▪
Introduction
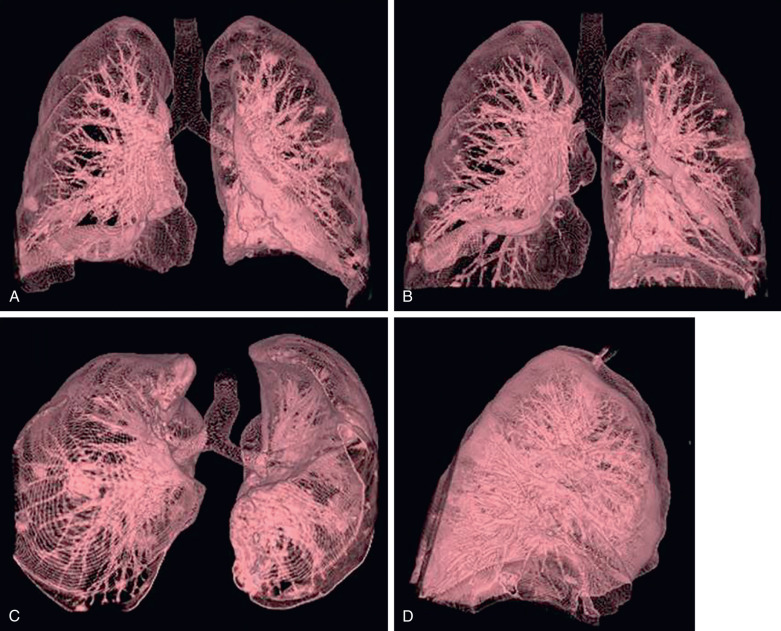
The lungs incorporate the parenchyma, vasculature, bronchial tree (trachea, bronchi, and bronchioles), and a network of investing connective tissue that supports and connects the structures to one another. The human lungs are a pair of large spongy organs for gas exchange between blood and the air. The lungs are covered by a serous membrane called the visceral pleura, and the surrounding cavity formed between the lungs and the surrounding chest wall and mediastinum, covered by parietal pleura, is called the pleural cavity . Understanding diseases of the chest requires the radiologist to have a sound knowledge of the normal lung anatomy. This chapter describes the gross and radiologic anatomy of the lungs. Although imaging with computed tomography (CT) is commonplace, most chest imaging is still done with plain chest radiography.
▪
Surfaces
There are three surfaces of each lung—the costal, mediastinal, and diaphragmatic surfaces. The costal surface is the outer smooth and convex surface, which faces the ribs and the vertebrae. The mediastinal surface abuts the mediastinum. The mediastinal surface of the right lung carries the impression of the right subclavian artery, superior vena cava (SVC), and paratracheal soft tissues, including the esophagus, the azygous vein, the right atrium, and the inferior vena cava (IVC). The left lung carries the impression of the left subclavian artery, thoracic aorta, and the left atrium and ventricle. The diaphragmatic surface, also called the base of the lung, rests on the thoracic diaphragm ( Fig. 1.1 ).
Hilum
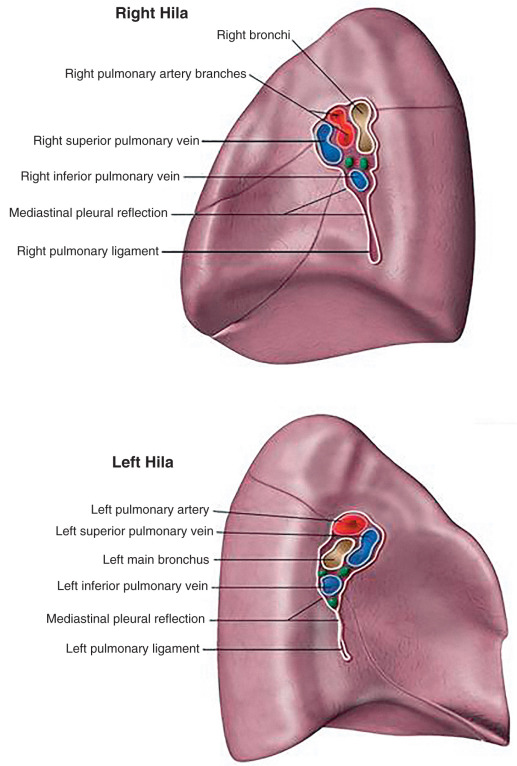
The hilum of the lung (also called the root of the lung ) is formed by the principal bronchi, the central pulmonary arteries and veins, the bronchial nerves and vessels, and the lymphatics, which enter and leave the lung from the mediastinum ( Fig. 1.2 ). The root of the right lung lies behind the SVC, the superior part of the right atrium, and below the azygos vein. The root of left lung lies beneath the aortic arch and in front of the descending aorta.
Lobes
The interlobar fissures are deep clefts in the lungs, lined by visceral pleura, which divide each lung into lobes. The right lung is divided into three lobes—the upper, middle, and lower lobes, separated by two fissures. The oblique fissure (major) separates the lower lobe from the middle and upper lobes; the horizontal fissure (minor) separates the upper from the middle lobe. The left lung is comparatively smaller and has only one oblique fissure, which divides it into two lobes, the upper and the lower. Fissures are frequently incomplete, allowing for collateral air drift and the spread of disease between lobes.
▪
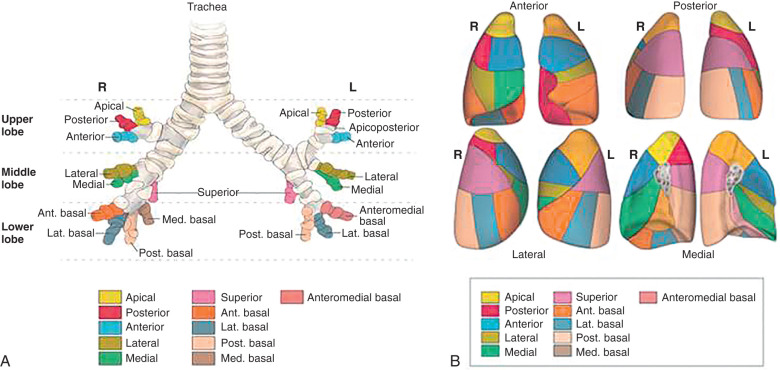
Bronchopulmonary Segments
The bronchopulmonary segment is a smaller division of each lobe, supplied by a tertiary bronchus and its own segmental artery. The significance of such compartmentalization is that each segment is functionally and anatomically discrete, and thus can be removed surgically without affecting the neighboring segments. The veins and lymphatics run along the edges of the segments. There are typically 10 bronchopulmonary segments in the right lung (three, upper lobe; two, middle lobe; five, lower lobe) and eight segments in the left lung (four, upper lobe; four, lower lobe). Table 1.1 lists the typical segmental anatomy ( Fig. 1.3 ). The branching pattern at the segmental level is relatively constant, with the largest variations occurring in the lower lobes. The most common variation occurs in the left lower lobe (LLL), with 4% to 10% of the lobes demonstrating separate origins of the anterior and medial basal segments, similar to the right lower lobe (RLL). On CT, one can define these segments based on the fissures and bronchovascular anatomy. Knowledge of segmental anatomy for the bronchoscopist is important for localization, for the surgeons, because the segments are considered surgical units and can be resected with conservation of adjacent lung, and for the clinician, because many disease processes are segmental in distribution, such as bronchopneumonia, mycobacterial infections, tumor, aspiration, pulmonary infarction, and sequestration.
| RIGHT LUNG | LEFT LUNG |
|---|---|
| Upper Lobe | |
| Apical | Apicoposterior |
| Anterior | Anterior |
| Posterior | Superior segment (lingula) |
| Inferior segment (lingula) | |
| Middle Lobe | |
| Lateral | |
| Medial | |
| Lower Lobe | |
| Superior | Superior |
| Anterior | Anteromedial |
| Medial | |
| Lateral | Lateral |
| Posterior | Posterior |
▪
Pulmonary Interstitium: Skeleton of the Lung
The pulmonary interstitial fibers are a network of connective tissues that provide support to the airways. The pulmonary interstitium is divided into two communicating compartments consisting of the axial or bronchovascular interstitium and the peripheral or subpleural interstitium. The axial interstitium extends from the hilum toward the periphery of the lung and surrounds the bronchovascular bundles. The axial interstitium is contiguous with the centrilobular interstitium, which surrounds the centrilobular arteriole and bronchiole within the secondary pulmonary lobule (SPL). The subpleural or peripheral interstitium lies beneath the visceral pleura and forms the borders of the SPL (interlobular septa). Extending between the centrilobular interstitium of the lobular core and the interlobular septa is a fine network of connective fibers known as the intralobular, parenchymal, or alveolar interstitium ( Fig. 1.4 ). The pulmonary gas exchange units, including the respiratory ducts, alveolar ducts, and alveoli, lie in close relation to the interlobular septa.
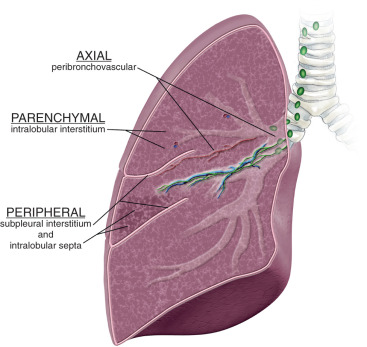
It is important to understand these different networks of interstitial fibers so that one can localize the interstitial disease processes and differentiate and diagnose interstitial lung diseases accurately. On radiographs, the interstitium is not well seen, and the diagnosis of the interstitial lung disease is frequently delayed. On high-resolution CT (HRCT), the interstitium is well seen, both centrally and peripherally. Therefore it is the modality of choice for interstitial lung diseases. The bronchovascular margins are smooth, and one should look for marginal blurring (edema, inflammation, and lymphangiectasia), irregularity (fibrosing conditions), and nodularity (granulomatous conditions and malignancy).
▪
Blood Supply and Bronchovascular Anatomy
The connective tissues, bronchi, and pleura are supplied in a dual fashion, in small part by the pulmonary arteries and veins and to a larger degree by the bronchial arteries and veins. The bronchial arteries arise from the aorta, are variable in number (more on the right side), and accompany the airways. Their branching pattern is similar to the bronchial tree. There is extensive anastomosis between the bronchial and pulmonary arteries under the pleura and adjacent to the small bronchi. They can be enlarged, and many chronic conditions are visible on CT, such as cystic fibrosis, bronchopulmonary aspergillosis, and tuberculosis. The bronchial veins drain via the pulmonary veins to the left atrium and the mediastinal veins, which later join the vena cava. The lymphatics drain the loose connective tissue below the pleura, arising from the interlobular septa and periarterial-peribronchial connective tissue. The lymphatics channel the lymph to the tracheal-bronchial, tracheal, and mediastinal lymph nodes.
▪
Pleura
The pleura is made up of two layers, parietal and visceral. During the embryonic period, the parietal pleura arises from the somatic mesoderm and the visceral pleura from the splanchnic mesoderm. The parietal pleura measures about 0.1 mm; the visceral pleura measures about 0.1 to 0.2 mm. The visceral pleura is adherent to the lung and the parietal pleura to the chest wall. There is a negative pressure within the pleural cavity, which is a space between the parietal and visceral pleura normally containing 10 to 20 mL of a plasma-like fluid. The parietal pleura courses along the cervical, costal, diaphragmatic, and mediastinal lung surfaces and reflects to constitute the costodiaphragmatic and costomediastinal recesses. The parietal pleura is supplied by the intercostal neurovascular bundles. Additional innervation comes from the phrenic nerve. The parietal pleura, in contrast to the visceral pleura, is exquisitely sensitive to the sensation of pain. However, the visceral pleura does receive autonomic innervation from the vagus nerve and is involved in some pulmonary reflexes. The visceral pleura receives blood supply from bronchial arteries, and its drainage is via the pulmonary veins; 25 to 75 mL of pleural fluid is necessary to be detectable on a lateral or decubitus examination, whereas 100 to 200 mL is required for the detection of an effusion on a posteroanterior (PA) radiograph.
▪
Lung Fissures
The major and minor fissures are composed of two adjacent layers of visceral pleura and divide the pulmonary parenchyma into different lobes. Other additional fissures are present. The inferior accessory fissure of the lower lobe is the most common accessory fissure and is present in 40% to 50% of pathologic specimens. The fissures’ depth and extent are variable but complete in 13% of lower lobes. The inferior accessory fissure can infrequently be identified on both the frontal and lateral chest radiographs and is best identified on CT scans, separating the medial basal segment from the other basal segments. With upper lobe collapse or post–upper lobectomy, the lower lobe expands, and the inferior accessory fissure moves laterally. The origin of the fissure adjacent to the diaphragm is frequently accentuated, forming a juxtaphrenic peak ( Fig. 1.5 ). A superior accessory fissure separates the superior segment from the basal segments. The superior accessory fissure is more common on the right than on the left and, when it is seen on the lateral radiograph, the position is posterior to the major fissure, with a slight caudal inclination at or below the minor fissure. Infrequently, a left minor fissure and other accessory fissures of the upper lobes can be identified ( Fig. 1.6 ). The azygos lobe is a normal variant, with an incidence of 0.4% to 1.0%, and is seen as a pleural line that crosses the right lung apex. The azygos vein is contained within this fissure and, although its position is variable within the fissure, it is usually seen in the lowermost aspect as a teardrop-shaped structure. The azygos lobe is formed when the right posterior cardinal vein, the embryologic precursor to the azygos vein, courses through the right upper lobe (RUL) instead of migrating medially. The azygos fissure is unique, except for its less frequent counterpart in the left upper lobe (LUL), in that it contains four layers of pleura instead of the usual two layers of visceral pleura. The inferior pulmonary ligaments contain a double layer of visceral pleura that tethers the mediastinum to the lungs and extends inferiorly from the pulmonary hila to the diaphragm; it may contain systemic vessels, nerves, and lymphatics. On axial CT, the inferior pulmonary ligament is visible in 40% to 70% of the general population. It is seen as a triangular opacity just inferior to the inferior pulmonary veins and is extrapulmonary in location. Thin linear and curvilinear densities are sometimes seen anterior to the inferior pulmonary ligaments and represent pleural reflections over the phrenic nerve ( Fig. 1.7 ).
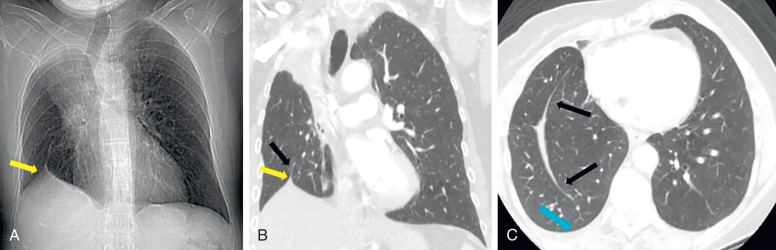


Fissures are best seen on CT because the x-ray beam may not be perpendicular to the fissure on the radiographs ( Fig. 1.8 ). Because the major fissures are oriented obliquely relative to the scan plane, their appearance may vary depending on the slice thickness and effects of volume averaging. An avascular band is associated with the fissures due to the small size of the vessels located in the peripheral lung on either side of the fissure ( Fig. 1.9 ). A few small dots in relation to the fissures or at the pleural surface may be seen in normal subjects, reflecting the presence of subpleural veins or points of intersection of interlobular septa with the pleural surfaces.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree