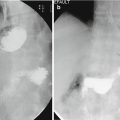
Fig. 4.1
A 5 cm layer of fat does not prevent diagnosis of 12 mm CBD dilatation due to an obstructing 10 mm calculus with posterior acoustic shadowing (white arrow). Note that the detail in the liver parenchyma is poor
A common ultrasound indication is to assess for gallstones. Obese patients are at higher risk of cholelithiasis, and there is also an increased frequency of stone formation following bariatric surgery, particularly Roux-en-Y gastric bypass. Ultrasound remains the best first test for the assessment for gallstone disease [4].
4.2.2.2 Radiography and Fluoroscopy
In radiography , image quality is reduced by photon scatter due to the greater depth of tissue beams that will pass through in obese patients. This effect increases noise in the image and reduces contrast resolution. Using a higher tube voltage reduces scatter but further reduces the contrast resolution. Digital radiography equipment has automated exposure control that may increase exposure time, thereby making images more susceptible to motion artefact. Image quality can be improved by using a smaller field of view to reduce scatter or grids to reduce scatter reaching the image intensifier, but the latter will increase radiation dose.
Fluoroscopy has similar issues, and a higher dose is typically needed to obtain diagnostic quality images. Depending on the quality and age of the equipment, low-dose pulsed fluoroscopy may be unable to provide the clarity of imaging required to make a diagnosis, and full exposures are usually needed to detect complications such as anastomotic leak, particularly where a subtle abnormality is present.
4.2.2.3 CT
CT image quality is also degraded by photon scatter and will potentially result in a decreased signal-to-noise ratio in obese patients resulting in noisier images. However it is usually possible to obtain diagnostic quality images in patients that fit on the scanner. Modern scanners have image acquisition techniques and post-processing which can mitigate the impact of photon starvation. These include maximizing the tube mA and kV settings to increase tube output, with dual source CT scanners providing an obvious additional advantage over single source scanners in this situation, assuming that they have sufficient generator power capacity. Tubes can be allowed to cool completely before scanning the patient to prevent overloading in older machines. Decreased pitch and increased tube rotation time increase the radiation reaching the CT detectors at the expense of higher radiation dose to the patient while increasing reconstructed slice thickness, and the use of post-processing techniques such as iterative reconstruction can reduce noise in the image and improve image quality.
Automated exposure settings applied at image acquisition to reduce image noise can result in a very increased dose to the patient, and the average organ dose to an obese patient is approximately three to four times that of nonobese patients [5]. This can also dramatically increase the acquisition time of the scan because of the lower tube rotation times that are needed, which can lead to image degradation from motion artefact from breathing for example. Dose and image acquisition time can be reduced in this situation by overriding automatic exposure controls and to accept that images may be noisier while still of diagnostic quality. Where automated exposure settings are used, it is essential that the patient is correctly centred within the scanner, since CT exposure and dose reduction techniques can be very dependent on correct patient positioning prior to scanning.
Truncation artefact results from an area being scanned outside the field of view. This leads to incorrect imaging reconstruction calculation producing an imaging artefact, seen as a bright halo around the periphery of the patient obscuring the edge of the images. While reconstruction algorithms can reduce this artefact, it is most important that the region of greatest interest is in the centre of the field of view to reduce the impact of truncation artefact on image quality (Fig. 4.2 a, b). While this usually has little consequence in diagnostic abdominal imaging, it can cause problems when assessing the edge of the patients with stomas and hernias or when performing CT-guided intervention requiring skin markers. In this situation patient repositioning or use of straps to centre the region of interest within the field of view may be beneficial.


Fig. 4.2
(a) Right and (b) left decubitus positions for CT colonography examination in a 220 kg male. The area of interest is in the centre of the field of view. On the edge of the scan field a high attenuation truncation artifact is seen (arrows) which is worse where the gantry is in direct contact with the patient
The optimal CT protocol depends on the clinical question, but in general using intravenous iodinated contrast medium to improve soft tissue contrast will optimize most studies. The dose of contrast medium is ideally calculated by patient weight, but in obese patients this leads to an overestimation of the required dose, since fat is poorly vascularized and hence does not significantly increase the overall blood pool. Estimations of lean body weight provide a better guide to dose, but a standard maximum fixed dose will negate the need for adjustments and may be a better approach [1]. The rate of injection and timing to trigger scans for each phase is the same as nonobese patients and depends on having secured venous access. Renal function assessment with eGFR should also be reviewed before administering iodinated contrast medium to reduce the risk of acute kidney injury.
4.2.2.4 Nuclear Medicine
Radionuclide imaging quality can be reduced in obese patients due to scatter and reduced signal-to-noise ratio. Doses are limited by legislation, but image quality can be improved by lengthening acquisition time. PET-CT is subject to the same limitations as both nuclear medicine and CT with truncation artefacts and reduced signal-to-noise ratio affecting image quality.
4.2.2.5 Magnetic Resonance Imaging
MR image quality is least affected directly by the volume of fat, as soft tissues do not attenuate radiofrequency energy (Fig. 4.3). Image quality will be affected by a reduced signal-to-noise ratio that, due to the larger scanning volume, reduces the radiofrequency signal per voxel of the image. Improved quality of the body surface coils containing an increased number of elements reduces this affect. Decreasing the field of view to increase the signal-to-noise ratio is limited by problems with phase wrapping artefact due to patient size. The key limitation of MRI is the length of acquisition and the need for good patient cooperation to reduce motion artefact when the patient is in a confined space. While open MRI systems are becoming more available, which potentially increases access to obese patients for MRI, these scanners usually operate at lower field strengths (0.5–0.6 T), which limit the imaging that can be performed.


Fig. 4.3
Diagnostic MRI quality with 1.5 T MRI coronal T2 weighted HASTE in a 120 kg patient. A calculus in the common bile duct is clearly demonstrated (arrow)
4.3 The Immediate and Early Postoperative Phase
Imaging in this period usually results from concerns for an early postoperative complication such as anastomotic leak or functional obstruction, to detect a source of infection or bleeding. There is a growing consensus that routine postoperative fluoroscopic imaging following bariatric surgery is not indicated due to the low pretest probability and the low sensitivity for detecting an anastomotic leak in asymptomatic patients [6]. Upper GI fluoroscopy and CT are the most commonly used modalities in this early postoperative period.
4.3.1 Upper GI Fluoroscopy Technical Aspects
Upper GI fluoroscopy studies give real-time information about the functional and anatomical appearances of the postoperative anatomy . Forward planning is important and a discussion with the surgical team should occur before the procedure. Important details to clarify include the exact time since surgery, type of surgery, nature of the anastomoses, lengths of any blind limbs, sites of drains and any intraoperative complications that may have arisen.
In every examination, a set of initial images as control views without any oral contrast medium should be obtained to identify metallic suture lines or surgical drains. This helps the operator to orientate and focus on the area of interest, to select the appropriate field of view and to demonstrate any densities present before contrast administration, which may be confused with a leak, particularly where contrast may have been given for another examination in the recent past. At least two views in different planes should be obtained – most often this will comprise an anterior-posterior and right anterior oblique to give the best views of the upper stomach and gastro-oesophageal junction. We advise that water-soluble iodinated contrast medium is selected to assess for anastomotic leak (Fig. 4.4) for two reasons: barium extravasation from a leak can lead to peritoneal contamination and barium peritonitis, and if a CT scan of the abdomen is subsequently required, then the scatter from retained barium in the bowel lumen can severely degrade image quality.


Fig. 4.4
Early post- Roux-en-Y fluo roscopy study for persistent vomiting on post op day 5, performed with non-ionic iodinated contrast medium, confirmed anastomotic integrity between the gastric pouch (G) and roux limb (R) and prompt gastric emptying. Note normal filling of the short blind limb (B), which should not be confused with a leak
Surgical drains may be present in the early postoperative views and usually placed near to anastomoses. These should be included in the field of view as an early leak may only be demonstrated by contrast medium filling the drain lumen. Oedema around the anastomoses in the early postoperative phase can cause transient obstruction, which will resolve with conservative measures in distinction to an anastomotic stricture.
4.3.2 CT Technical Aspects
Abdominal CT may be performed subsequent to fluoroscopy if there is uncertainty regarding whether a leak may be present, if the patient is showing signs of sepsis or when there is concern of other complications such as bleeding, ischaemia or small bowel obstruction. The CT protocol used depends upon the clinical concern . If there is concern regarding anastomotic leak or intra-abdominal collection , then we routinely administer 8% oral contrast medium, approximately 15–30 min before scanning to test the anastomotic integrity and perform a portal phase scan with intravenous contrast, provided that renal function is adequate. Alternatively, where there is concern about potential bleeding, then positive oral contrast medium should not be used as it may obscure any intra-luminal bleed. We routinely perform a triple phase scan with non-contrast, arterial and portal venous phase acquisition . Bolus tracking is recommended for the arterial phase imaging to optimally opacify arteries.
The postsurgical changes evident on the early postoperative CT depend upon the nature of surgery. Minimal fat stranding in the surgical bed and small traces of free fluid are expected after minimally invasive laparoscopic surgery such as LAGB or RYGB (Fig. 4.5). However the more challenging the surgery, and particularly revision bariatric surgical procedures, the greater the ‘normal range’ of postsurgical changes that may be expected. Important considerations in assessment include the volume of free gas present, which should be minimal in a patient undergoing laparoscopic surgery beyond the second postoperative day, but can persist in larger amounts for a longer period as a normal finding in patients undergoing laparotomy, and the volume of fluid present, which should be minimal in an uncomplicated operation, assuming there are no underlying cardiac or hepatic comorbidities – however, localized low volumes of fluid adjacent to the anastomosis or large volumes of free fluid (and gas) can herald a leak (Fig. 4.6). Extravasation of positive oral contrast is a clear sign of anastomotic disruption .



Fig. 4.5
Post RYGB. Generalized free fluid (F) without pneumoperitoneum, surrounding the spleen and liver. This could represent anastomotic leak (as in this case) or decompensated liver disease as causes depending on the clinical context

Fig. 4.6
Minor fat stranding (thin arrows) around the posterior gastric wall is an expected finding on day 3 post-RYGB. Note the trace of positive oral contrast medium in the roux alimentary limb (J). The fat adjacent to the gastric staple line of the excluded stomach looks clean (large arrow)
The planes surrounding the surgical sutures should be carefully examined for focal free fluid collections and gas, and if there is any concern in the context of sepsis, then positive oral contrast is recommended provided the patient can tolerate this.
4.3.3 Ultrasound Technical Aspects
Definitive exclusion of an intraperitoneal complication in any postoperative patient is very challenging with ultrasound in this obese cohort of patients. If there is a question of superficial abscess associated with surgical wound erythema, ultrasound may be used for exclusion, but ultrasound otherwise seldom plays a role in early postoperative imaging unless there are concerns for gallbladder and biliary pathology.
4.4 The Late Postoperative Phase
After recovery from the initial operation, which can take 6–8 weeks, imaging is most commonly requested to check the function of the postsurgical stomach, and therefore dynamic studies are more often used 30 days beyond the operation.
4.4.1 Fluoroscopy
Fluoroscopy still plays a major role in this stage, to assess the function and postsurgical anatomy [7]. Patients are adjusting to a diet that suits the postsurgical gastric anatomy and may present with symptoms such as discomfort on eating or even vomiting, particularly where they are failing to adjust the volume and consistency of their diet to the new alimentary arrangement. There is little concern for a leak at this stage, and so barium contrast medium can be used safely, particularly in the assessment for luminal stenosis, staple line disruption (producing fistula from gastric pouch to residual stomach in RYGB) and parastomal/perianastomotic ulceration. A normal barium study will reassure patients and focus the management of symptoms towards dietary modification rather than further intervention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree