstruction in the urinary tract (Fig. 7.2b, c).
Nuclear Scintigraphy
Diuretic renography may reveal delay in excretion of contrast and lack of obstruction in affected kidney.
Differential Diagnosis
The differential diagnosis includes congenital hydronephrosis, polycalycosis, and hydrocalycosis resulting from infundibular stenosis.
Vesico-ureteric reflux as a cause of the calyceal blunting must be excluded by VCU.
Pearls and Pitfalls
Megacalycosis refers to increase in size of the calyces in the affected kidney.
The calyceal dilatation is not related to obstruction or vesico-ureteric reflux.
Calyceal dilatation associated with normal or small pelvis should alert the physician about the possibility of megacalycosis, which is a non-obstructive pathology.
Ureteropelvic Junction Obstruction
General Information
Ureteropelvic junction (UPJ) obstruction is the most common cause of upper urinary tract obstruction in infants and children.
Although it can be present at any age, 25 % of cases are diagnosed within the first year of life, and 50 % are recognized before the age of 5 years.
The etiology is unclear, but it is believed to be due to functional disturbance of the short segment of the ureteral smooth muscle at the UPJ, restricting urinary flow across this region by interference with ureteral peristalsis.
Anatomical lesions such as bands, adhesions, or aberrant vessels crossing UPJ may also cause obstruction by compressing the ureter or pelvis.
It is more common on the left and affects males more commonly than females (2:1).
It is bilateral in 10–40 % of patients.
Imaging
Intravenous Pyelography
Intravenous pyelographic findings include pelvicalyceal delayed filling and dilatation, abrupt contrast transition at the UPJ, and nonvisualized or normal caliber ureter distal to the UPJ.
Prone position is useful since it promotes filling of the ureter with movement of contrast from calyces to the anteriorly located renal pelvis.
Voiding Cystourethrography
Voiding cystourethrography is important to exclude vesicoureteral reflux, which can also show pelvicalyceal dilatation indistinguishable from other causes of obstruction.
Ultrasound
Most cases are asymptomatic, and the preferred initial imaging modality is ultrasound, both in fetal and in postnatal periods.
On ultrasound, the renal pelvis is enlarged, and the ureter is not dilated.
Dilatation of renal pelvis is best evaluated by measuring the anteroposterior dimension of the renal pelvis in the transverse plane of the kidney.
A renal pelvis diameter of greater than 10 mm is considered abnormal in older children.
Computed Tomography
Crossing renal vessels are frequently associated with UPJ obstruction and usually supply the lower pole of the kidney. Crossing vessels may cause intermittent obstruction, and their presence may influence the type of surgical intervention.
Multi-detector CT scanning with 3-dimensional reconstruction is helpful in establishing the anatomy of the UPJ obstruction and demonstrating intrinsic or high-insertion UPJ.
CT angiography is as accurate as digital subtraction angiography (DSA) in depicting crossing arteries in cases of UPJ.
Magnetic Resonance Imaging
Static T2-weighted sequences allow categorization of the degree of hydronephrosis.
Early angiographic phases, as in CT angiography, clearly identify the vascular abnormalities (Fig. 7.3a, b).
Fig. 7.3
Ureteropelvic junction obstruction. (a) MR urography of a 6-month-old female with UPJ obstruction. T2-weighted image demonstrates a left-sided pelvicalyceal dilatation. (b) An aberrant crossing vessel (arrow) is seen on vascular phase of contrast-enhanced dynamic MRI
Dynamic contrast-enhanced MR urography facilitates individual kidney function assessment (Fig. 7.4a, b).
Fig. 7.4
A 2-year-old boy with left UPJ obstruction. (a) Dynamic contrast-enhanced renograms with furosemide injection are obtained from ROIs placed over the whole kidney. (b) Excretory curves reveal normal findings on the right side (1) with a decline and good washout reflecting contrast material elimination. However, on the left side (2), contrast accumulation and increasing intensity indicate a severe obstruction
Dynamic MR urography allows identification of the peak medullary signal intensity, distal tubular peak, and corticomedullary crossover point to detect deterioration in renal function.
Nuclear Scintigraphy
The most widely used noninvasive functional test to determine the severity of UPJ is diuretic renography.
In cases with UPJ obstruction, renograms will show that T1/2 is longer than 20 min, with little or no washout.
In radioisotope studies, curves of radionuclide uptake can be obtained, and renal transit time (RTT) can also be calculated.
Renal transit time is defined as the time it takes for the contrast agent to pass from the renal cortex to the ureter below the lower pole of the kidney.
Renal transit time in non-obstructed systems is less than 240 s and usually more than 490 s in obstructed systems.
Renal transit times between these values are considered ambiguous; conservative management with close follow-up is usually suggested.
Pathology
Ureteropelvic junction obstruction is the most common cause of ureteral obstruction. This condition can present at any age.
In children, it is more common in boys, more often left side, bilateral in 16 % of cases, and associated with other urologic malformations in 15–20 % of cases.
In adulthood, it is more common in women and is almost always unilateral.
It may appear funnel shaped with an area of distinct narrowing or may be quite stenotic (Fig. 7.5).
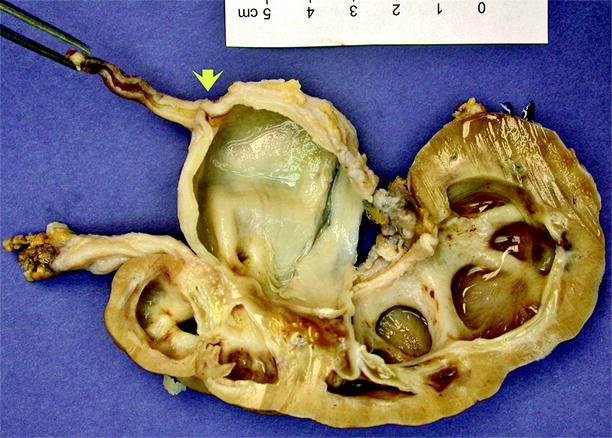
Fig. 7.5
Congenital ureteropelvic junction obstruction. Specimen is a nonfunctioning kidney from an 18-year-old male. The region of obstruction is indicated by the arrow. The renal pelvis and calyces are dilated, and the renal cortex is markedly thinned. Microscopically, the muscle layers in the area of the ureteropelvic junction may be normal, attenuated, disorganized, or predominantly longitudinal. The obstruction may also be extrinsic to the collecting system due to impingement of polar vessels associated with renal malrotation, but this accounts for the minority of cases (Image courtesy of Li Yan Khor, M.D.)
The microscopic findings in this condition are variable: the muscle layers in the area of the ureteropelvic junction may be normal, attenuated, disorganized, or predominantly longitudinal. In a minority of cases, the obstruction is extrinsic to the collecting system due to impingement of polar vessels associated with renal malrotation.
Differential Diagnosis
Differential diagnosis of UPJ obstruction includes multicystic dysplastic kidney (MDK), megacalycosis, and ureterovesical junction obstruction.
In MDK, cysts are of variable size and do not communicate with each other.
In megacalycosis, the renal pelvis is small, and functional studies do not demonstrate physical obstruction.
Dilatation of the ureter distal to the UPJ implies one of three entities: reflux megaureter, obstructed megaureter, or agnogenic megaureter (non-refluxing, non-obstructed megaureter).
Pearls and Pitfalls
Dilatation is best evaluated in the anteroposterior measurement of the renal pelvis in the transverse plane of the kidney.
Dynamic contrast-enhanced MR urography facilitates individual kidney function assessment (Fig. 7.4a, b).
Dynamic MR urography allows identification of the peak medullary signal intensity, distal tubular peak, and corticomedullary crossover point to detect deterioration in renal function.
Megaureter
General Information
Wide ureters can be divided into three categories: (1) reflux megaureter, (2) obstructed megaureter, and (3) agnogenic megaureter.
Reflux megaureter may be primary, that is, of unknown embryologic etiology, or may be secondary to vesical obstruction or neurogenic bladder.
Obstructed megaureter may be primary if it arises from an increase in the connective tissue component (of undetermined etiology) that results in an adynamic distal ureteral segment, or it may be secondary to external obstruction or distal stenosis, as in ureterocele or in an ectopically placed ureteral orifice of the upper pole of a completely duplicated collecting system.
Non-refluxing, non-obstructed megaureter or agnogenic megaureter may be primary if proved neither obstructed nor the result of polyuria, infection, or residual changes after release of obstruction.
Refluxing Megaureter
Refluxing megaureter may be primary or secondary. Vesicoureteral reflux is more common in females, which may be due to the additional mechanical support provided to males by the prostate and seminal vesicles.
In primary reflux, the ureterovesical junction is congenitally abnormal: ureteral tunnel length at the ureterovesical junction is inadequate.
On pathologic examination, the distal ureter may show deficiency of longitudinal muscle fibers in the intramural segment.
Secondary reflux implies anatomic or functional abnormalities of the bladder or urethra.
Obstructed Megaureter
Primary megaureter is a congenital obstruction involving the distal 0.5– 4 cm of the juxtavesical ureter. It is more common on the left side and is bilateral in 20 % of cases. In primary megaureter, the distal ureter is narrow and straight.
The distal ureteral segment in this condition is functionally obstructive.
On pathologic examination, the ureteral wall in the distal segment may exhibit normal muscle, hypoplasia or fibrosis of the smooth muscle, preponderance of circular fibers, or thickening of the periureteral sheath. The dilated ureter above this segment may show smooth muscle hypertrophy or an almost complete absence of muscle. About two-thirds of ureters that have markedly hypoplastic muscle are associated with renal dysplasia.
Secondary obstructed megaureter develops in such settings as neurogenic bladder, ureterocele, ectopically placed ureteral orifice of the upper pole of a completely duplicated collecting system, or obstructing calculus.
Non-refluxing, Non-obstructive Megaureter
It occurs in approximately 6–10 % of infants with antenatal hydronephrosis.
Vesicoureteral reflux is not found in these patents, and ureteral drainage is adequate on functional studies.
Imaging
Intravenous Pyelography
On IVP, the ureter is dilated predominantly in its distal part. Associated pelvicalyceal dilatation can be seen with variable degree.
Voiding Cystouretrography
Voiding cystouretrography (VCU) is the gold-standard examination for detecting vesicoureteral reflux.
Cyclic VCU has been more efficient in diagnosis of reflux. In this technique, two voiding attempts are made when the catheter is in place, and third attempt is made to void after the catheter removal.
Free reflux is demonstrated by voiding cystouretrograms and graded I to V according to the international grading system. Grading system of vesicoureteral reflux is summarized below as:
Grade I: Urine refluxes up into the ureter only.
Grade II: Urine refluxes up into the ureter, renal pelvis, and calyces. The renal pelvis and calyces appear normal.
Grade III: Urine refluxes into the ureter and collecting system. The ureter and pelvis appear mildly dilated, and the calyces are mildly blunted.
Grade IV: Urine refluxes into the ureter and collecting system. The ureter and pelvis appear moderately dilated, and the calyces are moderately blunted.
Grade V: Urine refluxes into the ureter and collecting system. The pelvis is severely dilated, the ureter appears tortuous, and the calyces are severely blunted (Fig. 7.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree