Hip deformity such as acetabular dysplasia and cam and pincer deformities are thought to be a major cause of hip osteoarthritis. Currently, clinically effective surgical procedures such as pelvic osteotomies and femoral and acetabular osteoplasties are available to correct the underlying deformity. These procedures are most effective in the presence of minimal chondral damage in the joint. Currently, and more so in the future, high-resolution morphologic imaging and biochemical imaging techniques such as Delayed gadolinium-enhanced MR imaging of cartilage, T2, and T1rho will have a clinically important role in diagnosing and staging chondral damage in the hip.
Key Points
- •
Acetabular dysplasia, cam, and pincer deformities are a major cause of premature hip osteoarthritis.
- •
An early feature of osteoarthritis is loss of the negatively charged proteoglycans in the extracellular matrix.
- •
Delayed gadolinium-enhanced MR imaging of cartilage (dGEMRIC) and sodium-imaging techniques are highly specific for assessing cartilage charge density.
- •
T2 and T1rho are noncontrast biochemical imaging techniques that show early cartilage matrix damage in vitro and some clinical studies.
- •
dGEMRIC is clinically useful in staging early osteoarthritis in patients with acetabular dysplasia.
Introduction
Increasingly, hip osteoarthritis is thought to be caused by structural deformities, such as acetabular dysplasia and femoroacetabular impingement (FAI). Acetabular dysplasia results in a shallow acetabulum that leads to hip instability, increased mechanical stress on the acetabular cartilage, and eventual joint degeneration. FAI syndrome is a dynamic mechanical phenomenon of the hip in which the femoral head or neck causes damage to the acetabular labrum and/or cartilage from direct collision between the 2 bony structures. Often the hip is predisposed to FAI syndrome because of a femoral and/or acetabular hip deformity. Currently, surgical techniques such as periacetabular osteotomy, femoral head-neck osteoplasty, and acetabular rim osteoplasty are available to correct the deformities that lead to instability or impingement. The surgical results are limited by the extent of articular damage before surgical intervention. Increasingly, high-resolution MR imaging and biochemical cartilage imaging techniques are becoming clinically important in detecting preradiographic cartilage damage. This article outlines the imaging methods to assess hip structural deformities and methods to assess chondral damage using MR imaging. Imaging is becoming critically important in treating patients with these hip disorders; however, as always, careful clinical-radiographic correlation must be performed to determine if the structural deformity seen on imaging studies is responsible for the patient’s problem and hence justifies surgical intervention.
Introduction
Increasingly, hip osteoarthritis is thought to be caused by structural deformities, such as acetabular dysplasia and femoroacetabular impingement (FAI). Acetabular dysplasia results in a shallow acetabulum that leads to hip instability, increased mechanical stress on the acetabular cartilage, and eventual joint degeneration. FAI syndrome is a dynamic mechanical phenomenon of the hip in which the femoral head or neck causes damage to the acetabular labrum and/or cartilage from direct collision between the 2 bony structures. Often the hip is predisposed to FAI syndrome because of a femoral and/or acetabular hip deformity. Currently, surgical techniques such as periacetabular osteotomy, femoral head-neck osteoplasty, and acetabular rim osteoplasty are available to correct the deformities that lead to instability or impingement. The surgical results are limited by the extent of articular damage before surgical intervention. Increasingly, high-resolution MR imaging and biochemical cartilage imaging techniques are becoming clinically important in detecting preradiographic cartilage damage. This article outlines the imaging methods to assess hip structural deformities and methods to assess chondral damage using MR imaging. Imaging is becoming critically important in treating patients with these hip disorders; however, as always, careful clinical-radiographic correlation must be performed to determine if the structural deformity seen on imaging studies is responsible for the patient’s problem and hence justifies surgical intervention.
Plain radiographic analysis of hip osteoarthritis
Plain radiographic analysis is the main method through which hip structural abnormalities are assessed, and is the gold standard for assessing radiographic osteoarthritis. However, by the time clear evidence of radiographic osteoarthritis is seen, often extensive damage is present in the joint, such that most surgeons would see this as a contraindication for joint-preserving surgery.
Pelvic Radiograph
The anteroposterior pelvic radiograph is used to assess the presence of radiographic osteoarthritis, determine acetabular coverage and orientation, and increasingly determine femoral head-neck offset.
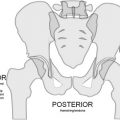
A properly obtained pelvic radiograph should have the coccyx directly over the pubic symphysis, and the iliac wings, obturator foramina, and acetabular tear drops should be symmetric in appearance ( Fig. 1 ). Additionally, if the pelvic inclination is appropriate, the distance between the superior border of the pubic symphysis and the first sacrococcygeal joint should average approximately 32 mm in men and 47 mm in women.
Radiographic osteoarthritis is often graded using the Tönnis classification in hip joint preservation surgery. A more quantitative method of assessing radiographic osteoarthritis is to measure the minimum joint space width (mJSW) of the weight-bearing zone. An mJSW less than 2.5 mm is considered to be definitely pathologic and is associated with poor outcome after FAI surgery. When treating acetabular dysplasia with periacetabular osteotomy, some radiographic osteoarthritis is tolerated as long as the joint space improves and becomes more congruent on abduction internal rotation functional radiographs. However, as a general rule in joint preservation surgery, the presence of Tönnis grade 2 or higher or mJSW less than or equal to 2 mm has been shown to be associated with poor prognosis after surgery.
False Profile Radiograph
For a complete assessment of the acetabular deformity, obtaining a false profile view is recommended ( Fig. 2 ). It is a good view to detect early cartilage loss in the superior weight-bearing zone typically seen in cam impingement and acetabular dysplasia. In cases of pincer impingement, the loss of posterior acetabular cartilage can be seen on the false profile view.
In a normal hip, the superior joint space is larger than the posterior joint space on a false profile view (see Fig. 2 ). When this relationship is reversed, it is a sign of significant cartilage loss in the weight-bearing acetabulum. Additionally, in pincer impingement, the counter-coup damage in the posterior acetabulum will be seen as joint space narrowing in this area, subchondral sclerosis, and cyst formation.
MR imaging
High-resolution MR imaging is widely used to detect the presence of chondral damage associated with FAI and acetabular dysplasia. MR imaging as a cross-sectional imaging modality also allows assessment of proximal femur and acetabulum morphology. Additionally, MR imaging is useful to rule out other causes of hip pain such as femoral neck stress fracture, benign and malignant tumors, and tendinopathy. True acetabular dysplasia is uncommon; however, cam deformity can be present up to 20% of the general population. Hence, a non-FAI cause of hip pain can be mistakenly attributed to the incidentally noted FAI deformity.
To maximally use the MR imaging study, high-resolution dedicated images of the hip are required. Additionally, appropriate sequences are required for accurate detection of the expected intraarticular and nonexpected extra-articular abnormalities.
Chondral Pathology
One of the primary purposes of MR imaging is to detect and stage chondral damage, because the extent of cartilage damage will determine the clinical outcome after surgery. The sensitivity of MR imaging for detecting cartilage damage is highly variable. The reported sensitivities vary from 50% to 90%. The detection of chondral flaps is especially difficult, with one report demonstrating sensitivity of only 23%. This finding is because the femoral and acetabular cartilage layers are in close approximation and hence very little contrast would penetrate into the potential space between the delaminated cartilage and bone. However, MR imaging is useful in identifying cases of minimal radiographic evidence of osteoarthritis but extensive local damage seen on MR imaging. These cases should be excluded from surgical interventions.
Many normal variants in labral and acetabular morphology may be mistaken for labral tears or cartilage defects. The supraacetabular fossa ( Fig. 3 ) is a common (10%) finding on MR arthrograms that may be mistaken for a cartilage defect. The supraacetabular fossa is a distinct structure separate from the acetabular notch that may (8.9%) or may not (1.6%) be filled with cartilage. It is usually located in the acetabular roof near the 12 o’clock position in the coronal and sagittal imaging planes. This appearance is in contrast to the stellate crease that is a continuation of the acetabular notch.
Bony Abnormalities Associated with Chondral Damage
In early osteoarthritis, secondary changes to the bone and labrum may help diagnose early cartilage damage and lend increased specificity to the detection of labral tears. Bony cyst formation in either the acetabulum or femoral head is usually associated with underlying cartilage damage. Additionally, osteophyte formation is a sign of early osteoarthritis.
Screening MR Imaging
A major benefit of MR imaging is its ability to screen for unexpected bony and soft tissue abnormalities. Because FAI deformity is highly prevalent in the asymptomatic population, one cannot assume that the detection of an FAI deformity is always the source of the patient’s symptoms. Having a sequence in the MR protocol designed to detect stress fractures ( Fig. 4 ) and tumors ( Fig. 5 ) is very useful and may potentially help the surgeon avoid catastrophic complications.
Role of biochemical imaging
Biochemical or compositional MR imaging techniques for cartilage hold the promise of detecting cartilage damage before irreversible structural damage occurs. Currently, 5 techniques are designed to probe different macromolecular components of the cartilage matrix. Each technique has its own advantages and challenges to practical clinical application.
Delayed gadolinium enhanced MR imaging of cartilage (dGEMRIC) is a contrast-based technique designed to specifically detect the loss of sulfated glycosaminoglycan content of articular cartilage. The MR imaging is performed after an intravenous or intraarticular injection of an anionic contrast agent chelate, Gd-DTPA 2- . This contrast agent is allowed sufficient time to partition into the cartilage before imaging is started. Because the contrast agent is negatively charged, it will partition into the articular cartilage in an inversely proportional manner. Through quantitating the amount of contrast agent in cartilage using MR imaging, the charge density of cartilage can be calculated or inferred. This technique is highly specific for glycosaminoglycan loss in cartilage, mainly because of the use of a negatively charged contrast agent. However, the need for contrast injection poses challenges, including the need for delay between contrast injection and imaging, need for a specific exercise protocol to facilitate contrast penetration into cartilage, and the risk of contrast reaction. Recently, concern has been raised with the use of contrast agent in patients with poor renal function because of the risk of developing nephrogenic systemic fibrosis, which is a rare and sometimes fatal syndrome. Despite these challenges, if the issues regarding timing of the scan after contrast administration and exercise protocol are respected, reproducible quantitative results can be obtained with root-mean-square average coefficient of variation less than 10%. Additionally, validated fast T1 mapping sequences are available, and therefore imaging times around 5 minutes are now feasible. In addition to the hip studies outlined previously, multiple clinical studies have been performed using dGEMRIC, showing the effect of exercise on knee cartilage, reconstitution of a more normal cartilage after autologous chondrocyte transplantation, and perhaps preservation of cartilage after high tibial osteotomy for knee osteoarthritis.
Currently, the most validated and commonly used technique for the hip is dGEMRIC. dGEMRIC has been validated against histology in vitro and ex vivo and clinically in hips and knees. dGEMRIC index has been shown to correlate with hip pain and degree of hip dysplasia. Similar findings were also seen in patients with FAI, in whom dGEMRIC correlated with pain and alpha angle. Additionally, dGEMRIC mapping of hips with a history of slipped capital femoral epiphysis showed differences between hips with normal and severe offsets. In FAI, comparison of MR imaging against surgical assessment of articular cartilage suggests that morphologic imaging correlates well with surgical findings. dGEMRIC findings did not correlate as well as morphologic MR imaging findings; however, dGEMRIC detected more areas of abnormal cartilage than both gross surgical inspection and morphologic imaging, perhaps suggesting that dGEMRIC is detecting morphologically normal but biochemically abnormal cartilage.
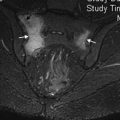
The cartilage matrix will modulate its charge density in response to mechanical loading. Presumably, because the mechanical load distribution in the hip joint is uneven, the charge density and hence the T1 value on 3-dimensional dGEMRIC scans are higher in the superior weight-bearing zone compared with the anterior or posterior aspect of the joint. In disease states such as acetabular dysplasia, the alteration in T1 value with progression of osteoarthritis seems to be much more diffuse throughout the joint than for FAI. Hence, the authors were able to demonstrate even with thick-section coronal slice dGEMRIC scans the predictive value of dGEMRIC in early clinical outcome after periacetabular osteotomy for acetabular dysplasia. In FAI, because the changes seen on dGEMRIC are often focal, normalizing the values at the labral chondral junction against the central dGEMRIC values seem to increase the ability to detect early disease.
Currently, dGEMRIC is used to increase the reliability in detecting chondral lesions in patients with FAI. Sagittal, oblique axial, or radial cuts can be used to confirm areas of chondral damage seen on standard morphologic sequences using the dGEMRIC data in the corresponding region. The authors do not rely solely on the dGEMRIC data in FAI cases but rather use it as additional quantitative data that may assist in the subjective image interpretation. Fig. 6 illustrates an example of a patient with FAI. Radiographs show minimal osteoarthritis, but on the dGEMRIC images the acetabular cartilage at the labral-chondral junction is clearly abnormal, especially compared with the normal femoral head cartilage.